Abstract
This study investigated the relationship between psychotherapeutic interventions and pharmacologic measures of pharmacotherapy treatment adherence in patients with bipolar I disorder, as well as the relationship between these measures and treatment outcome. Subjects were participating in an ongoing maintenance treatment study. Audiotaped therapy sessions were rated for frequency of psychotherapeutic interventions related to pharmacotherapy treatment adherence. Pharmacologic measures of medication adherence were compared to the tape ratings as well as to treatment outcome. Variability in log erythrocyte (RBC) lithium—a marker of probable nonadherence to the pharmacotherapy regimen—for individual patients correlated significantly with treatment adherence interventions scale ratings. This marker of nonadherence was significantly related to maintenance treatment outcome, as was variability of the serum lithium level/dose (L/D) ratio; however, no relationship was found between treatment adherence interventions scale ratings and outcome.
Similar content being viewed by others
Main
It is widely recognized that many people with bipolar disorder have difficulty adhering to prescribed medication (Goodwin and Jamison 1990; Cochran and Gitlin 1988; Cochran 1984; Jamison and Akiskal 1983). Estimates of lithium noncompliance range from 20% to 66% (Cochran and Gitlin 1988) in such patients. Psychotherapy is frequently employed as an adjunctive treatment strategy for bipolar disorder; however, it is not clear to what extent such intervention might enhance medication treatment adherence in this patient population. We hypothesized that therapists’ efforts targeted at enhancing pharmacotherapy treatment adherence would be associated with physiologic measures of treatment adherence and clinical outcome. Therefore, we initiated a study aimed at evaluating the outcome of therapists’ interventions directed toward pharmacotherapy treatment adherence, as reflected by both pharmacologic measures of treatment adherence and rates of episode recurrence.
METHODS
The Maintenance Therapies in Bipolar Disorder (MTBD-MH29618, E. Frank, Principle Investigator; Frank et al. 1999) study is an ongoing randomized trial of Interpersonal and Social Rhythm Therapy (IPSRT; Frank et al. 1994) versus an intensive clinical management (CM) control condition across both preliminary and preventative phases of treatment. Patients enter the study in the preliminary phase, during which acute treatment consisting of protocol pharmacotherapy and either IPSRT or CM is provided for their index episode of either mania or depression. Following recovery and 1 month of mood stability (defined by mean scores of ⩽7 and ⩽10 on the 17-item and 25-item versions of the Hamilton Depression Rating Scale (Hamilton 1960; Thase et al. 1992), respectively, and mean score of ⩽7 on the Bech-Rafaelsen Mania Scale (Bech et al. 1979, for a period of 4 weeks) patients enter in the preventative phase and are again randomized to either IPSRT or CM for maintenance treatment. Both treatment approaches include a standardized psychoeducational medication adherence training component early in the preliminary phase. Written informed consent was obtained from all participants in the MTBD study apprising them of both the study description and of the possible use of the data for additional research.
At the time this study was conducted, 155 patients had been entered into the MTBD protocol. Our initial eligibility criterion for inclusion in our study was that of having been in the maintenance phase of the MTBD study for at least 1 year. This led to a pool of 63 eligible patients. The resulting sample of patients was selected utilizing the following inclusion criteria: (1) three audiotaped, ratable sessions from the first 3 months of the preventative phase; (2) five blood level determinations [which we considered the minimum to estimate standard deviation (SD) with accuracy] within 8 months of beginning the preventative phase, three of which were required to be from the first 3 months in order to correspond with the time period of the selected audiotapes; (3) being treated with lithium; and (4) remaining clinically stable during the time period when all blood level data were collected. For patients who had recurrences, all data were collected prior to the time of recurrence. Reasons for tapes not being ratable included the following: occasionally malfunctioning equipment, taping errors by the clinicians, and lost or inaudible tapes. Of the original pool of 63 eligible patients, six could not be included based on criterion 1; 17 could not be included based on criterion 2; one could not be included based on criterion 3; and eight could not be included based on criterion 4. Outcome was categorized as either recurrence or completion of 2 years maintenance without recurrence. One additional patient who dropped out of the MTBD study before a categorizable outcome could be determined was excluded.
Thirty patients were eligible for inclusion in this study. For 29 of these, we obtained the criterion number of serum lithium levels for analyses, and for 20 of the 30 participants, the criterion number of erythrocyte (RBC) lithium levels were available. (The median number of clinical blood draws per outcome group during the first 8 months of the preventative phase was eight for completers and nine for patients with at least one recurrence). Our sample was comprised of 9 males and 21 females with a study entry age range of 19–63 years (mean ± SD = 36.6 ± 10.3, median = 37). Twenty-eight subjects were Caucasian, one was African-American and one was of Asian ethnic origin.
We developed a 12-item Likert-type scale, the Treatment Adherence Training Interventions Scale (TATIS; see Appendix), to measure therapists’ efforts spent on specific types of psychotherapeutic interventions pertaining to medication treatment adherence being performed with patients in both the IPSRT and the CM treatment groups. Four students were trained to rate audiotaped IPSRT and CM sessions using this scale. The mean score of three scale ratings for each patient was compared with the following objective pharmacologic measures of medication adherence that were based on data from five time points: (1) erythrocyte lithium variability (ELV) (Harvey and Kay 1991) (calculated as SD of the log of the RBC lithium content) and coefficient of variation (CV, calculated as [SD/mean] × 100) of log RBC lithium content; (2) SD and CV of clinically measured serum lithium level/dose (L/D) ratios. The correlation between TATIS scores and the pharmacologic measures of medication treatment adherence was assessed using the Spearman rho test. Patients who completed 2 years of maintenance treatment without experiencing a recurrent manic or depressive episode (DSM-IV criteria) (completers) were compared with those patients who had at least one recurrence (recurrers), on both pharmacologic measures of medication treatment adherence and TATIS scores, using the Mann-Whitney U-test. TATIS scores also were compared between patients in IPSRT treatment and those receiving clinical management using the Mann-Whitney U-test. Nonparametric tests were used because of small sample sizes and because the data were for the most part not normally distributed. Demographic and clinical variables for completers and recurrers were compared using chi-square or t-tests. Statistical analyses were performed using SPSS 9.0 for Windows (SPSS, Inc., Chicago, IL). All tests were two-tailed.
RESULTS
No statistically significant differences were found between completers (n = 16) and recurrers (n = 14) on the following demographic and clinical variables: proportion of males/females, study entry age, duration in weeks of index manic episode, duration in weeks of index depressive episode, baseline symptom severity, age at first mania, number of previous manic episodes, age at first depression, and number of previous depressive episodes (see Table 1. The Treatment Adherence Training Interventions Scale (TATIS) (Appendix A) mean score ratings (median = 1.33 scored points, range = 0–4.33) were significantly and positively correlated with the erythrocyte lithium variability measure, ELV (median = 0.095, range = 0.028–0.274 log mmoles Li/L RBCs; Spearman's rho = 0.50, p = .02), and were marginally associated with the coefficient of variation of log RBC lithium content (median = 25%, range = 6–53, Spearman's rho = 0.39, p = .09). TATIS scores were not significantly associated with either of the lithium L/D ratio-based measures (for SD of lithium L/D ratio, median = 0.09 mmoles/L/g, range = 0.04–0.33 mmoles/L/g, Spearman's rho = 0.16, p = .41; for CV of lithium L/D ratio, median = 13%, range = 7 – 44%, Spearman's rho = 0.077, p = .69).
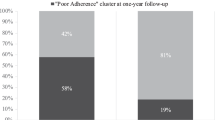
For the 20 subjects for whom the criterion number of RBC lithium levels were available: ELV was significantly greater (see Figure 1), and CV of log RBC lithium content was borderline significantly greater, in the seven patients who had at least one recurrent episode (median time to recurrence from maintenance randomization = 42.4 weeks) compared to the 13 patients who remained stable (for SD-based-ELV, median = 0.143 vs 0.076 log mmoles Li/L RBCs, respectively; Mann-Whitney U=16, p = .02; for CV, median = 32 vs 17%, respectively, Mann-Whitney U = 21, p = .05). These measures indicated that greater variability of measured RBC lithium was significantly associated with recurrent episodes.
For the 29 subjects for whom the criterion number of serum lithium levels were available: both the SD and CV (see Figure 2) of patients’ lithium L/D ratios were significantly greater in the 14 patients who had at least one recurrence than in the 16 patients who remained episode-free (for SD, median = 0.13 vs 0.07 mmoles/L/g, respectively, Mann-Whitney U = 47, p = .01; for CV, median = 19 vs 9%, respectively; Mann-Whitney U = 32, p < .001), suggesting that greater variability of serum lithium is also significantly associated with recurrence risk. No relationship was found between TATIS scores and either outcome (median = 1.17 for completers vs 1.67 for recurrers; Mann-Whitney U = 98, p = .58) or maintenance treatment assignment (median = 1 for IPSRT vs 1.33 for CM; Mann-Whitney U = 87.5, p = .31).
DISCUSSION
Results of this study provide further evidence that recurrence risk during preventative phase therapy of bipolar disorder is directly linked to nonadherence with prescribed therapy. Harvey and Kay (1991) previously examined the log RBC lithium content in relation to episode recurrence, and found ELV to be a useful parameter that was correlated with treatment outcome. They argue that logarithmic transformation of the RBC lithium level better allows for interindividual comparisons. Our observation of significantly higher ELV for those patients who suffered recurrences generally confirms Harvey and Kay's results.
The association between nonadherence and recurrence risk is particularly noteworthy because this study dealt with a relatively highly motivated and carefully selected group of patients. Moreover, by focusing on lithium responsive patients participating in a longitudinal protocol for at least one year, it is likely that highly nonadherent patients were already removed from the case mix. Thus, it appears that even a moderate degree of nonadherence has a significantly negative impact on longer term outcome.
There are very few existing studies specifically focusing on psychotherapeutic approaches to improving treatment adherence in patients with bipolar disorder. Cochran (1984) investigated the efficacy of a preventative treatment adherence intervention involving six weekly individual sessions focused on altering patients’ cognitions and behaviors. This model was found to significantly reduce patient hospitalizations, terminations of lithium against medical advice, and the number of nonadherence-precipitated affective episodes. However, Cochran noted that objective measures of lithium nonadherence did not yield significant results, possibly due to missing or incomplete blood test data. The Treatment Adherence Training Interventions Scale was significantly and positively associated with ELV, thereby relating higher frequency of compliance-related interventions with greater variability of RBC lithium. This suggests that clinicians recognize when at least some patients are not adhering to their pharmacological treatment and attempt to intervene. Although it is possible that outcomes would have been even worse if no such interventions were attempted, our findings suggest that these interventions had limited effectiveness. Thus, more intensive approaches to enhancing medication adherence are needed. Another possible treatment approach for enhancing pharmacotherapy treatment adherence in this patient population might involve some of the motivational interviewing techniques being used in the treatment of substance abuse (Miller and Rollnick 1991).
The finding that the CV of the lithium L/D ratio relates to clinical outcome differs from a previously published negative observation derived from a sample partially overlapping the one presented here (Mallinger et al. 1997). We believe this reflects differences in the subject population and sample timing. The earlier investigation done by Mallinger and colleagues included early recurrences and dropouts who would not have met the inclusion criteria utilized in the present report. Moreover, only the first year of maintenance treatment was investigated in the earlier report; some patients who successfully completed this first year subsequently had recurrences during the second year. Another methodological difference is that the earlier investigation used different time points for the lithium L/D ratio observations, including some from acute treatment prior to mood stabilization. The present findings must be interpreted in the context of these differences.
Therapists’ efforts spent on treatment adherence enhancement interventions were low across all patients (median = 2.33, range = 0–4.33, for mean score TATIS ratings, out of a possible maximum mean score of 45). This raises the general question of whether enough time was focused on treatment adherence during maintenance treatment. Further inquiry in this area might look at the therapist efforts spent on such interventions during the preliminary phase of treatment.
A limitation to this study was that lithium measurements were not available for all subjects from the larger study. Specifically, 17 patients from the larger study were excluded because they lacked the required number of blood samples from the time of interest. Excluding subjects because of missing blood sample data not only reduced statistical power but also adversely reduced design sensitivity because it is likely that patients who missed scheduled blood draws were also less adherent to prescribed medications. It is therefore suggested that future research in this area employ additional methods to measure treatment adherence behaviors, such as recording the number of canceled or missed appointments and using pill container devices that directly monitor medication access.
While our variability measures of both serum lithium L/D ratios and RBC lithium content were shown to be predictive of patient outcome, our investigation did not look at other important indicators of pharmacotherapy management and treatment adherence, such as the individual serum lithium levels themselves or clinical evaluation of patients’ medication-taking behaviors. Hence, we are unable to make an empirical comparison between our use of lithium level variability and other currently utilized measures of pharmacotherapy treatment adherence. However, a question that we hope to address in future investigations is whether the variability measurement approach will prove to be a useful adjunct to currently used clinical methodologies, since it provides a definable method for interpreting drug level data that may otherwise be difficult to quantify, especially in cases where a patient's individual lithium levels do not demonstrate a clear pattern.
These findings, although preliminary and based on a small sample, suggest that RBC and/or serum lithium variability measures may be utilized as a benchmark means of identifying patients who are at increased risk for recurrence, presumably because of inadequate treatment adherence. Patients identified by these means might then be targeted for improved clinical interventions aimed at enhancing treatment adherence. In this way, the overall success of bipolar disorder treatment might be improved.
References
Bech P, Bolwig TG, Kramp P, Rafaelson OJ . (1979): Bech-Rafaelsen Mania Scale and the Hamilton Depression Scale. Acta Psychiatrica Scandinavica 59: 420–430
Cochran SD . (1984): Preventing medical noncompliance in the outpatient treatment of bipolar affective disorders. J Consult Clin Psychol 52: 873–878
Cochran SD, Gitlin MJ . (1988): Attitudinal correlates of lithium compliance in bipolar affective disorders. J Nervous Mental Dis 176: 457–464
Frank E, Kupfer DJ, Ehlers CL, Monk TH, Cornes CL, Carter S, Frankel DR . (1994): Interpersonal and social rhythm therapy for bipolar disorder, integrating interpersonal and behavioral approaches. Behav Ther 17: 143–149
Frank E, Swartz H, Mallinger A, Thase M, Weaver EV, Kupfer DJ . (1999): Adjunctive psychotherapy for bipolar disorder: Effects of changing treatment modality. J Abnormal Psychol 108: 579–587
Goodwin FK, Jamison KR . (1990): Manic Depressive Illness. New York, NY, Oxford University Press
Hamilton M . (1960): A rating scale for depression. J Neurol Neurosurg Psychiat 23: 56–62
Harvey NS, Kay R . (1991): Compliance during lithium treatment, intra-erythrocyte lithium variability, and relapse. J Clin Psychopharmacol 11: 362–367
Jamison KR, Akiskal HS . (1983): Medication compliance in patients with bipolar disorder. Psychiat Clin N Am 6: 175–192
Mallinger AG, Frank E, Thase ME, Dippold CS, Kupfer DJ . (1997): Low rate of membrane lithium transport during treatment correlates with outcome of maintenance pharmacotherapy in bipolar disorder. Neuropsychopharmacology 16: 325–332
Miller WR, Rollnick S . (1991): Motivational Interviewing: Preparing People to Change Addictive Behavior. New York, NY, Guilford Press
Thase ME, Frank E, Mallinger AG, Hamer T, Kupfer DJ . (1992): Treatment of imipramine-resistant recurrent depression, III: Efficacy of monoamine oxidase inhibitors. J Clin Psychiat 53: 5–10
Acknowledgements
This study was supported, in part, by National Institute of Mental Health grants MH-29618 and MH-30915.
Author information
Authors and Affiliations
Corresponding author
Additional information
Presented in part at the Third International Conference on Bipolar Disorder, Pittsburgh, PA, June 17–20, 1999
Appendix 1
Appendix 1
Rights and permissions
About this article
Cite this article
Taylor, R., Mallinger, A., Frank, E. et al. Variability of Erythrocyte and Serum Lithium Levels Correlates with Therapist Treatment Adherence Efforts and Maintenance Treatment Outcome. Neuropsychopharmacol 24, 192–197 (2001). https://doi.org/10.1016/S0893-133X(00)00200-1
Received:
Revised:
Accepted:
Issue Date:
DOI: https://doi.org/10.1016/S0893-133X(00)00200-1
Keywords
This article is cited by
-
Stress, social rhythms, and behavioral activation: Psychosocial factors and the bipolar illness course
Current Psychosis & Therapeutics Reports (2004)
-
Stress, social rhythms, and behavioral activation: Psychosocial factors and the bipolar illness course
Current Psychiatry Reports (2003)