Abstract
Study design: A theoretical model of spinal stability is proposed.
Objective: To present a biomechanical study in vitro using flexibility and loading tests of the normal lumbar spine and of two lumbar models of spinal stability in order to determine which of the lumbar middle-column model and the personal suggested model of lumbar central axial pillar is more resistant and stable.
Setting: Hospital ’Sf.Treime‘, Iasi, Romania.
Methods: Twenty-three fresh human cadaveric lumbar spines were tested with flexibility and loading tests of the intact lumbar functional units and of two types of spinal model specimens: 10 lumbar middle-column models and 13 lumbar central pillar model specimens. Parameters of vertebral motion and vertebral compression were compared to determine the differences between the types of spinal models.
Results: The flexibility tests show a significant increase in motion of the lumbar middle-column model specimens compared to the lumbar central pillar model specimens. The lumbar central pillar model specimens are three times more stable compared to the middle-column models. The compression tests show that the lumbar central axial pillar model specimens were more resistant, on average by 10% (30% maximum) compared to the other model.
Conclusions: The lumbar model formed by the axial overlapping of the posterior half moon of vertebral body continued by the pedicles and the articular processes is more stable and more resistant compared to the middle-column model of the three-columns theory of Denis. In the lumbar spine this central axis spinal pillar is the structure of spinal stability and resistance, and I propose this central axial spinal pillar as the stabilizing structure for all the spine.
Similar content being viewed by others
Introduction
The concept of spinal stability was introduced in 1931 in the Watson-Jones classification of spinal fractures. Spinal stability may be difficult to define.1,2,3,4 The classic anatomical definitions of spinal stability are based on the two-columns theory of Holthworth (1963),4 the three-columns theory of Denis (1983)5,6 and the three-columns theory of Louis (1985).7 Spinal stability is a constant spinal biomechanical behaviour between the limits of the next responses to the spinal loadings and/or to the spinal motions and for the protection of the spinal cord.
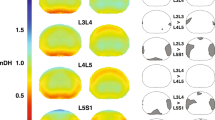
I put forward a view on the spinal stability based on the concept of the central axial spinal pillar8 (Figures 1 and 2). The posterior third of the vertebral body is continued by the pedicles and the two articular processes and together they form the central vertebral segment or the ’vertebral core‘. Axial overlapping of these central body-pedicles-facets segments forms a single central pillar of stability and resistance. This central axial spinal pillar is anatomically segmented but biomechanically continuous and it is the structure of spinal stability and of spinal resistance.
The body–intervertebral disc segments situated at the front of this central stability pillar make up by axial overlapping an anterior secondary pillar predominant for elastic loading transmission. The overlapping of the laminae and of the spinous processes with the tensile connecting ligaments is behind the central pillar. This posterior structure constitutes a rigid pillar whose functions are to anchor (as bracing wire) and to limit torsion and translation movements.
This paper presents an experimental study on the biomechanical behaviour of the classical columns and of this proposed central axial spinal pillar of the lumbar spine.
Methods
Twenty-three fresh human cadaveric lumbar spines were tested for the present study. The age of the specimens was between 25 years and 64 years, with the average of 50.2 years.
Specimen preparation
Lumbar vertebral segments L1-L4 (or L2-L5) were removed from cadaveric spines and all musculature was removed preserving ligaments and bone. Antero-posterior and lateral radiographs of all spines were taken to detect anatomic abnormality, serious degenerative diseases or neoplastic diseases.
Each lumbar spine was divided in two segments: superior functional spinal unit (FSU) L1/L2 and inferior FSU L3/L4 (or L2/L3 and L4/L5).
Ten superior lumbar segments were created resulting in 10 middle column segments and 13 superior lumbar segments were formed resulting in 13 central axial spinal pillar segments (Figures 3 and 4).
Flexibility and loading testing
First all superior intact lumbar spinal segments were tested for maximum motion of flexion, extension, axial rotation and lateral bending. After the middle column and central axial spinal pillar pattern-making, the spinal motions were tested once again in the same conditions. Then the 23 intact inferior lumbar segments, the 10 superior lumbar middle-column segments and the 13 superior lumbar central axial pillar segments were tested through axial compression.
The axial compression was measured using an automatic machine for strength of materials experiment, type FPZ: 100/1 (produced by Heckert, Germany) with the compression force increasing from 0 to 10 kN in 1 min at a speed of 10.29 mm/min (Figures 6,7,8). The diagram of loading test shows the moment of the fractures of the spinal segments (Figure 9). The cross-surface of all specimens was measured earlier (Figure 5).
Diagram of compression force-time: (a) intact lumbar segment and lumbar central axial pillar specimen; (b) intact lumbar segment and lumbar middle-column specimen; compression force: — intact lumbar segment, ······ central pillar specimen, –· middle-column specimen, down left arrow, moment of fracture
Stability parameters
The maximum motions of the intact lumbar segments may be compared with the middle column segments and with the central axial pillar segments using the stability index.9 The stability index is defined by the equation:

A higher value indicates a less stable situation between the two models as compared with the intact lumbar segment.
The spinal resistance established for the normal FSU and for the two spinal models can be compared by the spinal tension σ:

The ratio σof spinal model/σof intact spine shows the spinal resistance.
When this tension ratio is nearing one, the resistance of the spinal model is near that of the intact spine specimen.
Results
In flexion, the movements of the models of central axial lumbar spinal pillar were between 7° and 12° compared to the same intact lumbar segments that were between 6° and 10°, and the stability index was between 0.11 and 0.33.
In extension, the increase of motion of the lumbar central pillar model compared to the same intact lumbar segment was of maximum angle of two degrees. The stability index was between 0 and 0.4 for extension.
Axial rotation and lateral bending were the same for the lumbar central pillar model as for the same intact lumbar segment. The flexion motions of the lumbar middle-column models increased by 3°–5° and the stability index was between 0.37 and 0.66.
In extension the motions increased by 2°–4° and the stability index was between 0.33 to 1. Also there was an increase of the axial rotation and of lateral bending motions of two or three degrees for the lumbar middle-column models. The results of these flexibility tests are presented in Tables 1, 2 and 3.
The compression tests of three types of lumbar segments show that the mean force of 6.4 kN breaks the normal lumbar FSU (L3/L4 or L4/L5 segment) and the mean fracture pressure (fracture tension) was 314 N/cm2. The compression tension σ of mean 270–280 N/cm2 fractures the central axial lumbar pillar model and the mean fracture tension in the middle-column model was of 224–250 N/cm2. The results of the compression tests are presented in Tables 4 and 5.
Discussion
Spinal instability is an inadequate functional response determined by an anatomical spine injury, either preceding or caused by non physiological spinal motion or spinal loading. The stability ensures the security of the spinal biomechanical behaviour.10,11 Spinal cord and radicular protection is the final and not the first task of spinal stability. The biomechanical security limits are the segmental mobility limits and exceeding them can later endanger the spinal cord.1,8,12 Segmental mobility is a result of motion transmission and of the eccentric transmission of spinal loading.
The central axial spinal pillar is formed by the overlapping of the posterior third half moon of vertebral body, the pedicles and the articular processes (Figure 1). The central pillar has in cross-section a ’H‘ or ’X‘ shape which ensures biomechanically the maximum upright stability using the minimum anatomical material. The vertebral pedicles unite laterally the vertebral posterior segment with the facets, like two buttresses and thus the pedicles reinforce this structure which constitutes the central spinal pillar of stability.
The cross-section of the central pillar expands downwards because of the increase in the posterior segment of the vertebral body. The surface of the vertebral body's posterior third augments gradually caudally in the thoracal and lumbar spine. This shows the importance of the pedicles–facets segment for stability in the upper spine and the gradual increase in the importance of the vertebral body's posterior segment for stability and resistance in the lumbar spine. The base of the central spinal pillar is made of the sacrum and it is embedded in the pelvis providing the solidity of the entire superjacent structure (Figure 2).
The vertebral body and intervertebral disc segments situated in front of the central stability pillar make up by axial overlapping a secondary anterior pillar for predominantly elastic transmission of the loading.
The overlapping of the laminae and of the spinous processes with the tensile connecting ligaments13 constitutes a secondary posterior pillar for making it rigid and blocking the torsion and translation spinal movements.8
The multidirectional flexibility tests used for the intact lumbar L1/L2 or L2/L3 segments14,15 and then for the two anatomic lumbar models show significant increases of motion for the lumbar middle-column models compared to the lumbar central pillar models (Table 3).
All four movements tested amplified by more than 2 degrees for the lumbar middle-column models. The stability index quantifies the instability for the two models. A zero value indicates that the lumbar model was as stable as the intact lumbar segment. The higher values of the stability index for the lumbar middle-column models as compared with the lumbar spine is more stable. The differences between these two models based on the flexibility tests are significant. The middle-column model was threefold more unstable compared to the lumbar central axial pillar model in the lumbar spine.
The compression tests show different values for the fracture forces and the fracture tension of the three types of lumbar specimens because of the differences of cross-section surface and because of the differences of the characteristic structure. The intact lumbar segment specimens fracture by compression at a maximum 7.12 kN in our tests and the maximum fracture tension σ was of 380 N/cm2. The lumbar central pillar model specimens have a more elastic biomechanical behaviour compared to the lumbar middle-column model specimens, because of the facet joints. This additional elastic biomechanical behaviour increases the resistance and the fracture tension σ for the lumbar central pillar model specimens were bigger with a mean of 10% compared with the fracture tension of the lumbar middle-column model specimens.
The pressure ratios for these two models were between 0.76 to 0.94 for lumbar central pillar models and between 0.67 to 0.83 for middle-column models. The analysis of two specimens: one of central lumbar pillar model and the other of lumbar middle-column model at the same level and with similar parameters for intact lumbar segment (Case 9–Table 4, upper part and Case 8–Table 4, lower part) shows a difference loading of 300 N. The difference loading for all cases is between 300 to 500 N, therefore the lumbar central axial pillar model specimens can sustain in addition 30–50 Kg compared to the lumbar middle-column model specimens.
Following the compression tests all cases of lumbar intact FSU fractured at the upper vertebra and the fractures were of the entire vertebral body, type vertebral collapse (Figures 10 and 11)
The specimens of lumbar middle-column model and of the lumbar central pillar model both fractured at the upper vertebra.16,17 Also, in the cases of lumbar central axial specimens the spinal injuries included facet dislocations.
The results show that the additional elasticity of the lumbar central axial pillar model specimens increases the resistance in front of the compression forces compared to the lumbar middle-column model.
The axial central spinal pillar maintains the orthostatic posture and transmits elastically and plastically spinal loading and movements; the anterior secondary pillar takes over the loading elastically and the posterior secondary pillar limits the amplitude in order to protect the axial pillar. The secondary pillars also limit flexion-extension movements.
This proposed pattern establishes a correlation between the spinal structural lesions and the functional response represented by spinal instability. According to this model spinal instability is caused by the disruption of the continuity of the central spinal pillar and jeopardises the static stability and the response to loading or movement. Injuries of the secondary pillars do not cause biomechanical instability; injuries of the posterior arch can produce spinal cord compression although the spine is stable.
The lesion of the central spinal pillar cannot be isolated from the lesions of the secondary pillars; the lesions of the secondary pillars are partial or complete according to the mechanisms of injuries. A complete lesion of the central pillar or an extended lesion of the vertebral body including a lesion of the posterior ligament can cause instantaneous instability. When the central spinal pillar lesion coexists with the lesion of the secondary posterior pillar the following can occur:
–the facets bilateral lesion produces a late gradual instability;
–the facets and pedicles bilateral lesion causes a precocious gradual instability;
–full lesion of the central axial spinal pillar determines instantaneous instability.
A vertebral body lesion without injury of the posterior cortical layer nor of the vertebral posterior ligament and with a lesion of the secondary anterior pillar can sometimes produce a late instability. These types of lesion of the central pillar represent an instability risk and determine the treatment of spinal fractures:
–immediate stabilization through orthosis or surgical stabilization;
–surgical decompression with or without surgical stabilization or postoperative orthosis.
Some systems of spinal fixation cannot make a good spinal stabilization because of the lack of restoration of the axial central spinal pillar: classic posterior hook-rod systems and segmentally fixed-rod systems (Luque), interspinous wiring or sublaminar wiring. Also lateral mass plates and screws for the cervical spine are frequently ineffective in the treatment of progressive kyphotic deformities. Instrumentation Cotrel-Dubousset is a compact system for segmental spinal rigid making system without axial spinal pillar restoring. According to this model the best restoration of the central axial pillar is made by the systems of posterior spinal interbody fusion, or anterior spinal interbody fusion (PLIF and ALIF for lumbar spine) and the systems of spinal fusion using transpedicular screw devices.
Conclusion
A biomechanical spinal pattern consisting of one central pillar and two secondary pillars is presented here:
–an axial central pillar for stability and resistance by overlapping of the posterior third of the vertebral body continued with the pedicles and the two facets;
–a secondary anterior pillar for predominantly elastic transmission of the loading;
–a secondary posterior pillar for making rigid (anchoring as bracing wire) and blocking the torsion and translation movements.
The current study showed that in the lumbar spine the central axial spinal pillar model was more resistant and more stable compared to the middle-column spinal model. The better stability is determined by the ’H‘ shape and the bigger cross-section surface of this central axial pillar. The centre of weight is projected inside the basal cross-section surface of the central axial spinal pillar. The increased resistance is determined mainly by the greater elasticity induced by the inclusion of the facet joints in the central axial spinal pillar model.
Therefore the central axial pillar in lumbar spine is the spinal structure for resistance and stability. Spinal instability appears by the disruption of the biomechanical continuity of the axial central spinal pillar determined by an anatomical lesion and endangers the static spinal stability and the spinal response to loading or/and movements, with or without spinal cord damage.
Biomechanical knowledge of spinal instability can help the prevention of postoperative instability by protecting or reconstructing the central spinal pillar. The assessment of post-traumatic spinal instability helps determine the most appropriate treatment: the complete lesion of the central pillar causes instantaneous instability and requires axial reconstruction and orthopaedic or surgical stabilization, while partial lesion of the central pillar can produce instability, depending on which central pillar segment was injured and on the extent of the secondary pillars damage.
The surgical approach also depends on the existence of spinal cord compression and the stabilization type is selected in order to eliminate the instability and according to the surgical risk.
References
Kirkaldy-Willis WH, Farfan HF . Instability of the lumbar spine Clin Orthop 1982 165: 110–123
Panjabi MM . The stabilizing system of the spine. Part I. Function, dysfunction, adaptation and enhancement J Spinal Disord 1992 5: 383–389
Panjabi MM . The stabilizing system of the spine. Part II. Neutral zone and instability hypothesis J Spinal disord 1992 5: 390–397
Pintar FA, Maiman DJ, Yoganandan N . Clinical and experimental biomechanics of the spine (chapter 152), in section I Degenerative disc disease and selected spinal disorders In: Tindall GT, Cooper PR, Barrow DL (eds) The Practice of Neurosurgery CD Version 4.18.4–June 11 1997 Baltimore: Williams & Wilkins
Denis F . The three column spine and its significance in the classification of acute thoracolumbar spinal injuries Spine 1983 8: 817–831
Denis F . Spinal instability as defined by the three-column spine concept in acute spinal trauma Clin Orthop 1984 189: 65–76
Louis R . Spinal stability as defined by three-column spine concept Anat Clin 1985 7: 33–42
Iencean SM . Traumatic spinal instability Personal communication, Word Spine 1, Berlin, 27.08.-1.09.2000
Wang JL, Panjabi MM, Isomi T . The role of bone graft force in stabilizing the multilevel anterior cervical spine plate system Spine 2000 25: 1649–1654
Pope MH, DeVocht JW . The clinical relevance of biomechanics Neurologic Clinics 1999 17: 1
Stokes IAF, Frymoyer JW . Segmental motion and instability Spine 1987 12: 688–691
Krismer M et al. Biomechanik der lumbalen instabilitat Orthopade 1997 26: 516–520
Pintar FA et al. Biomechanical properties of human lumbar spinal ligaments J Biomech 1992 25: 1351–1356
Diaconescu N, Veleanu C, Klepp HJ . Biomechanics of the spine In: Diaconescu N, Veleanu C, Klepp HJ (eds) The spine, structure and function Bucuresti: Ed. Med 1977 pp 201–287
Panjabi MM et al. Validity of the three-column theory of thoracolumbar fractures. A biomechanic investigation Spine 1995 29: 1122–1127
Bay BK, Yerby SA, McLain RF, Toh E . Measurement of strain distribution within vertebral body section by texture correlation Spine 1999 24: 10–17
Frei HP, Oxland TR, Slomczykowski M, Nolte L-P . Vertebral body deformations contrasted under compression and shear loading Communication, ISSLS Annual meeting 1997, Singapore, June 2–4 (57)
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Iencean, S. The stabilizing axial spinal pillar in the lumbar spine. Spinal Cord 40, 178–185 (2002). https://doi.org/10.1038/sj.sc.3101272
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101272