Abstract
S(-)3-amino-1-hydroxypyrrolidone-2 (S(-)HA-966), a potent γ-hydroxybutyrate-like drug, inhibits spontaneous firing and induces a pacemaker-like discharge pattern in nigral dopamine (DA)-containing neurons. Recent evidence has suggested that these effects could be mediated by GABAB receptors and, thus, is likely to involve G protein intermediaries. To test this hypothesis, extracellular single-unit recording techniques were used to assess the effects of S(-)HA-966 in animals that had received an intranigral injection of pertussis toxin (PT). Failure to respond to the inhibitory effects of apomorphine was taken as presumptive evidence that PT-sensitive G protein-coupled receptors had been inactivated. No significant differences were observed in the basal firing properties of DA cells recorded in control and PT-lesioned animals. However, in marked contrast to the inhibitory effects observed in uninjected and sham-lesioned animals, S(-)HA-966 significantly increased the firing rate of apomorphine-insensitive DA neurons in PT-lesioned rats. The excitatory effects of S(-)HA-966 were accompanied by a significant reduction in bursting activity and an increase in the regularity of firing. These data indicate that the inhibitory effects of S(-)HA-966 are mediated locally within the substantia nigra by a PT-sensitive substrate, presumably a G protein-coupled receptor.
Similar content being viewed by others
Main
3-amino-1-hydroxypyrrolidone-2 (HA-966) is a four carbon, chiral hydroxamate structurally similar to the lactone form of γ-gamma-hydroxybutyrate (GHB). Not surprisingly, HA-966 and GHB share nearly identical neurochemical, electrophysiological, and behavioral profiles (Bonta et al. 1971; Singh et al. 1990; Waldmeier 1991; Engberg and Nissbrandt 1993; Shepard et al. 1995). Both compounds have sedative, anxiolytic, and antispasmotic properties, although neither is in widespread clinical use in the United States because of their ability to induce EEG changes in animals similar to those observed in human absence epilepsy (Bonta et al. 1971; Snead, 1988). However, recent clinical data showing that GHB is effective in suppressing alcohol and opiate withdrawal (Gallimberti et al. 1992, 1993) and that S(-)HA-966 can prevent cocaine sensitization in rats (Morrow et al. 1997) and attenuate PCP-induced changes in dopamine (DA) metabolism in the primate prefrontal cortex (Jentsch et al. 1997) has rekindled interest in the potential therapeutic applications of these compounds.
GHB and HA-966 produce marked alterations in the activity of mesencephalic DA-containing neurons. In the chloral hydrate anesthetized rat, both drugs are capable of reversibly suppressing impulse flow leading to a compensatory increase in DA levels in terminal field areas, including the dorsal and ventral striatum (Gessa et al. 1966; Hillen and Noach 1971; Roth et al. 1973; Shepard and Lehmann 1992). S(-)HA-966 is considerably more potent in this regard than either GHB or the R(+) enantiomer of HA-966, which also exhibits affinity for the glycine allosteric site on the N-methyl-D-aspartate (NMDA) receptor (Singh et al. 1990). The inhibitory effects produced by lower doses of GHB (⩽ 200 mg/kg) and S(-)HA-966 (⩽10 mg/kg) are accompanied by a complete cessation of bursting activity and the emergence of a pacemaker-like firing pattern that is not typically observed in vivo (Engberg and Nissbrandt 1993; Shepard et al. 1995). Evidence indicating that bursting activity is an important mechanism for modulating DA release (reviewed by Overton and Clark 1997) has led to speculation that some of the behavioral effects of these drugs (i.e., anxiolytic activity) could stem from their effects on neuronal firing pattern.
GHB, a naturally occurring metabolite of GABA, satisfies several of the criteria ascribed to endogenous neurotransmitters, including its own receptor/binding site (Maitre 1997). However, recent evidence suggests that the effects of the compound are mediated through an interaction with GABAB receptors. For example, GHB-induced increases in oscillatory firing of thalamocortical neurons together with the resultant “spike and wave” EEG discharge characteristic of absence seizures are blocked by the GABAB receptor antagonist, CGP 35348 (Snead 1992; Williams et al. 1995). Changes in the firing rate and discharge pattern of nigral DA neurons following GHB are also blocked by systemic administration of CGP-35348 (Engberg and Nissbrandt 1993; Erhardt et al. 1998) as are the increases in DA levels and synthesis in the forebrain (Waldmeier 1991; Nissbrandt and Engberg 1996). Likewise, the inhibitory effects of S(-)HA-966 on nigral DA neurons both in vivo and in vitro are fully antagonized by CGP-35348 and 2-hydroxysaclofen (Shepard et al. 1995; Grobaski et al. 1997). These data are consistent with earlier findings showing that GABAB antagonists also attenuate the increase in DA synthesis produced by S(-)HA-966 (Waldmeier 1991).
Despite the data summarized above, binding studies indicate that neither GHB nor HA-966 possess appreciable affinity for GABAB receptors. Using [3H]baclofen as a radioligand and membranes prepared from rat cerebral cortex, Bernasconi et al. (1992) initially reported that GHB binds only weakly to these receptors with an IC50 of 150 μM. Moreover, when valproate is added to block its degradation to GABA, GHB is without affect on GABAB binding, regardless of the technique used for membrane preparation (Hechler et al. 1997). GHB, in concentrations as high as 1 mM, is also ineffective in displacing [3H]GABA from GABAB receptors using autoradiographic binding techniques (Snead 1996). S(-)HA-966 also fails to exhibit appreciable affinity for GABAB receptors. Binding assays in which [3H]GABA is used in combination with saturating concentrations of isoguvacine to block binding to GABAA receptors, indicate that the potency of S(-)HA-966 relative to GABA is approximately 0.0005, and binding is not stereoselective (Grobaski et al. 1997). Morrow et al. (1997), using [3H](-)baclofen as a radioligand, estimated the IC50 of S(-) and R(+)HA-966 at 200 and 350 μM, respectively. Notably, although GHB and S(-)HA-966 exhibit nearly identical potency as putative GABAB receptor agonists in binding assays, S(-)HA-966 is over 200 times more potent than GHB in altering DA neuronal activity. This has prompted several investigators to question the involvement of GABAB receptors as sole mediators of the biochemical, electrophysiological, and behavioral effects of GHB and S(-)HA-966 (Grobaski et al. 1997; Morrow et al. 1997).
Although GABAB receptors couple to a variety of transduction mechanisms, their inhibitory postsynaptic effects are mediated primarily by activation of an inwardly rectifying K+ channel (Newberry and Nicoll 1984; Gähwiler and Brown 1985; Misgeld et al. 1995; Lüscher et al. 1997). Unlike their ionotropic counterparts, metabotropic GABAB receptors exert their effects indirectly through activation of the guanine nucleotide binding proteins, G0 and Gi (Andrade et al. 1986; Thompson and Gähwiler 1992). Pertussis toxin (PT), a compound that inactivates Gi/o proteins via ADP-ribosylation, blocks the postsynaptic actions of the GABAB agonist baclofen on a variety of neurons (reviewed by Reisine 1990; Misgeld et al. 1995). PT has also been shown to prevent absence seizures induced by GHB, an effect that has been attributed to an increase in a GABAB receptor-mediated K+ conductance in thalamocortical neurons (Williams et al. 1995). Although it is not yet known whether PT blocks the inhibitory effects of GHB on DA neurons, recent studies have shown that the drug increases a K+ conductance in these cells that can be antagonized by CGP-35348 (Madden and Johnson 1998).
The marked similarity between the physiological and pharmacological profile of GHB and S(-)HA-966 strongly suggest that these drugs share a common mechanism of action. Although recent studies support the involvement of G protein-coupled receptors in mediating the inhibitory effects of GHB, it is currently unknown whether a similar mechanism contributes to the nearly identical effects produced by S(-)HA-966. In the present group of experiments, local injections of PT were used to assess the role of nigral Gi/o proteins in mediating the electrophysiological effects of S(-)HA-966 on DA-containing neurons.
MATERIALS AND METHODS
Animals
All experiments were performed using adult, male Sprague–Dawley rats (280–350 g, Dominion Laboratories, Dublin, VA). Animals were housed in a temperature-controlled vivarium under scheduled lighting conditions and provided unrestricted access to food and water. All experiments were conducted in strict accordance with the procedures outlined in the Guide for the Care and Use of Laboratory Animals as adopted and promulgated by the National Institutes of Health and the University of Maryland School of Medicine.
Intercerebral Injections
With the exception of a small group of control subjects (n=5), all animals used in these experiments received intranigral injections of PT (1 μg in 1 μl) or an equivalent volume of vehicle (0.1 M phosphate buffer containing 0.5 M NaCl). Rats were anesthetized with chloral hydrate (400 mg/kg, IP) and mounted in a stereotaxic apparatus. A small incision was made in the scalp and a burr hole drilled in the skull overlying the substantia nigra (4 mm anterior to the lambdoid suture and 2 mm lateral to the midline). Injection cannula were prepared from a 4-cm length of 30-gauge stainless steel tubing (HTX-30, Small Parts Inc., Miami, FL) and beveled to a 45° angle. Thick-walled polyethylene tubing (PE-20) was used to connect the cannula to a 10 μl gas-tight Hamilton syringe. Cannula were stereotaxically positioned in the ventral–anterior region of the substantia nigra using coordinates from the Koenig and Klippel (1963) Rat Brain Atlas (2.4 mm anterior to ear bar zero, 2.5 mm lateral to the midline, 8–8.5 mm ventral to cortical surface). A hydraulic microdrive was used to position the injection cannula, which enabled it to be withdrawn slowly (3–5 μm s−1) to minimize backflow up the needle track. Injections were made using a BAS microdialysis pump programmed to deliver a 1 μl volume at 0.1 μl/min. All injections were made on the right side of the brain. Cannula were removed 2 to 3 minutes following the injection, and a small piece of gelfoam soaked in sterile saline was placed over the burr hole before closing the wound margins with surgical staples.
Single-Unit Recording Techniques
Electrophysiological experiments were performed approximately 48 hours following intranigral injections. Rats were anesthetized with chloral hydrate (400 mg/kg, IP), and the right femoral vein was cannulated for intravenous (IV) administration of supplementary anesthetic and experimental drugs. Soft tissues surrounding the ear canals and wound margins were infiltrated with a long-acting local anesthetic (2% mepivacaine) before positioning the animal in a stereotaxic frame (Kopf, Tujunga, CA). Body temperature was maintained at 36.5°C using a feedback-controlled heating unit (Fintronix, Orange, CT).
Neuronal activity was recorded extracellularly using epoxy-coated tungsten microelectrodes (FHC Corp. Brunswick, ME) ranging in impedance from 2.5 to 5 MΩ at 135 Hz). Electrodes were stereotaxically positioned within the zona compacta of the substantia nigra using coordinates obtained from the Koenig and Klippel (1963) Rat Brain Atlas—1.6 to 2.2 mm anterior to ear bar zero, 6.8 to 8 mm ventral to cortical surface, and 1.5 to 3 mm lateral to the midline. Electrode potentials were amplified, filtered (0.1–400 kHz bandpass) and monitored visually and aurally. Well-isolated units were identified as dopaminergic on the basis of their location and unique electrophysiological characteristics including long-duration (> 2.5 ms) triphasic action potentials, slow firing rates (1–8 Hz), and irregular single spike or burst firing discharge pattern (Bunney et al. 1973; Grace and Bunney 1984). Individual spikes were isolated from background noise using a window discriminator (Fintronix, Orange, CT), the output of which was directed to a PC-based data acquisition system that displayed firing rate data in real time while simultaneously storing interspike interval (ISI) data for analysis off-line (RISIPS, Symbolic Logic, Dallas, TX).
Experimental Design and Data Analysis
Studies were designed to compare the effects of S(-)HA-966 on the spontaneous activity of nigral DA-containing neurons in three groups of animals including uninjected (n = 5), sham-injected (n = 14), and PT-lesioned (n = 16) rats. Single-unit activity was recorded for 5 to 10 min to establish the basal firing properties of the cell. Each animal then received a single injection of the ID50 dose of S(-)HA-966 (6 mg/kg, IV; Shepard et al. 1995). A cumulative dosing protocol could not be used because of the slow onset of the effects of the drug (Shepard and Lehmann 1992; Shepard et al. 1995). Within 20 minutes following the initial dose of S(-)HA-966, animals received an injection of apomorphine (40 μg/kg, IV) followed by haloperidol (0.1 mg/kg). Only one cell was tested per animal. Spike trains comprising 1,000 consecutive action potentials were used to assess drug-induced changes in firing rate and discharge pattern. Data were collected immediately before the first injection and again following the development of a stable level of activity representing the maximal effects of S(-)HA-966. First-order ISI histograms were compiled and used to compute the variation coefficient (standard deviation of the ISI distribution expressed as a percentage of the mean interval). This statistic has been used successfully to quantify changes in firing pattern of cells with unequal firing rates (Werner and Mountcastle 1963). ISI data were also analyzed for evidence of bursting activity using the burst detection parameters developed and validated by Grace and Bunney (1984). Briefly, bursts were identified as spike pairs with an ISI ⩽ 80 ms. Subsequent spikes were considered as part of the initial burst unless an interval exceeding 160 ms was encountered that signaled burst termination. Although spike doublets were counted as bursts, six bursts comprising a minimum of three spikes/burst were required to meet the operational definition of bursting activity. All data are expressed as the arithmetic mean ± standard error of the mean (SEM). Comparison of group means was made using a paired t- (within-group comparisons) or Student's t-test (between-group comparisons). All p values were derived from two-tailed probability distributions.
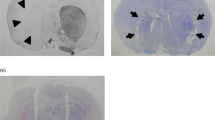
Localization of Recording and Injection Sites
At the conclusion of each experiment, the position of the tip of the recording electrode was marked by application of a small direct current (+20 μA for 30 s). Following removal from the stereotaxic apparatus, animals were deeply anesthetized and perfused transcardially with saline followed by 10% neutral buffered formalin. Coronal sections (40 μm) were cut on a freezing microtome and stained with cresyl violet. Sections were examined microscopically to verify that the injection and recording sites were localized within the substantia nigra.
Drugs
Chloral hydrate and apomorphine were obtained from Sigma (St. Louis, MO). Haloperidol was obtained from McNeil Laboratories in injectable form. S(-)HA-966, baclofen, and PT were purchased from RBI (Natick, MA). CGP-35348 was generously donated by Ciba-Geigy Pharmaceuticals (Basal, Switzerland). All drugs were reconstituted or diluted to their final concentration in sterile distilled water.
RESULTS
Effects of S(-)HA-966 on DA Neuronal Activity in Uninjected and Sham-Injected Rats
Intravenous administration of a single dose of S(-)HA-966 (6 mg/kg, IV) inhibited the firing rate of all cells recorded in uninjected (n = 5) and sham-injected (n = 14) rats. Cells in both groups exhibited similar basal firing rates (uninjected: 4.1 ± 0.2 Hz; sham-injected: 3.8 ± 0.3 Hz; Student's t, p > .5) and were equally sensitive to the rate-decreasing effects of the drug (% control firing: uninjected: 61.5 ± 5.7%; sham-injected: 54.3 ± 7.6%, Student's t, p > .5). As previously reported (Shepard et al. 1995), DA cells occasionally showed a biphasic response to S(-)HA-966, consisting of an initial increase in firing rate followed by a sustained inhibition (Fig. 1A). Neither the magnitude of the transient excitation (∼ 30%) nor the proportion of cells showing the biphasic response (∼ 30%) varied between the two control groups. The inhibitory effects of S(-)HA-966 were associated with a pronounced change in the temporal organization of neuronal spike trains (Figure 1B,C, D). Predrug firing patterns, which ranged from an irregular single spike to a multiple spike bursting discharge, became uniformly pacemaker-like following the drug, resulting in an 83.7 ± 5.2% and 76.3 ± 6.2% decrease in the variation coefficient of uninjected and sham-injected rats, respectively. Bursting activity, when present, was completely suppressed by the drug. Because uninjected and sham-injected rats exhibited an identical response to S(-)HA-966, these groups were combined to form a single control group for comparison with PT-lesioned animals.
Effect of S(-)HA-966 on the firing properties of a representative DA-containing neuron in a sham-injected rat. (A) Cumulative rate histogram depicting the actions of a single IV injection of S(-)HA-966 (6 mg/kg) on neuronal firing rate. Note the transient increase in activity immediately following injection. Subsequent administration of the DA agonist apomorphine (apo, 40 mg/kg) completely inhibits spontaneous activity, which is then fully restored by haloperidol (halo, 0.1 mg/kg). Horizontal bars above rate histogram denote areas used to compile the ISI histograms. (B) to (C): First-order ISI histograms compiled (B) immediately prior to and (C) 15 min after injection of S(-)HA-966. Note the marked reduction in variability of the interval distribution, which necessitated changing the vertical scale of the histogram. (D) Raster diagram illustrating a 25-second sample of contiguous intervals used to construct the histograms presented in (C) and (D). Tick marks represent individual spikes. Note the highly regular firing pattern exhibited by the cell following S(-)HA-966
Effects of Intranigral PT on the Basal Firing Properties of DA Neurons
A total of 16 animals received intranigral injections of PT, 48 hours before onset of the recording studies. Injection coordinates targeted the anterior regions of the substantia nigra pars reticulata, approximately 1.2 mm rostral to the planned recording sites (Innis and Aghajanian 1987). Electrode tracts were always made caudal to the injection site and were presumed to have entered tissue regions that had been exposed to PT. However, because it was not possible to control the spread of the injection, no assumptions could be made a priori whether the concentration of the toxin at the recording site had reached levels sufficent to inactivate Gi/o fully. To assess the functional status of G proteins in PT-injected rats, individual DA neurons that had previously been treated with S(-)HA-966 were challenged with a single dose of the DA agonist, apomorphine. The inhibitory effects of apomorphine are known to be mediated by D2 autoreceptors that couple to inwardly rectifying K+ channels via a PT-sensitive G protein (Baring et al. 1980; Innis and Aghajanian 1987; Akaoka et al. 1992; Kim et al. 1995). Cells that failed to respond to the agonist were considered to have been exposed to a local concentration of PT sufficient to inactivate G protein-coupled receptors. The dose selected for testing (40 μg/kg, IV) was eight- to tenfold higher than the ID50 dose of the drug in chloral hydrate anesthetized rats (Martin et al. 1990; Kreiss et al. 1995) and was sufficient to rapidly and completely inhibit the spontaneous activity of all DA neurons recorded in uninjected and sham-injected rats (Figure 1A). Of the 16 cells recorded in PT-injected rats, 12 were unaffected by the DA agonist. The remaining four neurons were completely inhibited in response to the apomorphine challenge and were excluded from all statistical comparisons with cells recorded in control animals.
The distribution of control firing rates and predrug discharge patterns obtained from both control and apomorphine-insensitive DA neurons recorded in PT-injected rats are illustrated in Figure 2. The average basal firing rate was not significantly different between groups (control: 3.9 ± 0.2 Hz, PT-injected: 3.5 ± 0.2 Hz, Student's t, p > .2). Firing pattern, although slightly more variable in the PT-lesioned group (variation coefficient: 63.9 ± 5.1%), also did not differ significantly from control values (53.0 ± 4.8%; Student's t, p > .1). In addition, the number of cells that satisfied the operational definition of burst firing was comparable between control (9/19) and PT-lesioned groups (7/12).
Scattergram illustrating the distribution of spontaneous firing rates and discharge patterns of DA neurons recorded in control (n = 19) and PT-lesioned rats (n = 12). Each point represents a single cell. Control values were obtained from uninjected and sham-lesioned rats. Average firing rates (A) and variation coefficients (B) were computed immediately before administration of S(-)HA-966. Circles represent cells with an irregular single-spike discharge; triangles are neurons that met the operational definition of bursting activity. Horizontal lines represent the arithmetic mean. No significant differences were observed in the firing rate, variation coefficient, or incidence of bursting activity between cells in control and PT-lesioned rats
Effects of S(-)HA-966 on DA Neuronal Activity in PT-Injected Rats
The effect of S(-)HA-966 on the activity of an apomorphine-insensitive DA neuron recorded in a PT-lesioned rat is illustrated in Figure 3A. In marked contrast to the inhibitory effects of the drug observed in control animals, a single IV injection of 6 mg/kg of S(-)HA-966 resulted in a sustained increase in neuronal firing rate. Identical effects were observed in 11 of 12 apomorphine-insensitive neurons. By contrast, the four cells recorded in PT-lesioned animals that remained sensitive to the inhibitory effects of apomorphine exhibited a significant reduction in firing in response to S(-)HA-966 (Fig. 3B).
Effect of S(-)HA-966 on the firing rate of DA-containing neurons in PT-lesioned rats. (A) Representative rate histogram illustrating the excitatory effects of S(-)HA-966 on an apomorphine-insensitive DA neuron recorded in a PT-lesioned rat. Excitatory effects, similar to those illustrated in this example, were observed in 11/12 cells subsequently shown to be refractory to the inhibitory effects of apomorphine (apo). (B) Recording obtained from a PT-lesioned animal in which baclofen (bac) and apomorphine (apo) reversibly suppressed neuronal activity. 4/16 neurons recorded in PT-lesioned animals remained sensitive to apomorphine and were excluded from the statistical analysis. In each of these cells, the effects of S(-)HA-966 was inhibitory. Horizontal bars indicate the range of data used to compile the interspike interval histograms presented in Figure 5
S(-)HA-966 significantly increased the firing rate of apomorphine-insensitive DA cells (predrug: 3.5 ± 0.2 Hz; postdrug: 4.4 ± 0.3 Hz, paired t(11) = 3.5 p < .005; Figure 4A). In contrast, cells recorded in the pooled control group were significantly inhibited by the drug (predrug: 3.9 ± 0.2 Hz, postdrug: 2.1 ± 0.2 Hz, paired t(18) = 5.6, p < .0001). Despite the increase in firing rate observed in PT-lesioned animals, firing pattern became significantly more regular following S(-)HA-966 (variation coefficient, predrug: 63.9 ± 5.1%; postdrug: 37.2 ± 5.8%, paired t(11) = 4.2, p < .002, Figure 4B). However, the pattern-regularizing effects of S(-)HA-966 in PT-lesioned rats were less pronounced than those observed in control cells (variation coefficient, predrug: 49.8 ± 5.3%, postdrug: 8.9 ± 1.7, paired t(15) = 7.7, p < .0001; Figure 5A). The number of cells comprising the control group used to compare drug-induced changes in firing pattern (n = 16 was less than that used to compare the basal firing properties of control and PT-lesioned cells (n = 19) because three control neurons were completely inhibited by S(-)HA-966. Burst firing, which was evident in 7/12 PT-lesioned cells, was also significantly reduced by the drug (% spikes in bursts, predrug: 39.6 ± 8.7%; postdrug: 7.6 ± 2.7%; paired t(6) = 3.1, p < .05). However, in marked contrast to control cells, in which bursting was completely eliminated by S(-)HA-966, 4/7 bursting cells in PT-lesioned animals continued to meet the operational definition for burst-firing following the drug.
Effects of S(-)HA-966 on the firing rate and discharge pattern of nigral DA-containing neurons in control and PT-lesioned rats. Data were collected immediately before (open bars) and 15 min following (crosshatched bars) a single 6 mg/kg dose of the drug and are expressed as the mean ± SEM. Statistical comparison of pre- and postdrug values was accomplished using a paired t-test (*** p < .0001; ** p < .005)
Effects of S(-)HA-966 on the firing pattern of nigral DA neurons recorded in PT-lesioned rats. (A) to (C) Apomorphine-insensitive cell. Data were obtained from the rate histogram illustrated in Figure 3A. First-order ISI histograms compiled immediately before (A) and 15 min following (B) a 6 mg/kg dose of S(-)HA-966. C: Raster diagram illustrating a 25-second sample of contiguous intervals used to compile the histograms presented in (A) and (B). Tick marks represent individual spikes. Note that, although there is evidence of an increase in the regularity of firing, the variation coefficient increases attributable to the variance introduced by the irregular intervals interposed between episodes of regular spiking. (D) to (E) ISI histograms obtained from the cell illustrated in Figure 3B immediately before (D) and 15 minutes following (-)HA-966 (E). (F) Raster diagram of a sample of the intervals used to compile the histograms shown in (D) and (E). Cells recorded in PT-lesioned rats that remained sensitive to apomorphine showed a significant increase in regularity of firing identical to that seen in control neurons
DISCUSSION
S(-)HA-966 has previously been shown to inhibit the spontaneous activity of nigral DA neurons (Shepard and Lehmann 1992). Subsequent studies showing that these effects are reversed by CGP-35348 and 2-hydroxysaclofen suggest that GABAB receptors contribute to this response (Shepard et al. 1995; Grobaski et al. 1997). In contrast, binding studies have consistently indicated that S(-)HA-966 has no appreciable affinity for these receptors. The results of the present study have extended these findings by demonstrating that the inhibitory effects of S(-)HA-966 involve a PT-sensitive substrate and, thus, could be mediated by the same family of G protein-coupled receptors that underlie the inhibitory effects of GHB and baclofen.
Technical Considerations
Sensitivity to PT is widely regarded as presumptive evidence that a response is mediated via G protein-coupled receptors (Reisine 1990; Misgeld et al. 1995). The toxin acts by ADP-ribosylating a cysteine residue on the α subunit of Gi/o, uncoupling the receptor from its effector. In the present study, we chose to deliver PT directly into the substantia nigra, as opposed to an interventricular route, both in an effort to restrict its actions to the ventral midbrain and to increase the likelihood that tissue concentrations would reach levels sufficient to ensure maximal ribosylation. The principal disadvantage of this approach is the potential for mechanical disruption of the tissue in the vicinity of the injection site. For this reason, cannulae were positioned ventral to the pars compacta of the substantia nigra, and recordings were made at a minimum of 1.2 mm caudal to the injection site. To assess the potential confound introduced by tissue damage resulting from intracerebral injections, the effects of S(-)HA-966 were compared between uninjected rats and animals that received an intranigral injection of the PT vehicle. Both groups of control animals showed an identical response to the drug, making it unlikely that nonspecific effects contributed to the actions of S(-)HA-966 in PT-lesioned rats. DA neurons in both control groups also exhibited a typical response to systemic administration of apomorphine and haloperidol, further evidence that the cells had not been injured during the PT injections. In contrast, the majority of cells recorded in PT-lesioned rats (12/16) were refractory to the DA agonist. Because the inhibitory effects of apomorphine are mediated through a PT-sensitive mechanism (Innis and Aghajanian 1987), failure to respond to the drug was taken as prima facie evidence that G proteins had been inactivated. This method was deemed to provide a more direct way of assessing the functional status of Gi/o in individual neurons than conventional biochemical estimates of “back-ribosylation” in tissue samples.
PT Fails To Alter the Basal Firing Properties of Nigral DA Neurons
In addition to modulating the effects of DA and GABA at D2 and GABAB receptors, respectively, PT-sensitive G proteins couple to receptors that mediate the effects of a variety of endogenous neurotransmitters and modulators, including angiotensin, endogenous cannabinoids, galanin, melatonin, NPY, opioid peptides, somatostatin, acetylcholine, norepinephrine, serotonin, adenosine, and glutamate (Wess 1998). PT actions are not discriminate, and experimental evidence indicating that one PT-sensitive G protein-coupled receptor has been inactivated would imply that other Gi/o-sensitive receptors in the same cell have been similarly affected (Wess 1998). Given the well-established role of many of the previously mentioned neurotransmitters in modifying the activity of DA neurons, it is somewhat surprising that neither the average basal firing rate nor discharge pattern of cells recorded in PT-lesioned rats differed significantly from cells in control animals. Similar results were obtained by Innis and Aghajanian (1987) and could infer that G protein-coupled receptors do not actively contribute to the basal firing properties of these neurons. However, compensatory changes in the activity of DA neurons during the interval between PT injections and the start of the recording studies could have masked alterations attributable to inactivation of these receptors. It is also conceivable that chloral hydrate alters the activity of afferents that might otherwise influence the discharge characteristics of these cells via activation of G protein-coupled receptors.
PT Blocks the Inhibitory Effects of S(-)HA-966
Despite similarities in the basal firing properties of nigral DA neurons in control and PT-lesioned rats, cells in the latter group exhibited a qualitatively different response to S(-)HA-966 than either sham-injected or uninjected rats. As a group, DA neurons in control animals were inhibited by an average of 44%, consistent with previous dose-response experiments in which the ID50 dose of the drug was estimated at 6 mg/kg (Shepard et al. 1995). In contrast, the majority of cells recorded in PT-lesioned rats showed a sustained increase in firing rate in response to the drug. These results indicate that the inhibitory effects of S(-)HA-966 are mediated through a PT-sensitive substrate, presumably involving a receptor coupled to Gi/o. Because PT was applied directly within the substantia nigra, it also seems likely that the inhibitory effects of the drug are mediated locally. This interpretation is consistent with data showing that bath application of S(-)HA-966 inhibits the activity of DA neurons in coronal brain slices, a preparation in which afferent inputs originating from neurons outside the midbrain are severed (Grobaski et al. 1997).
The excitatory effects of S(-)HA-966 observed in PT-lesioned rats suggest that the drug exerts multiple and opposing actions on the activity on DA neurons. Although the effects of S(-)HA-966 in the anesthetized rat are predominantly inhibitory, sustained increases in neuronal firing have occasionally been observed in response to doses below 6 mg/kg (Shepard et al. 1995). The inhibitory effects of the drug are also frequently preceded by a transient increase in neuronal activity (Figure 1). The biphasic effects of S(-)HA-966 are similar in some respects to the actions of GHB that also increases DA neuronal firing when administered in low doses (Diana et al. 1991). It is possible that the excitatory effects of S(-)HA-966 are mediated through a pharmacological mechanism distinct from that underlying the inhibitory effects of the drug. However, it is important to note that although PT was administered locally, S(-)HA-966 was injected intravenously and, thus, was available to alter the activity of neurons throughout the CNS. Accordingly, it is equally plausible that the excitatory effects of the drug are manifest though a disinhibitory process in which activation of the same PT-sensitive mechanism that inhibits the firing rate of nigral DA neurons evokes changes in the activity of cells that project to the midbrain, resulting in an increase in DA neuronal firing. The conspicuous absence of transient or sustained increases in DA neuronal firing rate during local application of S(-)HA-966 in vitro provides further support for the notion that the local inhibitory effects of the drug mask an excitatory effect mediated by afferent projections (Grobaski et al. 1997).
PT Attenuates the Pattern Regularizing Effects of S(-)HA-966
One of the most distinctive aspects of the electrophysiological profile of S(-) HA-966 is its ability to change the firing pattern of nigral DA neurons profoundly. When administered in dosages below 10 mg/kg, the drug induces a homogeneous pacemaker-like firing pattern, which closely resembles that observed spontaneously in brain slice preparations. Spontaneous bursting activity is completely suppressed by the drug. Although the changes in firing pattern are dose dependent, pacemaker activity has been observed in the absence of a significant change in firing rate (Shepard and Lehmann 1992; Shepard et al. 1995). In addition, although the inhibitory effects of S(-)HA-966 can be fully reversed by the GABAB receptor antagonist CGP-35348, pacemaker firing persists following recovery of neuronal firing rate (Shepard et al. 1995). These data suggest that the rate-decreasing and pattern-normalizing effects of S(-)HA-966 are mediated by independent mechanisms. The results of the present study are generally consistent with this hypothesis. Thus, S(-)HA-966 continued to regularize neuronal firing pattern in PT-lesioned rats, despite the fact that the inhibitory effects of the drug had been abolished. The percentage of spikes in bursts was also significantly reduced by the drug. However, the magnitude of the change in firing pattern produced by S(-)HA-966 in PT-lesioned rats was frequently less pronounced than that observed in control animals. For example, of 12 cells analyzed in PT-lesioned rats, only four exhibited variation coefficients comparable to those obtained in control rats after S(-)HA-966 (i.e., < 20%), and over half the bursting cells tested continued to satisfy the operational definition of bursting activity following the drug. The apparent reduction in the ability of S(-)HA-966 to regularize neuronal firing pattern in PT-lesioned rats could have occurred as a consequence of the increase in firing rate produced by the drug, because a decrease in interspike interval would have increased the probability of encountering spike pairs that satisfied the operational definition of bursting activity. Indeed, in those instances where cells were retained long enough to observe recovery from the excitatory effects of S(-)HA-966, firing pattern became increasingly pacemaker-like as the firing rate returned to predrug levels.
Are GABAB Receptors Responsible for the Electrophysiological Effects of S(-)HA-966 ?
As a member of the large family of G protein-coupled receptors, postsynaptic GABAB receptors are known to be inactivated by PT (Reisine 1990; Misgeld et al. 1995). The results of the present study are entirely consistent with previous pharmacological data implicating these receptors in the inhibitory effects of S(-)HA-966. However, our findings do not exclude the possibility that the inhibitory effects of S(-)HA-966 are mediated by other PT-sensitive receptors. Indeed, recent binding studies have indicated that S(-)HA-966 has little or no affinity for archetypal GABAB receptors (Grobaski et al. 1997; Morrow et al. 1997). Among the list of alternative candidates is the GHB receptor, which also seems to couple to a PT-sensitive G protein (Ratomponirina et al. 1995). On the other hand, recent studies showing that native GABAB receptors are heterodimers and that each of the constituent proteins is expressed in different isoforms suggest that GABAB receptor subtypes could exist (reviewed by Bettler et al. 1998; Möhler and Fritschy 1999). These observations raise the intriguing possibility that both S(-)HA-966 and GHB may represent a new generation of subtype-specific, GABAB receptor ligands.
References
Akaoka H, Charlety P, Saunier CF, Buda M, Chouvet G . (1992): Inhibition of nigral dopamine neurons by systemic and local apomorphine: Possible contribution of dendritic autoreceptors. Neuroscience 49: 879–891
Andrade R, Malenka RC, Nicoll RA . (1986): A G protein couples serotonin and GABAB receptors to the same channels in hippocampus. Science 234: 1261–1265
Baring MD, Walters JR, Eng N . (1980): Action of systemic apomorphine on dopamine cell firing after neostriatal kainic acid lesion. Brain Res 181: 214–218
Bernasconi R, Lauber J, Marescaux C, Vergnes M, Martin P, Rubio V, Leonhardt T, Reymann N, Bittiger H . (1992): Experimental absence seizures: Potential role of gammahydroxybutyric acid and GABAB receptors. J Neural Transm Suppl 35: 155–177
Bettler B, Kaupmann K, Bowery N . (1998): GABAB receptors: Drugs meet clones. Curr Opinion Neurobiol 8: 345–350
Bonta IL, De Vos CJ, Grijsen H, Hillen FC, Noach EL, Sim AW . (1971): 1-Hydroxy-3-amino-pyrrolidone-2(HA966): A new GABA-like compound, with potential use in extrapyramidal diseases. Br J Pharmacol 43: 514–535
Bunney BS, Walters JR, Roth RH, Aghajanian GK . (1973): Dopaminergic neurons: Effect of antipsychotic drugs and amphetamine on single cell activity. J Pharmacol Exp Ther 185: 560–571
Diana M, Mereu G, Mura A, Fadda F, Passino N, Gessa G . (1991): Low doses of gammahydroxybutyric acid stimulate the firing rate of dopaminergic neurons in unanesthetized rats. Brain Res 566: 208–211
Engberg G, Nissbrandt H . (1993): Gamma-hydroxybutyric acid (GHBA) induces pacemaker activity and inhibition of substantia nigra dopamine neurons by activating GABAB-receptors. Naunyn Schmiedebergs Arch Pharmacol 348: 491–497
Erhardt S, Andersson B, Nissbrandt H, Engberg G . (1998): Inhibition of firing rate and changes in the firing pattern of nigral dopamine neurons by gamma-hydroxybutyric acid (GHBA) are specifically induced by activation of GABA(B) receptors. Naunyn Schmiedebergs Arch Pharmacol 357: 611–619
Gähwiler BH, Brown DA . (1985): GABAB-receptor-activated K+ current in voltage-clamped CA3 pyramidal cells in hippocampal cultures. Proc Natl Acad Sci USA 82: 1558–1562
Gallimberti L, Ferri M, Ferrara SD, Fadda F, Gessa GL . (1992): Gamma-hydroxybutyric acid in the treatment of alcohol dependence: A double-blind study. Alcohol Clin Exp Res 16: 673–676
Gallimberti L, Cibin M, Pagnin P, Sabbion R, Pani PP, Pirastu R, Ferrara SD, Gessa GL . (1993): Gamma-hydroxybutyric acid for treatment of opiate withdrawal syndrome. Neuropsychopharmacology 9: 77–81
Gessa GL, Vargiu I, Crabai F, Boero GC, Caboni F, Camba R . (1966): Selective increase of brain dopamine induced by gamma-hydroxybutyrate. Life Sci 5: 1921–1930
Grace AA, Bunney BS . (1984): The control of firing pattern in nigral dopamine neurons: Burst firing. J Neurosci 4: 2877–2890
Grobaski KC, Ping H, da Silva HM, Bowery NG, Connelly ST, Shepard PD . (1997): Responses of rat substantia nigra dopamine-containing neurones to (-)HA-966 in vitro. Br J Pharmacol 120: 575–580
Hechler V, Ratomponirina C, Maittre M . (1997): γ-Hydroxybutyrate conversion into GABA induces displacement of GABAB binding that is blocked by valproate and ethosuximide. J Pharmacol Exp Ther 281: 753–760
Hillen FC, Noach EL . (1971): The influence of 1-hydroxy-3-amino-pyrrolidone-2 (HA-966) on dopamine metabolism in the rat corpus striatum. Eur J Pharmacol 16: 222–224
Innis RB, Aghajanian GK . (1987): Pertussis toxin blocks autoreceptor-mediated inhibition of dopaminergic neurons in rat substantia nigra. Brain Res 411: 139–143
Jentsch JD, Elsworth JD, Redmond DE Jr, Roth RH . (1997): Phencyclidine increases forebrain monoamine metabolism in rats and monkeys: Modulation by the isomers of HA-966. J Neurosci 17: 1769–1775
Kim KM, Nakajima Y, Nakajima S . (1995): G protein-coupled inward rectifier modulated by dopamine agonists in cultured substantia nigra neurons. Neuroscience 69: 1145–1158
Koenig JFR, Klippel RA . (1963): The Rat Brain: A Stereotaxic Atlas. Baltimore, Williams & Wilkins
Kreiss DS, Bergstrom DA, Gonzalez AM, Huang KX, Sibley DR, Walters JR . (1995): Dopamine receptor agonist potencies for inhibition of cell firing correlate with dopamine D3 receptor binding affinities. Eur J Pharmacol 277: 209–214
Lüscher C, Jan LY, Stoffel M, Malenka RC, Nicoll RA . (1997): G protein-coupled inwardly rectifying K+ channels (GIRKs) mediate postsynaptic but not presynaptic transmitter actions in hippocampal neurons. Neuron 19: 687–695
Madden TE, Johnson SW . (1998): Gamma-hydroxybutyrate is a GABAB receptor agonist that increases a potassium conductance in rat ventral tegmental dopamine neurons. J Pharmacol Exp Ther 287: 261–265
Maitre M . (1997): The gamma-hydroxybutyrate signaling system in brain: Organization and functional implications. Prog Neurobiol 51: 337–361
Martin LP, Cox RF, Waszczak BL . (1990): Efficacy and potency comparisons among apomorphine enantiomers: Effects on dopamine neurons in substantia nigra of rat. Neuropharmacology 29: 135–143
Misgeld U, Bijak M, Jarolimek W . (1995): A physiological role for GABAB receptors and the effects of baclofen in the mammalian central nervous system. Prog Neurobiol 46: 423–462
Möhler H, Fritschy J-M . (1999): GABAB receptors make it to the top–as dimers. Trends Pharmacol Sci 20: 87–89
Morrow BA, Lee EJK, Taylor JR, Elsworth JD, Nye HE, Roth RH . (1997): S)-(-)HA-966, a gamma-hydroxybutyrate-like agent, prevents enhanced mesocorticolimbic dopamine metabolism and behavioral correlates of restraint stress, conditioned fear, and cocaine sensitization. J Pharmacol Exp Ther 283: 712–721
Newberry NR, Nicoll RA . (1984): Direct hyperpolarizing action of baclofen on hippocampal pyramidal cells. Nature 308: 450–452
Nissbrandt H, Engberg G . (1996): The GABAB-receptor antagonist, CGP 35348, antagonizes gamma-hydroxybutyrate and baclofen-induced alterations in locomotor activity and forebrain dopamine levels in mice. J Neural Transm 103: 1255–1263
Overton PG, Clark D . (1997): Burst firing in midbrain dopaminergic neurons. Brain Res Brain Res Rev 25: 312–334
Ratomponirina C, Hode Y, Hechler V, Maitre M . (1995): Gamma-hydroxybutyrate receptor binding in rat brain is inhibited by guanyl nucleotides and pertussis toxin. Neurosci Lett 189: 51–53
Reisine T . (1990): Pertussis toxin in the analysis of receptor mechanisms. Biochem Pharmacol 39: 1499–1504
Roth RH, Walters JR, Aghajanian GK . (1973): Effects of impulse flow on the release and synthesis of dopamine in the rat striatum. In Usdin E. Synder SH (eds), Frontiers in Catecholamine Research. New York, Pergamon Press, pp 567–574
Shepard PD, Connelly ST, Lehmann H, Grobaski KC . (1995): Effects of the enantiomers of (+/−)HA-966 on dopamine neurons: An electrophysiological study of a chiral molecule. Eur J Pharmacol 285: 79–88
Shepard PD, Lehmann H . (1992): ±)-1-Hydroxy-3-aminopyrrolidone-2 (HA-966) inhibits the activity of substantia nigra dopamine neurons through a non-N-methyl-D-aspartate-mediated mechanism. J Pharmacol Exp Ther 261: 387–394
Singh L, Donald AE, Foster AC, Hutson PH, Iversen LL, Iversen SD, Kemp JA, Leeson PD, Marshall GR, Oles RJ et-al . (1990): Enantiomers of HA-966 (3-amino-1-hydroxypyrrolid-2-one) exhibit distinct central nervous system effects: (+)HA-966 is a selective glycine/N-methyl-D-aspartate receptor antagonist, but (-)-HA-966 is a potent gamma-butyrolactone-like sedative. Proc Natl Acad Sci USA 87: 347–351
Snead OC . (1992): Evidence for G protein modulation of experimental-generalized absence seizures in rat. Neurosci Lett 148: 15–18
Snead OC . (1988): Gamma-hydroxybutyrate model of generalized absence seizures: Further characterization and comparison with other absence models. Epilepsia 29: 361–368
Snead OC . (1996): Relation of the [3H]γ-hydroxybutyric acid (GHB) binding site to the γ-aminobutyric acidB (GABAB) receptor in rat brain. Biochem Pharmacol 52: 1235–1243
Thompson SM, Gähwiler BH . (1992): Comparison of the actions of baclofen at pre- and postsynaptic receptors in the rat hippocampus in vitro. J Physiol Lond 451: 329–345
Waldmeier PC . (1991): The GABAB antagonist, CGP 35348, antagonizes the effects of baclofen, gammabutyrolactone, and HA-966 on rat striatal dopamine synthesis. Naunyn Schmiedebergs Arch Pharmacol 343: 173–178
Werner G, Mountcastle VB . (1963): The variability of central neural activity in a sensory system and its implications for the central reflection of sensory events. J Neurophysiol 26: 958–977
Wess J . (1998): Molecular basis of receptor/G-protein-coupling selectivity. Pharmacol Ther 80: 231–264
Williams SR, Turner JP, Crunelli V . (1995): Gamma-hydroxybutyrate promotes oscillatory activity of rat and cat thalamocortical neurons by a tonic GABAB, receptor-mediated hyperpolarization. Neuroscience 66: 133–141
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Shepard, P., Connelly, S. Pertussis Toxin Lesions of the Rat Substantia Nigra Block the Inhibitory Effects of the γ-Hydroxybutyrate Agent, S(-)HA-966 without Affecting the Basal Firing Properties of Dopamine Neurons. Neuropsychopharmacol 21, 650–661 (1999). https://doi.org/10.1016/S0893-133X(99)00063-9
Received:
Revised:
Accepted:
Issue Date:
DOI: https://doi.org/10.1016/S0893-133X(99)00063-9