Abstract
Study design: A cross-sectional study.
Objective: To clarify the existing controversy with regard to whether paraplegic patients suffer a loss of bone mass in the upper limbs.
Setting: Madrid, Spain.
Methods: We evaluated bone mass by phalangeal ultrasonography in 35 male patients with paraplegia (mean age 49±12 years), and 25(OH)D3 and PTH to exclude the presence of osteomalacia and secondary hyperparathyroidism. Spasticity was evaluated according to the Ashworth scale. Patients were compared with a control group of 35 healthy male subjects (mean age 48±13 years).
Results: The patients had lower 25(OH)D3 levels and amplitude-dependent speed of sound (Ad-SOS) than controls (both P<0.001), and higher PTH levels (P<0.05). There was a statistically significant negative association between PTH and 25(OH)D3 levels (r=−0.52, P<0.0001, CI −0.73 to −0.22) and between 25(OH)D3 and injury duration (r=0.34, P<0.05, CI −0.60 to −0.01). There was no correlation between Ad-SOS values, levels of PTH or 25(OH)D3, and the injury duration. No significant difference in Ad-SOS values was found in patients grouped according to low-to-normal 25(OH)D3 level or according to normal-to-high PTH level. There were no differences in relation to muscle tone. Only alkaline phosphatase and tartrate-resistant acid phosphatase levels were higher in patients than in controls (both P<0.001).
Conclusion: Paraplegic patients had a loss of phalangeal bone mass that was unrelated to the levels of vitamin D or PTH, or to muscle tone, so it seems to be related to increased bone resorption rather than to deficient bone formation.
Similar content being viewed by others
Introduction
Recent progress in the management of spinal cord injury (SCI) has prolonged the survival of patients. Subsequently, the incidence of secondary bone and joint disorders has increased in patients with SCI. The existence of osteopenia and osteoporosis in these patients is well-documented,1,2,3,4 but most studies have examined only small populations of patients (for instance, Biering-Sorensen et al3 studied eight patients [six men and two women], and Garland et al4 compared only 10 controls with 20 chronic patients). Therefore, the results of these studies have been debated. Regardless of the number of patients studied, osteopenia and/or osteoporosis have been related with various causes, such as the age and sex of the patient, time since injury, site of the neurological lesion (paraplegia or tetraplegia), muscle tone, degree of mobility, adaptation to a good rehabilitation program, use of medication, post-SCI changes in body composition, and disturbances in the calciotropic hormones,5,6,7,8,9 among others. It has been reported recently that all patients with SCI suffer osteoporosis of the paralyzed extremities.8
Studies of these patients have been made with densitometric techniques (dual photon absorptiometry [DPA] and dual-energy X-ray absorptiometry [DXA]),1,2,3,4,9 or peripheral quantitative computed tomography (pQCT).10 We know of no studies that have evaluated osteopenia in patients with SCI using quantitative ultrasound techniques (QUS). This technique has drawn the attention of the scientific community in recent years as a low-cost, sensitive and radiation-free method for identifying patients with osteoporosis and predicting the risk of hip fracture. Attention has focused on ultrasound as a potential tool for obtaining information in vivo not only on bone density, but also on bone quality.11 On the other hand, the diagnostic sensitivity of ultrasound has been found to be comparable to measurements obtained with spinal and proximal femoral DXA.12 Even so, these techniques can only be used to define the degree of osteopenia. However, since osteomalacia with secondary hyperparathyroidism5 has been reported in patients with SCI, determinations must be made of 25(OH)D3 and PTH levels in order to define adequately the degree of osteopenia and concomitant presence of osteoporosis and/or osteomalacia with secondary hyperparathyroidism.
Therefore, we wanted to use QUS to assess bone mass (quantity and quality) by scanning the phalanxes in a group of patients with SCI, in which we also studied muscle tone and the possible existence of osteomalacia and hyperparathyroidism, by determinations of 25(OH)D3 and PTH.
Materials and Methods
The study was carried out in January and February, 1999. Each month had an average of 219 h of sunlight. A total of 35 chronic male patients with paraplegia (mean age 49±12 years) were studied. Subjects' neurological levels ranged from T4 to T10. The severity of lesion of the subjects was assessed using the ASI Impairment scale, with 5 ‘A’, 12 ‘B’ and 18 ‘C’. Duration of injury ranged from 5 to 33 years. The control group was composed by 35 males of similar age (48±13 years), race, and geographic origin, who were deemed normal on the basis of blood tests and clinical history. Both groups had no dietary restrictions. None of the persons in either group was taking medication that could interfere with calcium metabolism. Patients and controls were from the Health District of Cáceres, Spain. The patient group collaborated enthusiastically in the study. All gave written informed consent, and the Office for Protection of Research Risks of the University of Extremadura approved the study, in accordance with the Helsinki Declaration of 1975.
The data of the two groups are summarized in Table 1. Baseline blood tests and Ad-SOS measurements were made in the same session. Spasticity was assessed using the modified Ashworth Scale.13
Ultrasound studies
Prior to the study, conventional radiographs of both hands were made in order to exclude pathological alterations at the measurement sites. As in previous studies,14 bone status was assessed using an ultrasound device model DBM Sonic 1200® (IGEA, Carpi, Italy) to measure amplitude-dependent speed of sound (Ad-SOS) in meters per second. Phalanges (II–V) of the non-dominant hand were measured and an average value was computed. Coupling was achieved using standard ultrasound gel. Two 16 mm-diameter, 1.25 MHz transducers mounted on a high-precision caliper measured the distance between probes. The probes were positioned on the mediolateral phalangeal surfaces using the phalanx head as a reference point. Positioning and repositioning this instrument is easy because the prominences of the lower phalangeal epiphysis are used as references. Instrument position was determined from three measurements in eight subjects made at time intervals not exceeding 21 days. The coefficient of variation (CV) was 0.77%. Inter-observer CV was 1.1%.
Analytical studies
No coffee, tea, smoking, alcohol, or exercise was permitted for 24 h before the investigation. The hematological and biochemical studies were performed on blood samples taken in the fasting state at 0800 h. Biochemical measurements were made of blood glucose, transaminases, GGT, creatinine, calcium, phosphorus, total proteins, bilirubin, alkaline phosphatase (AlPh), tartrate-resistant acid phosphatase (TRAP), and a coagulation study. In all cases, calcium was corrected for proteins according to Parfitt.15 A biochemical study of calcium excretion and tubular phosphate resorption was made in a 24-h urine sample. The biochemical parameters were measured in blood serum using a BM/Hitachi Automated Analyzer System 717 (Boehringer, Mannheim, Germany). Serum TRAP was quantified in the Hitachi automated analyzer with α-naphthyl substrate, using a reagent from Boehringer Laboratories (Boehringer, Mannheim, Germany) that reacts specifically with the isoenzyme 5β synthesized by osteoclasts.16 Twenty-four hour urinary calcium excretion was determined by atomic absorption spectroscopy using a Perkin Elmer Model 5000 spectrophotometer (Perkin Elmer, Norfolk, CT, USA). Blood samples were centrifuged and serum was stored at−20°C until analyzed. All samples were analyzed in the same assay to eliminate inter-assay variation. Assay reproducibility was determined by assaying four samples five times in five different runs. The CV between runs was determined by components of variance.17 In every case, the CV was less than 6%. PTH was determined using the Intact PTH IRMA kit (Nichols Institute Diagnostic, San Juan Capistrano, CA, USA). The intra-assay and inter-assay CV was <5% for both. 25(OH)D3 was determined with the 25OH-vit. D3-RIA-CT kit of Biosurce Europe, S.A. (Zoning Industriel, Nivelles, Belgium). The intra-assay and inter-assay CV was <8% in both.
Statistical studies
All values were expressed as mean±SD. The normal distribution of data was confirmed by calculating skew and kurtosis before applying standard tests. The groups (patients and controls) were compared using analysis of variance to determine the differences. A minimum P-value of <0.05 was the necessary condition for statistical significance. Regression and correlation analysis was used as appropriate to examine relations between continuous variables. These studies were carried out with the StatView 5.0.1. program (SAS Institute Inc., Cary, NC, USA) on a Macintosh computer.
Results
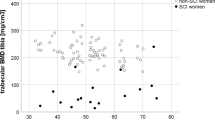
The results obtained for the variables analyzed are shown in Table 1. The patients had lower 25(OH)D3 and Ad-SOS values than controls (P<0.001 and <0.05 respectively) and higher PTH levels (P<0.05). In the patient group, 46% had 25(OH)D3 values below 15 ng/ml, the lower limit of the accepted normal range, which is defined as vitamin D deficiency by convention.18 Seven patients (20%) had PTH levels above 65 pg/ml, the accepted upper limit. Ad-SOS did not correlate with either PTH or 25(OH)D3 levels. There was a statistically significant negative association between PTH and 25(OH)D3 (r=−0.52, P<0.0001, CI −0.73 to −0.22) (Figure 1). Ad-SOS did not correlate with the duration of the condition. There was a statistically significant negative association between the duration of the injury and 25(OH)D3 (r=−0.34, P<0.05, CI −0.60 to −0.01).
No significant difference in Ad-SOS values was found among the patients grouped by low-to-normal 25(OH)D3 levels (1990±87 vs 1999±121 m/s, respectively, p NS). The difference in Ad-SOS in the patients grouped by high-to-normal PTH was not significant (1994±83 vs 1996±112, respectively, p NS). No differences in Ad-SOS were observed in relation to muscle tone. After excluding the only two cases of muscular flaccidness, Ad-SOS was 1999±95 in patients with muscle spasm versus 2072±49 m/s in controls (p NS).
Other basline biochemical values are listed in Table 1. In the patients, only alkaline phosphatase and TRAP levels showed statistically significant differences between patients and controls (P<0.05 and <0.001, respectively). No changes were observed in serum creatine, corrected serum Ca, serum P, total proteins, AST, and ALT.
Discussion
Indirect and in vivo experiments have shown that QUS may provide information not only about bone mass but also about bone tissue architecture and elasticity.11 Several studies have demonstrated that QUS measurements of the patella, tibia, or phalanges can identify patients who are prone to vertebral fractures as effectively as DXA of the spine, hip, or forearm. These studies have found that the diagnostic sensitivity of QUS is equal to or greater than that of DXA of the spine and hip.12 A longitudinal study has shown that radiogrammetry of the metacarpals can predict hip fractures.19 A cross-sectional trial has demonstrated that radiographic absorptiometry of the phalanges discriminates between osteoporotic and healthy postmenopausal women.20 In another study, radiographic absorptiometry of the phalanges of elderly women disclosed a larger deviation from peak adult bone mass compared with other techniques such as spinal DXA, spinal QCT, femoral neck DXA, and forearm DXA.21 The phalanx is considered to be of special interest, as it seems to be very sensitive to early bone resorption.22 Our Ad-SOS data for this site indicate a reduction in bone density in the patient group, compared with the control group.
Several bone disorders, both axial23 and peripheral,24 have been described in patients with SCI. Stress fractures also have been reported, mainly as a result of severe osteoporosis,25 and osteoporosis with or without osteopenia.1,2 Osteopenia has been reported to be due more to decreased bone formation than to accelerated bone resorption.26 However, Pietschmann et al27 observed the opposite, a significantly higher urinary hydroxyproline/creatine ratio in patients than in controls, as Naftchi et al28 also observed in patients with tetraplegia and paraplegia. Our observation of an elevation in TRAP and alkaline phosphatase in patients compared with controls supports these findings.
Regardless of the mechanism of osteopenia in paraplegics, the findings related with osteopenia are debated. Dauty29 recently reanalyzed this problem in 31 patients with SCI and concluded that the degree of demineralization of the lumbar spine, pelvis, and lower limbs is independent of the neurological level of the injury. In 27 male and two female patients with SCI, the trabecular and cortical bone mineral density (BMD) of the radius and ulna was significantly reduced in persons with tetraplegia, but no changes in the trabecular or cortical BMD of the radius and ulna were detected in persons with paraplegia.10 Garlan,4 in paraplegic and tetraplegic subjects, detected significant differences only in the arms and trunk. In 19 patients with permanent paraplegia, a significant deficit was found in the tibia, but a barely significant deficit in the distal forearm for the group as a whole.30 We observed similar, but more significant, results using QUS on the phalanxes.
Forty-six per cent of our patients had low 25(OH)D3 levels, but only 20% had elevation of serum PTH levels. We believe that the changes observed in vitamin D levels were not related to seasonal variations in the availability of vitamin D, as reported by Haddad et al.31 To control this factor, our study was carried out in a 1-month period when the amount of vitamin D provided by the environment is relatively constant: solar and meteorological conditions are stable, and there was little change in the dietary habits of the participants. Elias and Gwinup26 report that the endocrine consequences of immobilization are decreased serum PTH and decreased dihydroxyvitamin D synthesis. We observed elevation of PTH in 20% of cases, but we attribute it more to the 25(OH)D3 deficit than to immobilization, based on the correlation observed between PTH and 25(OH)D3. On the other hand, immobilization reduces PTH, as reported by Elias and Gwinup.26 Although 46% of the patients had an evident deficit in 25(OH)D3, the analysis of Ad-SOS in relation to vitamin D levels disclosed no differences. There also were no differences in relation to PTH. This suggests that the marginal reduction in Ad-SOS was due more to the loss of bone mass than to the existence of osteomalacia and/or secondary hyperparathyroidism.
In conclusion, using QUS we found that patients with paraplegia and an active life had a significant reduction in bone mass compared with a control group of similar age. This loss of bone mass cannot be related with levels of vitamin D, PTH and/or muscle tone. It seems to be related more to increased bone resorption than to deficient bone formation, as suggested by the elevation seen in TRAP and alkaline phosphatase.
References
Hancock DA, Reed GW, Atkinson PJ . Bone and soft tissue changes in paraplegic patients Paraplegia 1979 17: 267–271
Chantraine A, Heynen G, Franchimont P . Bone metabolism, parathyroid hormone, and calcitonin in paraplegia Calcif Tissue Int 1979 27: 199–204
Biering-Sorensen F, Bohr HH, Schaadt OP . Longitudinal study of bone mineral content in the lumbar spine, the forearm and the lower extremities after spinal cord injury Eur J Clin Invest 1990 20: 330–335
Garland DE, Stewart CA, Adkins RH, Hu SS, Rosen C, Liotta FJ, Weinstein DA . Osteoporosis after spinal cord injury J Orthop Res 1992 10: 371–378
Bauman WA, Zhong YG, Schwartz E . Vitamin D deficiency in veterans with chronic spinal cord injury Metabolism 1995 44: 1612–1616
Demirel G, Yilmaz H, Paker N, Onel S . Osteoporosis after spinal cord injury Spinal Cord 1998 36: 822–825
Bauman WA, Spungen AM, Adkins RH, Kemp BJ . Metabolic and endocrine changes in persons aging with spinal cord injury Assist Technol 1999 11: 88–96
Kocina P . Body composition of spinal cord injured adults Sports Med 1997 23: 48–60
Moynahan M, Betz RR, Triolo RJ, Maurer AH . Characterization of the bone mineral density of children with spinal cord injury J Spinal Cord Med 1996 19: 249–254
Frey-Rindova P, de Bruin ED, Stussi E, Dambacher MA, Dietz V . Bone mineral density in upper and lower extremities during 12 months after spinal cord injury measured by peripheral quantitative computed tomography Spinal Cord 2000 38: 26–32
Njeh CF, Boivin CM, Langton CM . The role of ultrasound in the assessment of osteoporosis: a review Osteoporos Int 1997 7: 7–22
Joly J, Westhovens R, Borghs H, Peeters H, Tirry J, Nijs J, Dequeker J . Reference curve and diagnostic sensitivity for a new ultrasound device for the phalanges, the DBMsonic 1200, in Belgian women Osteoporos Int 1999 9: 284–289
Ashworth B . Preliminary trial of carisoprodol in multiple sclerosis Practitioner 1964 192: 540–542
Rico H, Aguado F, Revilla M, Villa LF, Martin FJ . Ultrasound bone velocity and metacarpal radiogrammetry in hemodialyzed patients Miner Electrol Metab 1994 20: 103–106
Parfitt AM . Chlorothiazide induced hypercalcemia in juvenile osteoporosis and hyperparathyroidism New Engl J Med 1969 281: 55–59
Rico H, Villa LF . Serum tartrate-resistant acid phosphatase as a biochemical marker of bone remodeling Calcif Tissue Int 1993 52: 149–150
Descos L, Andre C, Beorghia S, Vincent C, Revillard JP . Serum levels of β2-microglobulin – a new marker of activity in Crohn's disease N Engl J Med 1979 301: 440–441
Scharla SH . Prevalence of subclinical vitamin D deficiency in different European countries Osteoporos Int 1998 8: Suppl 2 S7–S12
Jergas M, San Valentin R, Black M, Nevitt L, Palermo L, Genant HK, Cummings SR . Radiogrammetry of the metacarpals predicts future hip fracture: a prospective study J Bone Miner Res 1995 10: Suppl 1 475
Takada M, Engelke K, Hagiwara S, Grampp S, Jergas M, Gluer CC, Genant HK . Assessment of osteoporosis: Comparison of radiographic absorptiometry of the phalanges and dual X-ray absorptiometry of the radius and lumbar spine Radiology 1997 202: 759–763
Kleerekoper M, Nelson DA, Flynn MJ, Pawluszka AS, Jacobsen G, Peterson EL . Comparison of radiographic absorptiometry with dual-energy X-ray absorptiometry and quantitative computed tomography in normal older white and black women J Bone Miner Res 1994 9: 1745–1749
Cadossi R, Cane V . Pathways of transmission of ultrasound energy through the distal metaphysis of the second phalanx of pigs: an in vitro study Osteoporos Int 1996 6: 196–206
Bhate DV, Pizarro AJ, Seitam A, Mak EB . Axial skeletal changes in paraplegics Radiology 1979 133: 55–58
Nottage WM . A review of long-bone fractures in patients with spinal cord injuries Clin Orthop 1981 155: 65–70
Rafii M, Firooznia H, Golimbu C, Sokolow J . Bilateral acetabular stress fractures in a paraplegic patient Arch Phys Med Rehabil 1982 63: 240–241
Elias AN, Gwinup G . Immobilization osteoporosis in paraplegia J Am Paraplegia Soc 1992 15: 163–170
Pietschmann P, Pils P, Woloszczuk W, Maerk R, Lessan D, Stipicic J . Increased serum osteocalcin levels in patients with paraplegia Paraplegia 1992 30: 204–209
Naftchi NE, Viau AT, Sell GH, Lowman EW . Mineral metabolism in spinal cord injury Arch Phys Med Rehabil 1980 61: 139–142
Dauty M, Perrouin Verbe B, Maugars Y, Dubois C, Mathe JF . Supralesional and sublesional bone mineral density in spinal cord-injured patients Bone 2000 27: 305–309
Finsen V, Indredavik B, Fougner KJ . Bone mineral and hormone status in paraplegics Paraplegia 1992 30: 343–347
Haddad JG, Stamp TCB . Circulating 25-hydroxyvitamin D in man Am J Med 1974 57: 57–62
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Pedrera, J., Mañas, P., Gómez, M. et al. Ultrasound bone mass in paraplegic patients. Spinal Cord 40, 83–87 (2002). https://doi.org/10.1038/sj.sc.3101256
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101256
Keywords
This article is cited by
-
Vitamin D deficiency in individuals with a spinal cord injury: a literature review
Spinal Cord (2017)
-
Differential Bone Turnover in an Angulated Fracture Model in the Rat
Calcified Tissue International (2004)