Abstract
Study Design: A new method for prevention of cerebrospinal fluid leakage was studied.
Objective: To prevent cerebrospinal fluid leakage, we developed a polytetrafluoroethylene fascia patch inlay method.
Background: One of the major risks of the anterior approach for intra-dural spinal cord lesions is the cerebrospinal fluid leakage.
Methods: A small hemangioblastoma located on the ventral side of the cervical cord was resected with an anterior approach. The dural closure was performed using this polytetrafluoroethylene fascia patch inlay method.
Results: The patient had a satisfactory clinical course with no cerebrospinal fluid leakage.
Conclusion: This polytetrafluoroethylene fascia patch inlay method is very effective. This method may provide both prevention of CSF leakage and future spinal cord adhesion to the dura.
Similar content being viewed by others
Introduction
For the intramedullary spinal cord tumor, the posterior approach has been commonly employed.1,2,3 Only in selected cases was the anterior approach employed to reduce intra-operative cord injury.4,5,6,7 The anterior approach requires vertebrectomy and fusion. This relatively deep and narrow exposure make it difficult to achieve dural closure without CSF leakage, which can be hard to treat.8,9 This report describes in detail the procedure of the PTFE-fascia patch inlay method, which is useful for preventing CSF leakage associated with the anterior approach for intra-dural spinal lesions.
Methods and Results
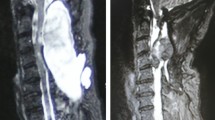
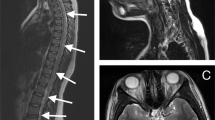
The case presented here had a small hemangioblastoma located on the ventral side of the spinal cord at the C5-level with a concomitant large syrinx extending from the medulla to the T4 level (Figure 1A). The anterior approach was selected because of the small size and the location of this tumor. The anterior surface of the C4 to the C6 vertebral body was exposed in the usual manner. Vertebrectomy was performed on C5 and the lower one-third of the C4 and upper one-third of the C6 vertebral body were drilled off. The size of the dural exposure was 28×18 mm. After the dura and arachnoid had been opened, the tumor could be totally removed. The PTFE sheet (WL Gore & Associates, Inc. AZ, USA), 0.1 mm in thickness, was cut to 30×10 mm in size. The fascia was then removed from the portion of the gluteus maximus muscle attached to the iliac bone crest. The fascia was sutured to the PTFE sheet at six points with PTFE Suture (CV 6-0 suture, WL Gore & Associates) to create the PTFE-fascia patch (Figure 2A). This patch was placed under the opened dura, and the surface of the spinal cord was covered with the PTFE side of the patch to prevent future spinal cord adhesion to the dura (Figure 2B). The dural edge and fascia of the patch were fixed with continuous suturing with CV 6-0 PTFE suture. A graft taken from the iliac crest was tailored to fill the gap between the C4 and C6 vertebral bodies and fixed with a cervical plate system. Prophylactic lumbar spinal drainage was performed for 4 days following surgery.
Hemangioblastoma of the cervical spinal cord. (A) T1-weighted magnetic resonance (MR) image with Gd-DTPA enhancement showing a small enhanced mass and extensive syrinx in the cervical cord. (B) Left vertebral angiogram indicating a highly vascular intramedullary tumor at C5. The tumor feeding artery and draining vein can be seen. (C) Post-operative MRI. T1-weighted magnetic resonance (MR) image with Gd-DTPA enhancement shows no evidence of residual tumor and reduction in size of the syrinx
Post-operative MRI demonstrated total removal of the tumor and a reduced syrinx size (Figure 1C). The patient shows no sign of CSF leakage and has enjoyed a satisfactory clinical course without additional neurological deficits.
Discussion
The anterior approach for intra-dural pathological abnormalities can be very effective in certain special cases, such as mid-ventral small hemangioblastoma, ventrally bleeding cavernous hemangioma and small AVM fed by the anterior spinal artery.4,5,6,7,10 The anterior approach provides direct access to the ventral surface of the spinal cord on both sides of the anterior spinal artery,4,11 so the feeding artery can be treated first. However, difficulties with watertight dural closure and the high risk of post-operative CSF leakage render an anterior exposure for an intra-dural pathological abnormality impractical in most cases.8,9
The PTFE-fascia patch inlay method, however, provides effective repair of the dura while preventing CSF leakage. Intra-dural CSF pressure compresses this inlay graft against the dural defect, so sealing of the dura should be complete. Hadly et al8 reported superior results with the fibrin glue technique and that it provided a solid intra-operative seal, even with repeated Valsalva maneuvers up to 40 mmHg.12 We previously used fibrin glue for another anterior approach case, but the patient had transient swallowing difficulty caused by CSF leakage. We therefore believe that our inlay method is the key for preventing CSF leakage.
While the PTFE sheet is thought to prevent future adhesion of the spinal cord to the dura, the fascia of this patch tends to adhere to the dura. For this reason, we developed the PTFE-fascia patch, which makes use of the advantages of the two materials. Sawa et al5 reported using the anterior approach for resection of an anteriorly located spinal meningioma extending from the foramen magnum to the second thoracic vertebral body. They repaired the dural defect with fascia fat and fibrin glue, which resulted in a satisfactory clinical course. Fat also prevents adhesion, but the preparation is more difficult than that of the PTFE sheet.
Prophylactic lumbar spinal drainage for several days may also be considered for the prevention of post-operative CSF leakage, and was also performed in the case reported here.
It is our belief that if the PTFE-fascia patch inlay method described here is used routinely, the anterior approach for intra-dural spinal lesions can be expected to become a more effective procedure.
References
Murota T, Symon L . Surgical management of hemangioblastoma of the spinal cord: a report of 18 cases Neurosurgery 1989 25: 699–708
Solomon RA, Stein BM . Unusual spinal cord enlargement related to intramedullary hemangioblastoma J Neurosurg 1988 68: 550–553
Xu QW, Bao WM, Mao RL, Yang GY . Magnetic resonance imaging and microsurgical treatment of intramedullary hemangioblastoma of the spinal cord Neurosurgery 1994 35: 671–676
Iwasaki Y, Koyanagi I, Hida K, Abe H . Anterior approach to intramedullary hemangioblastoma: Case report Neurosurgery 1999 44: 655–657
Sawa H, Tamaki N . Complete resection of a spinal meningioma extending from the foramen magnum to the second thoracic vertebral body via the anterior approach: Case report Neurosurgery 1993 33: 1095–1098
Sonntag VKH, Hadley MN, Spetzler RF . The transoral-transclival approach to the upper cervical spine In: Sundaresan N, Schmidek HH, Schiller AL et al (eds) Tumors of the Spine: Diagnosis and Clinical Management Philadelphia: WB Saunders 1990 pp 319–335
Williams Jr FC et al. Anterolateral transthoracic transvertebral resection of an intramedullary spinal arteriovenous malformation. Case report J Neurosurg 1991 74: 1004–1008
Hadly MN et al. Comparative transoral dural closure technique: a canine model Neurosurg 1988 22: 392–397
Yamaura A et al. Repair of cerebrospinal fluid fistula following transoral transclival approach to a basilar aneurysm. Technical note J Neurosurg 1979 50: 824–836
Giroux JC, Nohra C . Anterior approach for removal of a cervical intradural tumor: Case report and technical note Neurosurgery 1978 2: 128–130
Martin NA, Khanna RK, Batzdorf U . Posterolateral cervical or thoracic approach with spinal cord rotation for vascular malformations or tumors of the ventrolateral spinal cord J Neurosurg 1995 83: 254–261
Weakland HJ . The epidural blood patch–current practices and concerns CRNA 1994 5: 156–163
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Yuguchi, T., Kohmura, E. & Yoshimine, T. PTFE-fascia patch inlay method for the anterior approach for cervical intradural spinal lesion. Spinal Cord 40, 601–603 (2002). https://doi.org/10.1038/sj.sc.3101323
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101323