Abstract
Study design: Retrospective outcome measurement study.
Objectives: Patients suffering from malignant tumour disease and metastases to the spine develop a variety of clinical complaints including radicular symptoms and/or spinal cord compression syndromes. Palliative decompressive laminectomy with total or partial tumour resection is an acknowledged method of treatment, despite controversy.
Setting: The Department of Neurosurgery of the University of Vienna.
Method: Patients suffering from metastases with predominant infiltration of the dorsal epidural parts, or patients who could not be operated on via an anterior approach, were included. Eighty-four patients who met these criteria underwent decompressive laminectomy with total or partial tumour removal. The study analyzed motor function, pain relief and continence in a 2- and 4-month post-operative follow-up. According to the criteria of motor performance, 20% of the patients had been mobile pre-operatively.
Results: In the immediate post-operative period 45%, after 2 months 33% and after 4 months 26%, were considered mobile. None of the paraplegic patients showed functional improvement. The median survival time was 6.5 months. Pre-operatively, 56% of the patients had shown continence dysfunction. Post-operatively, 38%, and after 2 months 46% of the patients, developed continence disorders. A significant reduction in analgesic medication was also observed in the post-operative period.
Conclusion: In our series, palliative laminectomy with total or subtotal tumour reduction in patients with malignant spinal metastatic disease resulted in amelioration of motor function, pain and continence and therefore improved the patients' quality of life. The improvement in quality of life shows that this method is a valuable option in neurosurgical therapy, except for cases with pre-operative paraplegia. However, in patients with severe pre-operative paraparesis, the authors recommend laminectomy only in very exceptional cases, because of the poor post-operative neurological results.
Similar content being viewed by others
Introduction
In 5% to 10% of the cases, malignant tumours metastasise to the spine.1,2,3,4,5,6 They stem mostly from primary carcinomas of the prostate, breast, lung, kidney and haematopoietic/reticuloendothelial tissue.1,2,4,5,7,8,9,10
The symptoms typically start with back pain or radicular pain followed by sensory disturbance and motor weakness.7,8,11,12 Transection syndromes are rarely the primary manifestation of disease in the spine. Due to the fact that tumour tissue compromising the spinal canal ventrally cannot be effectively resected from the posterior approach,1,2,3,4,12,13,14,15,16,17 neurosurgical intervention in these cases of spinal metastasis is still a matter of controversy among many authors.2,4,12
The objective of the retrospective study was to demonstrate the mobility, continence, pain and quality of life in our patients, following palliative decompressive laminectomy.
Patients and methods
This study included only patients suffering from metastases with predominant infiltration of the dorsal epidural parts, or patients who could not be operated on via an anterior approach. A follow-up neurological assessment was conducted in 84 patients who met these criteria, 31 of whom were women and 53 were men. The average age of the patients was 60 years (range: 23–82 years). Those patients underwent decompressive laminectomy with total or subtotal tumour resection at the Department of Neurosurgery of the University of Vienna, between 1991 and 1998.
Patients with drop metastasis from CNS-tumours were not included. The study evaluated: patient history, adjuvant pre-/post-operative radiotherapy and/or chemotherapy, pre- and post-operative neurological assessment (immediately afterwards, 2 and 4 months later), concentrating on mortality, pain, urinary and/or faecal incontinence as well as lifespan. The study classified those patients who had been able to walk with or without walking aid pre-operatively, as ambulatory. Patients, who had been dependent on walking aids pre-operatively, were assessed according to their improvement in walking distance. Twenty per cent of all patients included in the study had been mobile pre-operatively. The study classified patients who required less analgesic as having improved. Continence was categorized as being mild, intermediate or severe (permanent catheter). Table 1 shows the pre-operative status of the patients.
Results
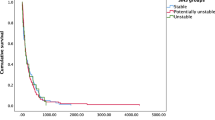
Mobility rose to 45% in the immediate postoperative evaluation, thus showing an improvement of 25%. This rate sank to 33% after 2 months, and to 26% after 4 months. None of the five patients who had been paraplegic pre-operatively, recovered from the paralysis following laminectomy (see Tables 1 and 2). Of the 28 patients who had only been able to slightly flex their knees or toes preoperatively, 22% regained full mobility, and of the 23 patients from group III (straight leg lifting from supination) nine became mobile with walkers and three became mobile without assistance. Twenty per cent of the patients had been mobile pre-operatively, four, despite low-grade paresis, and 15 had required walkers or crutches. All of them were fully mobile in the immediate post-operative period, although only 68% showed significant improvement in mobility and an increase in walking distance. Furthermore, in patients whose only pre-operative symptom was pain, a clear reduction in analgesic consumption was shown post-operatively (see Table 3). However, 55% of the patients with an immediate post-operative decrease in analgesic consumption required an increase in pain-relief medication after 2 and 4 months respectively. Fifteen of the 56% of patients who suffered from urinary retention (see Table 4) needed pre-operative catheterisation.
In total, 18% of the patients included in the study reported an improvement in micturition disturbances, and after 4 months 51% of them still had continence disorders. None of the patients who required preoperative catheterisation, showed improvement.
Adjuvant radiotherapy was conducted either pre- or post-operatively on 45 patients. Forty per cent of the 25 patients, who received adjuvant radiotherapy postoperatively, became mobile for at least 2 months. Of 20 patients, who had received radiotherapy and who had to be operated on because of neurological deterioration, 45% became mobile post-operatively. Thirty-nine patients received no adjuvant radiotherapy. Thirty-six per cent of the patients who had received only surgical therapy became mobile post-operatively.
Eighty per cent of the metastases originated from carcinomas of lung, breast, prostate, kidney and hematopoietic/reticuloendothelial tissue (Table 5 shows the primary tumours and the median post-operative time of survival). Fifty-four per cent of the patients showed isolated and 46% multiple vertebral body infiltration. Laminectomy and partial tumour resection was performed on 65 patients and laminectomy with complete tumour excision on 19 patients; 44% became mobile in the immediate post-operative period, following partial resection, and 57% following radical extirpation after laminectomy. In 96% of the patients the study was able to identify the actual point in time when these symptoms started. In 75% of the patients the symptoms began with pain alone, and in 21% of the cases they began as transection or paresis with or without associated pain. Thirty-eight per cent of the patients who had initially only shown pain improved, and 35% of the patients with paresis also improved. The duration of pain varied from 1 day to 104 weeks, with an average of 8.2 weeks. The duration of paresis varied from 1 day to 7.5 weeks, with an average of 4 days. Forty-nine per cent of 37 patients, who had developed paresis within 48 h, were mobile post-operatively.
The average duration of hospitalisation was 9 days with a range of 7–12 days.
Complications
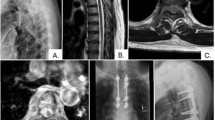
Intra-operative complications occurred in four cases (complication rate 4.7%). The most common intra-operative complication was dural opening in three patients, and laminectomy at the wrong level in one patient, which was immediately corrected through intra-operative X-ray.
Operative complications were experienced in five patients (5.9%): the most common complication was superficial wound infection found in four patients (4.7%), and an epidural abscess in one patient, where surgery had to be repeated.
Discussion
Our results showed that tumour patients with spinal cord compressing metastasis experienced an improvement in their quality of life. They achieved better mobility and continence function as well as a reduction of analgesic medication following palliative decompressive laminectomy. This indicates the method to be a valuable option in neurosurgical therapy.
Immediate decompression of the spinal canal to relieve cord compression caused by spinal metastasis is crucial in patients with associated neurological deficit, primarily in order to prevent further deterioration but also to obtain pain relief and partial or complete tumour extirpation.1,4,7,14
Due to the heterogeneous group of patients with varying prognoses,2,6,7,16,18,19 the therapeutic method of choice is often difficult and is subject to controversy among the authors. In 1980, Young and co-workers found no significant difference in clinical prognosis between laminectomy followed by radiotherapy and radiotherapy only in 29 patients.6
Management strategies were developed based on classification systems, but these have also been subject to much criticism.1,9 Bach and co-workers, however, found laminectomy followed by radiotherapy to be far superior to sole radiotherapy in a multicenter study involving 398 patients.1
Decompressive laminectomy had to be performed on 20 of our patients due to neurological deterioration after having received radiotherapy. Interestingly, these patients showed – even though to only a small degree – a better prognosis compared to those receiving radiotherapy following laminectomy. Furthermore, we noticed a higher rate of success in laminectomy combined with pre- or post-operative radiotherapy compared to laminectomy only. For this reason, randomised prospective studies with larger numbers of patients should be conducted.1,6,10,11,18,20
Nevertheless, the disadvantage of the dorsal approach lies in the inability to remove completely a ventrally located tumour3,7,14,15,17,19,21 rendering relatively moderate results even following subtotal tumour extirpation.4,7 We found ventral or ventrolateral as well as cuffed spinal cord compression in 85% of our patients. Radical tumour extirpation was performed on 19 patients who showed a higher degree of mobility post-operatively compared to those who had received partial tumour resection, which coincides with the literature.12 Byrne stated that neither the time elected for surgery nor the choice of surgery are clear and are still subject to much controversy.2 Since we were able to find a significant improvement in mobility, pain and continence leading to a better quality of life in patients suffering from terminal cancer, we consider the palliative decompressive laminectomy with total/partial tumour resection to be a favourable method of treatment. However, it must be mentioned that the prognosis is considerably lower than the ventral approach with vertebrectomy with implants, which results in neurological improvement in 75–95% of all cases.3,4,7,15,16,22
In our series, palliative laminectomy with total or subtotal tumour reduction in patients with malignant spinal metastatic disease resulted in amelioration of motor function, pain and continence and therefore improved patients' quality of life. The significant improvement in quality of life proves this method, with the exception of preoperative paraplegia, to be a valuable option in neurosurgical therapy. However, in patients with preoperative severe paraparesis, the authors recommend laminectomy only in very exceptional cases, because of the poor post-operative neurological results.
References
Bach F et al. Metastatic spinal cord compression Acta Neurochir 1990 107: 37–43
Byrne NT . Spinal cord compression from epidural metastases N Engl J Med 1992 327: 614–619
Overby MC, Rothman AS . Anterolateral decompression for metastatic epidural spinal cord tumours J Neurosurg 1985 62: 344–348
Sundaresan N et al. Treatment of neoplastic spinal cord compression: results of a prospective study Neurosurgery 1991 29: 645–650
Turgut M, Gül B, Girgin O, Taskin Y . Role of surgical treatment in 70 patients with vertebral metastases causing cord or root compression Arch Orthop Trauma Surg 1997 116: 415–419
Young RF, Post EM, King GA . Treatment of spinal epidural metastases J Neurosurg 1980 53: 741–748
Akeyson EW, McCutcheon IE . Single stage posterior vertebrectomy and replacement combined with posterior instrumentation for spinal metastasis J Neurosurg 1996 85: 211–220
Constans JP et al. Spinal metastases with neurological manifestations; Review of 600 cases J Neurosurg 1983 59: 111–118
Harrington KD . Metastatic disease of the spine J Bone Joint Surg 1986 68: 1110–1115
White AW, Patterson RH, Bergland RM . Role of Surgery in the treatment of spinal cord compression by metastatic neoplasm Cancer 1971 27: 558–561
Garcia-Picazo A, Ramirez PC, Rivas PP, Garcia de Sola R . Utility of surgery in the treatment of epidural vertebral metastases Acta Neurochir 1990 103: 131–138
Sherman RMP, Waddell JP . Laminectomy for metastatic epidural spinal cord tumours Clin Orthop 1986 207: 55–63
Enkaoua EA et al. Vertebral metastases, a critical appreciation of the preoperative prognostic Tokuhashi score in a series of 71 cases Spine 1997 22: 2293–2298
Harrington KD . Anterior cord decompression and spinal stabilization for patients with metastatic lesions of the spine J Neurosurg 1984 61: 107–117
Hosono N et al. Vertebral body replacement with a ceramic prosthesis for metastatic spinal tumours Spine 1995 20: 2454–2462
Rosenthal D, Marquard G, Lorenz R, Nichtweiß M . Anterior decompression and stabilization using a microsurgical endoscopic technique for metastatic tumours of the thoracic spine J Neurosurg 1996 84: 565–572
Shaw B, Frederick LM, Borges L . One stage posterolateral decompression and stabilization for primary and metastatic vertebral tumours in the thoracic and lumbar spine J Neurosurg 1989 70: 405–410
Khan FR, Glicksman AS, Chu FCH, Nickson JJ . Treatment by radiotherapy of spinal cord compression due to extradural metastases Radiology 1967 89: 495–500
Weller SJ, Rossitch E . Unilateral posterolateral decompression without stabilization for neurological palliation of symptomatic spinal metastasis in debilitated patients J Neurosurg 1995 82: 739–744
Gorter K . Results of laminectomy in spinal cord compression due to tumours Acta Neurochir 1978 42: 177–187
Kadar E, Kisfaldu N, Czirjak S, Jakab F . Resection of a giant schwannoma by combined surgical exposure Acta Chir Hungarica 1997 36: 158–159
Tomita K et al. Total en bloc spondyectomy and circumspinal decompression for solitary spinal metastases Paraplegia 1994 32: 36–46
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Schoeggl, A., Reddy, M. & Matula, C. Neurological outcome following laminectomy in spinal metastases. Spinal Cord 40, 363–366 (2002). https://doi.org/10.1038/sj.sc.3101324
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101324
Keywords
This article is cited by
-
Analysis of factors delaying the surgical treatment of patients with neurological deficits in the course of spinal metastatic disease
BMC Palliative Care (2018)
-
Paraplegia of spinal epidural compression by metastatic breast cancer and urgent radiotherapy—timeliness for naught?
Journal of Neuro-Oncology (2009)
-
Il trattamento delle metastasi vertebrali
LO SCALPELLO-OTODI Educational (2008)
-
Faecal incontinence as presentation of an ependymomas of the spinal cord
World Journal of Surgical Oncology (2007)
-
Circumferential stabilization with ghost screwing after posterior resection of spinal metastases via transpedicular route
Neurosurgical Review (2007)