Abstract
Study design: Prospective study.
Objectives: To evaluate the feasibility of color ultrasound imaging of the urethra in association with UPP to diagnose intrinsic sphincter deficiency (ISD).
Setting: Italy.
Methods: We studied a group of 13 normal female volunteers (mean age 29 years) during the estrogenic phase and a group of 15 patients (mean age 63.9 years) with ISD. All patients and normal volunteers underwent color ultrasound imaging using a 4–7 MHz convex broad band transducer. Translabial sagittal scans of the urethra were obtained. The color ultrasound parameters were optimized for detection of parenchymal slow flows. A subjective score of the degree of vascularization along the entire urethra was established as follows: (a) minimal or absent (1), (b) poor (2), (c) moderate (3), (d) good (4). Statistical analysis, using the non-parametric Mann-Whitney rank sum test, was carried out to determine differences of ultrasound scores between volunteers and patients.
Results: The statistical evaluation showed that the differences between the ultrasound scores in the two groups was statistically significant (P<0.001).
Conclusion: We affirm that color ultrasound imaging of the urethra seems to be feasible and useful in association with UPP in the diagnosis of ISD even if this echographic investigation needs further observations.
Similar content being viewed by others
Introduction
The factors responsible for normal intrinsic sphincter closure are smooth muscle contractility, integrity of periurethral fascia, normal innervation and mucosal seal factors which include mucosal turgor and thickness and the vascularization of the urethra.
The contribution of blood flow and the action of hormones on urethral closure pressure, which constitute the main intrinsic mechanisms of urethral closure, are known from studies in which urethral pressure measurements were extensively employed.1,2,3,4
The urethral pressure profile (UPP) is at present the most urostatic measurement in the field of urodynamics. It is a topographic curve showing pressures along the length of the urethra. It does not, however, represent the real urethral function and, contrary to expectations, has been of limited practical value in the assessment and management of incontinence.
In the last few years the abdominal leak point pressure (ALPP) has allowed us to study and to classify the stress urinary incontinence (SUI), even if this technique needs to be standardized.
Recently some authors demonstrated that the new ultrasound digital equipment allows visualization of the urethral vascular flows5,6,7 and for this reason the aim of our study was to evaluate the feasibility of urethral color ultrasound imaging and the arterial vascularization of the urethra in association with UPP to diagnose intrinsic sphincter deficiency (ISD) in female patients.
Materials and methods
We studied two groups of women: (1) 13 normal volunteers (mean age 29.0 years), with an absence of pelvic floor disorders and no history of incontinence during the estrogenic phase, (2) 15 incontinent patients (mean age 63.9 years) affected by ISD due to failure of previous vaginal surgery for urinary incontinence in 14 cases and in one case due to spinal cord injury (SCI) at the S2-S3 level. Urodynamic evaluation was not carried out in normal volunteers because it was not accepted by this group of subjects for the invasiveness of the above mentioned exam.
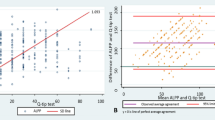
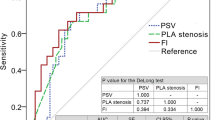
In all patients ISD was diagnosed by clinical and urodynamic investigations (pressure/flow study, VLPP, static and dynamic UPP by microtransducers). All subjects signed informed consent and underwent color ultrasound imaging with commercial digital equipment (HDI-5000, ATL, USA) using a 4–7 MHz convex broad band transducer. Translabial sagittal scans of the urethra were obtained by placing the transducers directly on the external urethral meatus. The color ultrasound parameters were optimized for detection of parenchymal slow flows. Images obtained from each subject were independently examined by two sonographers who were blind to the subject's clinical status and age. The sonographers were asked to give a subjective score of the degree of vascularization along the entire urethra as follows: (a) minimal or absent (1), (b) poor (2), (c) moderate (3), (d) good (4). We compared the values of the maximum closure urethral pressure (MCUP), performed by microtransducers, of each pathologic patient with the ultrasound score. Statistical analysis, using the non-parametric Mann-Whitney rank sum test, was carried out to determine differences between ultrasound scores in the two groups.
Results
The data are shown in Tables 1 and 2. All normal volunteers had a median score of 4 (Figure 1) except for two cases with a score of 3 (Figure 2). In the incontinent group 10 cases had a score of 2 (Figure 3) and five cases had a score of 1 (Figure 4). The Mann-Whitney rank sum test showed that the differences between the ultrasound scores in the two groups was statistically significant (P<0.001). The findings in the incontinent group were: a low ultrasound score, a low MCUP and a positive stress test in the supine position.
Discussion and Conclusions
In 1953 Berkow8 drew attention to the extensive blood supply to the urethra and Enhoning9 suggested that the rich urethral vascular network might act as an important auxiliary closing mechanism. This hypothesis was subsequently studied by Bump10 who tried to calculate the contribution of the vascular component to urethral pressure.
The resting UPP, made up of contributions from the sphincter and supporting structures in the urethra, can be measured exploiting the principles embodied in UPP methodology. This evaluation gives a graph incorporating all closure forces involved in compressing the urethral lumen. Vascular, skeletal and smooth muscle components of urethral closure play important roles in forming the shape of the UPP. In 1980 Rud carried out a systematic study to characterize the contribution of striated and smooth muscles within the urethra with reference to the influence of systemic blood pressure. This study revealed that striated muscle in the urethra, including the pelvic floor, is responsible for one third of total intraurethral pressure, that another third of urethral closure is due to blood flow and that the remaining third is the consequence of contributions from connective and periurethral tissues.
It is, therefore, evident that the vascularity of the urethra effects closure and that hormones play a very important role in modifying the softness of the urethra which makes it amenable to skeletal muscle compression. Hormonal and biomechanical changes of the components of the urethra and its surrounding structures modulate the magnitude of the UPP values. Estrogen and progesterone, in particular, are known to affect most components that contribute to urethral closure in many ways, such as biomechanical softening of the tissues, interaction with estrogen receptors, modification of adrenergic receptor density and innervation, changes to electrophysiological properties of smooth muscle, inhibition of extraneuronal uptake of catecholamines, modification of cholinergic responses and interaction with prostaglandins.2,11
In clinical practice, however, the reported effects of estrogen treatment, in terms of cure rates and urethral profile measurements, are conflicting.3,4,12,13
These aspects confirm, as is known, that UPP is of limited practical value in studying continence or in the follow-up of incontinent patients undergoing estrogen therapy.
The feasibility of color ultrasound imaging of the female urethra in normal subjects was previously reported by us, showing an increase of resistive index (RI) in the proximal urethra justifying the presence of a `seal effect' related to the existence of a rich venous urethral vascularization involved in the mechanism of urethral closure.7
In the present study, in some patients, the ecographic score did not correlate with the MCUP and this finding could be an indication that sometimes the UPP is of limited practical value while color ultrasound imaging of the female urethra allowed visualization and classification, using a subjective US score, of the urethral arterial vascularization of normal volunteers and patients affected by ISD.
The ultrasound score was consistent with the clinical evaluation in all patients affected by ISD and in only one normal volunteer did the ultrasound score show moderate urethral vascularity. In particular, in the patient affected by neurogenic stress incontinence the US score showed poor urethral vascularity probably due to an alteration of autonomic innervation of the arterial vascularization component of the urethra in consequence of SCI at the S2-S3 level. This ecographic finding, if confirmed by a sufficient number of cases, could represent an important tool with UPP in the diagnosis of neurogenic female stress incontinence.
In conclusion we can affirm that color ultrasound imaging of the urethra seems to be feasible and useful in association with UPP in the diagnosis of ISD even if this echographic investigation needs further observations.
References
Rud T et al. Factors maintaining the intraurethral pressure in women Invest Urol 1980 17: 343
Iosif CS, Batra S, Ek A, Astedt B . Estrogen receptors in the human female lower urinary tract Am J Obstet Gynecol 1981 141: 817
Miodrag A, Castleden CE, Vallance TR . Sex hormones and the female urinary tract Drugs 1988 36: 491
Sorensen S . Urethral pressure variations in healthy and incontinent women, doctoral thesis Neurourol Urodyn 1992 11: 549
Beco J, Léonard D, Léonard F . Study of the female urethra's submucous vascular plexus by color Doppler World J Urol 1998 16: 224
Jackson J et al. Is postmenopausal urethral blood flow affected by hormone replacement therapy? A placebo controlled pilot study Neurourol Urodyn 1997 16: 352
Siracusano S et al. Colour Doppler ultrasonography of female urethral vascularization in normal young volunteers: a preliminary report BJU Int 2001 88: 378
Berkow SG . The corpus spongiusum of the urethra: its possible role in urinary control and stress incontinence in women Am J Obstet Gynecol 1953 65: 346
Enhorning G . Simultaneous recording of the intravesical and intraurethral pressure Acta Chir Scand 1961 276: Suppl 1
Bump RC, Huang KC, McClish DK, Fantl JA . Effect of narcotic anesthesia and skeletal muscle paralysis on passive and dynamic urethral function of stress continent and incontinent women Neurourol Urodyn 1991 10: 523
Caine M, Raz S . Some clinical implications of adrenergic receptors in the urinary tract Arch Surg 1975 110: 247
Walter S, Wolf H, Barlebo H, Haakon Kaalund Jensen . Urinary incontinence in post-menopausal women treated with estrogens: a double-blind clinical trial Urol Int 1978 33: 135
Wilson PD et al. Treatment with oral piperazine oestrogene sulphate for genuine stress incontinence in post-menopausal women Br J Obstet Gynaecol 1987 94: 568
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Siracusano, S., Bertolotto, M., Silvestre, G. et al. The feasibility of urethral color ultrasound imaging in the diagnosis of female intrinsic sphincter deficiency: preliminary results. Spinal Cord 40, 192–195 (2002). https://doi.org/10.1038/sj.sc.3101276
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101276
Keywords
This article is cited by
-
Assessment of urethral vascularity using 2D colour Doppler high-frequency endovaginal ultrasonography in women treated for symptomatic stress urinary incontinence: 1-year prospective follow-up study
International Urogynecology Journal (2016)
-
Pelvic floor disorders: role of new ultrasonographic techniques
World Journal of Urology (2011)
-
A comparison of periurethral blood flow resistive indices and urethral closure pressure of incontinent women
International Urogynecology Journal (2006)