Abstract
Currently accepted treatments for schizophrenia can effectively control positive symptoms but have limited impact on cognitive deficits in schizophrenia. The purpose of these experiments was to address this unmet need by characterizing the effects of classical and second-generation antipsychotics on cognitive impairments associated with schizophrenia. An additional aim was to characterize the part(s) of the pharmacological profile of drugs that were important to reverse deficits. Cognitive deficits were assessed using a frontally mediated attentional set-shifting task in rats that is analogous to tasks used in humans and nonhuman primates that assess executive function. Mirroring findings in patients with schizophrenia, the classical antipsychotic haloperidol was ineffective in treating set-shifting deficits induced by subchronic treatment with phencyclidine (PCP). Similarly, second-generation antipsychotics, risperidone, clozapine, and olanzapine were ineffective. In contrast, selected doses of sertindole and the 5-HT6 receptor antagonist SB 271046 attenuated PCP-induced set-shifting deficits. Finally, the 5-HT2A receptor antagonist M100907 was without effect. Further examination revealed that repeated treatment (21 days) with sertindole, but not olanzapine, also was effective in reversing the executive function deficit. These data suggest that the combination of 5-HT6 antagonistic activity and the absence of antimuscarinic activity may represent key characteristics of the pharmacological profile for improved antipsychotic drugs for schizophrenia.
Similar content being viewed by others
INTRODUCTION
For many years, psychotic symptoms have been considered the hallmark for schizophrenia and have been the primary target for pharmacological treatment. However, Kraepelin's characterization of schizophrenia from over a century ago included descriptions of cognitive deficits (Kraepelin, 1904), and these have gained greater attention in the treatment literature during the past decade (Green et al, 2000; Weinberger and Gallhofer, 1997). Cognitive deficits found in patients with schizophrenia appear widespread and are related to executive function, working memory, and attention. These cognitive deficits are present at the onset of illness, persist for most of patients’ lives without remission, and may precede the development of positive symptoms (Tollefson, 1996; Brewer et al, 2006). Unlike psychotic symptoms, cognitive deficits demonstrate a robust inverse association with community functioning and illness outcome (Addington and Addington, 1999; Green, 1996; Harvey et al, 1999). Therefore, treatments that ameliorate cognitive deficits have the potential to significantly improve patients’ quality of life. However, such treatments remain elusive.
Conventional antipsychotic treatments (eg haloperidol) are reported to lack effect on cognitive deficits (Mortimer, 1997), and to impair some cognitive functions (Cleghorn et al, 1990; Cutmore and Beninger, 1990). Novel antipsychotic compounds (second-generation or ‘atypical’ antipsychotics) such as clozapine (Fitton and Heel, 1990), olanzapine (Fulton and Goa, 1997), and sertindole (Kane and Tamminga, 1997; Azorin et al, 2006) have some beneficial effect on negative symptoms and reduced potential to produce extrapyramidal side effects, but these agents have demonstrated inconsistent effects on cognitive function in patients with schizophrenia. Depending on the type of cognitive domain measured, second-generation antipsychotics have been reported to produce improvement (Mortimer 1997; Meltzer and McGurk, 1999; Keefe et al, 2007), no effect (Hoff et al, 1996; Meltzer and McGurk, 1999), and impairment (Goldberg et al, 1993). The effect of sertindole on cognitive function has not been investigated extensively; however, a small clinical trial indicates a beneficial effect on some cognitive substrates, including executive function, in individuals diagnosed with schizophrenia (Gallhofer et al, 2007). When these data are considered together, second-generation antipsychotics seem superior to typical neuroleptics with regard to cognitive function; however, the selectivity and magnitude of attenuation of cognitive deficits has been variable. Thus, there appears to be some promise for second-generation drugs in treating cognitive deficits associated with schizophrenia. Yet methodological limitations related to clinical studies (eg schizophrenia heterogeneity, different cognitive measures) hinder the assessment of treatment efficacy. Investigating these questions with preclinical evaluation allows for greater control regarding subject history, the production and manipulation of types of impairments, and the ability to use selective pharmacological compounds.
In preclinical cognition tests, differential effects of antipsychotics have been reported, with some antipsychotics impairing cognitive function in normal animals, and others apparently having no effect (eg Didriksen, 1995; Skarsfeldt, 1996; Didriksen et al, 2006). However, an unmet need in the treatment of schizophrenia is improvement of impaired cognition. Cognitive improvement by pharmacological intervention is difficult to show in healthy animals and may have little predictive validity for efficacy in schizophrenia. A more desirable starting point methodologically is one where normal cognitive function is disrupted, and the effect of treatments in ameliorating deficits can be observed.
In the current experiments, we utilized a rodent model of attentional set shifting that is sensitive to the effects of lesions (Birrell and Brown, 2000; Fox et al, 2003), natural aging (Barense et al, 2002), and pharmacological manipulations (Chen et al, 2004; Rodefer et al, 2005; Rodefer and Nguyen, 2006). In addition, we employed the well-validated subchronic phencyclidine (PCP)-administration paradigm (Jentsch and Roth, 1999; Cochran et al, 2003; Egerton et al, 2005; Abdul-Monim et al, 2006, 2007) to produce enduring cognitive deficits similar to those observed in schizophrenia (Javitt and Zukin, 1991). This permitted us to examine treatment effects of classical and second-generation antipsychotics that have different profiles and activity at multiple neurotransmitter receptors, including dopamine (DA) D2, 5-HT2A, and 5-HT6. In Experiment 1, we investigated acute treatment with a range of antipsychotics (haloperidol, risperidone, clozapine, olanzapine, sertindole). We also evaluated the selective 5-HT2A receptor antagonist M100907 and the 5-HT6 receptor antagonist SB 271046, in order to elucidate possible differential mechanistic effects of atypical antipsychotics. In Experiment 2, we studied the effects of 3-week repeated treatment with sertindole and olanzapine to mimic more closely clinical treatment regimens with antipsychotics, and to compare acute and repeated treatment regimens. A goal of these experiments was to characterize the pharmacological profile of drugs that have the greatest promise for treating cognitive deficits in schizophrenia to aid development of effective treatments for these debilitating symptoms.
MATERIALS AND METHODS
Subjects
Male Long-Evans rats (Harlan, Indianapolis, IN), weighing about 250 g (approximately 60 days old) at the beginning of the study, were housed individually in plastic cages (25 × 45 × 20 cm). Testing was conducted during the light phase of a 12 h light/dark cycle (lights on at 0700 hours). For 7–10 days before the onset of behavioral testing, rats were maintained on a restricted feeding schedule with daily feed amounts contingent on their performance on the food-motivated task. Varying post-session food allotments beginning permitted us to maintain rats at 85–90% of ad libitum body weight. Water was always available ad libitum in the home cage. All experimental protocols were approved by the Institutional Animal Care and Use Committee and were conducted in compliance with the guidelines of the NIH Guide for Care and Use of Laboratory Animals.
Apparatus
The set-shifting task adapted for rodents uses olfactory and tactile stimuli, rather than the visual stimuli used for testing of nonhuman primates and humans (Birrell and Brown, 2000). This experiment used terracotta flowerpots as digging bowls, with an internal diameter and depth of 10 cm. We applied scented oils to the rim of the pot to produce a long-lasting odor and we refreshed the odors at the beginning of each testing session.
The test chamber was a Plexiglas box measuring 50 × 37.5 × 25 cm with an opaque barrier separating one-third of the box from the rest (along the long axis of the box). On each trial, the two digging pots were placed adjacent to each other in the larger section of the box while the rat waited in the smaller section. The rat was given access to the pots by raising the barrier, which was then put back down once the trial had begun.
Procedure
Rats learned to dig for a cereal food reward (Honey Nut Cheerio, General Mills, Minneapolis, MN) that had been buried (∼2.5 cm depth) in one of two terracotta pots (10 cm internal diameter and depth) that were filled with different digging media (eg corn cob bedding or small pieces of foam) or scented with different odorants (eg vanilla or jasmine oil, or both). The presence of reward was consistently associated only with one dimension (medium or odor) of each pot (counterbalanced across rats). After training on two problems in which the reward was consistently associated with the same stimulus dimension (medium or odor), rats were then tested on new discrimination problems during one test session (Table 1). Initially, reward was associated with a new stimulus within a consistent relevant stimulus dimension (ie intradimensional shift (IDS); eg vanilla to jasmine). Subsequently, reward was shifted to a new and previously irrelevant stimulus dimension (ie extradimensional shift (EDS); eg vanilla to glass beads). In addition, rats experienced multiple reversal problems where reward was shifted to a previously nonreinforced stimulus (S−) within the same dimension while the previously reinforced (S+) stimulus became nonreinforced. Direction of EDS (ie odor to medium or medium to odor) was counterbalanced across subjects and was without effect on any of the behavioral variables (all p's >0.05), so it was not considered in the presentation of results. The high number of possible pairings and orderings of stimuli prevented complete counterbalancing, so the stimuli were assigned in pairs that were maintained across all subjects (eg when jasmine was the S+, vanilla was always the S−, and vice versa). The criterion for advancing to the next discrimination problem was six consecutive correct trials during all test sessions. Completion of all seven discrimination problems occurred in one test session that lasted approximately 1–3 h.
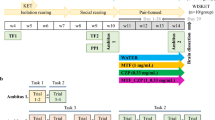
Drug Administration
PCP HCl obtained from Sigma-Aldrich (St Louis, MO, USA) and Lundbeck A/S (Copenhagen, Denmark) was prepared in sterile physiological (0.9% w/v) saline at a concentration of 5.0 mg/ml. Saline served as vehicle for PCP and was administered i.p. in a volume of 1.0 ml/kg. After habituating to the colony room environment, rats received a series of subchronic injections of PCP or saline twice daily (approximately at 0800 and 2000 hours) for 7 days. After subchronic injections were completed, rats experienced a washout period of 10 days before behavioral training and testing. Clozapine, haloperidol, and risperidone were obtained from Sigma-Aldrich and were dissolved in a minimum amount of acetic acid and then diluted in water, which served as vehicle. Solutions were adjusted to pH 4.5–6.0 with 0.1 M NaOH as needed. Sertindole, olanzapine, M100907, and SB271046 were supplied by Lundbeck A/S and a 5% aqueous solution of hydroxyl-propyl-β-cyclodextrin (cyclodextrin) was used as vehicle for each. Based on pilot data (Rodefer, 2006) we evaluated acute drug administration in Experiment 1 of clozapine (0.1–5 mg/kg, i.p.), risperidone (0.01–0.3 mg/kg, i.p.), haloperidol (0.01–0.1 mg/kg, i.p.), M100907 (0.08–0.32 mg/kg, s.c.), and SB271046 (10 mg/kg, s.c.) or their vehicles were administered in a volume of 1.0 ml/kg. Sertindole (0.63–2.5 mg/kg), olanzapine (1.5–3.0 mg/kg), and the cyclodextrin vehicle were administered p.o. with a neonatal feeding tube at a volume of 5.0 ml/kg. Drugs were administered immediately before behavioral testing, with the exception of sertindole (2 h, due to a delayed peak effect), to evaluate the effects of drug on all discrimination problems in the set-shifting procedure. We selected dose ranges for compounds that did not produce behavioral disruption and that have been shown to induce DA D2 receptor occupancies corresponding to therapeutically effective levels (Olsen et al, 2006) or to be effective in relevant mechanistic in vivo models (Zhang and Bymaster, 1999; Sanchez and Arnt, 2000; Hatcher et al, 2005; Wunsch et al, 2006). The compounds examined differ on activity at DA D2, 5-HT2A, and 5-HT6 receptors. Based on these previous reports, all drugs examined had adequate duration of action for CNS activity during the test session. During repeated (21 days) drug administration in Experiment 2, rats completed PCP dosing before beginning daily dosing for 3 weeks with olanzapine (3.0 mg/kg, b.i.d), sertindole (1.3 mg/kg a.m. only+p.m. vehicle injection; 24 h exposure was ensured due to the long serum half-life of sertindole), or vehicle (b.i.d.). Rats received the final treatment dose about 60 min prior to testing in the set-shifting procedure. Experimenters were blind to group assignment in all experiments.
Plasma Analysis
Blood samples were drawn 3–4 h after administration of sertindole, after completion of the attentional set-shifting test. Rats were anesthetized with an overdose of pentobarbital and cardiac blood was obtained and then centrifuged for 10 min at 4°C. Plasma was drawn off and samples were immediately frozen at −80°C, before shipping in dry ice for analysis.
The plasma concentration of sertindole was determined by liquid chromatography/tandem mass spectrometry (LC–MS/MS). On-line sample preparation and liquid chromatography were performed with turbulent flow chromatography (Cohesive Technologies, UK), using a dual column configuration, according to the methodology described previously (Sanchez and Kreilgaard 2004). Escitalopram was used as the internal standard. MS/MS detection was performed with an Applied Biosystems Sciex API 3000 instrument in positive-ion electrospray ionization mode. Olanzapine was analyzed using the same methodology used for sertindole but with an acidic mobile phase system (water/acetonitrile with 0.1% formic acid) instead of an alkaline system (water/methanol with 0.1% ammonium hydroxide), a different analytical column (Phenomenex Synergi Max-RP, 2 × 30 mm instead of Waters XTerra MS C8, 2.1 × 20 mm) and an Applied Biosystems Sciex API 4000 instrument. Sertindole and olanzapine were detected at a parent>daughter molecular mass of 441.30>113.10 and 313.18>256.10 AMU using a depolarization potential of 46/41, a collision energy of 57/33 and a collision cell exit potential of 22/6, respectively. Nitrogen was used for the auxiliary and nebulizer gases, and argon was used for the collision gas. Retention times were 0.7 min for sertindole and 4.1 min for olanzapine. The peak area correlated linearly with the plasma concentration of the analytes in the range of 1–500 ng/ml. If the plasma sample drug concentration was above 500 ng/ml, the sample was diluted appropriately in blank plasma before analysis. The lower limit of quantification was 1.0 ng/ml for all compounds (peak S/N>6).
Data Analysis
Because cognitive deficits are experimentally induced, we first conducted a validity check of these methods by examining set-shifting performance (trials to criterion for EDS task performance) of animals treated with subchronic PCP or saline with an analysis of variance (ANOVA) with two main effects (discrimination problem, subchronic treatment) and the problem × subchronic treatment interaction. Subsequently, we assessed the impact of acute (Experiment 1) or sustained (Experiment 2) drug treatment on set-shifting performance across all discrimination problems using repeated measures ANOVA. In all analyses, Bonferroni corrected post hoc comparisons were used following significant F-values to test mean differences between dosing groups.
RESULTS
Validity Check on Formation of Attentional Set
A repeated measures ANOVA was used to examine the effect of problem (IDS vs EDS) on trials to criterion in all control subjects (subchronic saline administration+either acute vehicle or repeated 21-day vehicle treatment, with duration of treatment included as a between-subjects factor). Analyses indicated a significant difference between the IDS and EDS problems (F(1, 78)=25.99, p<0.001, data not plotted), with no significant effect of duration of saline administration (F(1, 78)=2.10, p=0.15) or interaction between duration and problem (F(1, 78)=0.39, p=0.53). Control rats across all experiments required significantly more trials to criterion within the EDS problem (mean (SE) trials=10.04 (0.28)) compared to the IDS problem (mean (SE) trials=8.53 (0.22)). Thus, these analyses suggest that the EDS problem was reliably more difficult than the IDS problem in all control animals and that animals formed a cognitive set in this procedure.
Validity Check of Experimentally Induced Cognitive Deficits
We first examined effects of PCP pretreatment between rats that had received either subchronic PCP or saline administration followed by washout during the pretreatment phase and received acute vehicle injections prior to testing. There was a significant main effect of discrimination problem (F(1, 132)=13.64, p<0.001), a main effect of PCP pretreatment (F(1, 132)=16.46, p<0.001) and a significant discrimination problem by PCP pretreatment interaction (F(6, 132)=12.83, p<0.001). Bonferroni post hoc analyses revealed that subchronic PCP-treated animals differed significantly from saline-treated animals on the trials to criterion for the EDS task (t(20)=9.23, p<0.001) (Figure 1, top frame) and this was evident in all other cohort comparisons. No significant PCP-induced impairment on trials to criterion was observed on any other discrimination problem (all ps>0.05), Thus, subchronic PCP administration reliably and selectively impaired set-shifting performance in the EDS discrimination problem.
Performance of subjects in the attentional set-shifting procedure that were treated with subchronic (7 days) phencyclidine (PCP) or saline and acute administration of either risperidone (0.01–0.3 mg/kg; top (a)), clozapine (0.1–5.0 mg/kg, bottom (b)), or vehicle. Rats treated with subchronic PCP+veh were significantly impaired on extradimensional shift (EDS) trials to criterion compared to rats treated with subchronic saline+veh. Neither risperidone nor clozapine reversed the PCP-induced EDS impairment at any dose examined. Two doses of clozapine (0.3 & 5.0 mg/kg) significantly increased the trials required to complete Rev1. (*p<0.05) (PCP+veh and saline+veh n=10–12 per group; risperidone treatment groups n=8–10 per group; clozapine treatment groups n=8–10 per group). Error bars represent one standard error of the mean (SE).
Experiment 1: Effects of Acute Antipsychotic Administration
We tested the ability of acutely administered antipsychotics to reverse the cognitive deficit in EDS function observed in animals treated with subchronic PCP administration (PCP+veh group). Examination of the behavioral effects of risperidone (0.01–0.3 mg/kg, i.p.) (Figure 1 top) revealed a significant main effect of discrimination problem (F(6, 240)=128.47, p<0.01) but no significant main effect of risperidone drug dose (F(4, 240)=0.40, p=0.81) or risperidone dose × problem interaction (F(24, 240)=1.01, p=0.48). Thus, the treatment with risperidone did not attenuate the PCP-induced EDS deficit across any dose examined.
Examination of the behavioral effects of clozapine (0.1–5.0 mg/kg, i.p.) (Figure 1 bottom) revealed a significant main effect of discrimination problem (F(6, 288)=89.90, p<0.001) but no significant main effect of clozapine drug dose (F(5, 288)=1.27, p=0.30). However, there was a significant clozapine dose × problem interaction (F(30, 288)=1.63, p=0.02). Bonferroni post hoc analyses revealed significant differences during the Rev1 discrimination problem between the PCP+veh treatment group and the PCP+0.3 mg/kg (t(19)=3.20, p<0.05) and PCP+5.0 mg/kg (t(18)=4.01, p<0.001) clozapine treatment groups, representing poorer performance in the clozapine-treated rats at these doses compared to the PCP-treated rats that received vehicle. There were no other significant differences between PCP+veh and any clozapine-treated groups. Thus, clozapine did not attenuate the PCP-induced EDS deficit across any dose examined.
Analysis of acute haloperidol administration (0.01–0.1 mg/kg, i.p.) (Figure 2 top) revealed a significant main effect of discrimination problem (F(6, 198)=134.47, p<0.001), a significant main effect of haloperidol dose (F(3, 198)=17.50, p<0.001), but no significant haloperidol dose × problem interaction (F(18, 198)=0.88, p=0.60). Bonferroni post hoc analyses revealed that compared to the PCP+veh group, the 0.1 mg/kg dose of haloperidol resulted in significantly increased trials to criterion during the Rev1 (t(18)=5.56, p<0.001), Rev2 (t(18)=2.87, p<0.05), EDS (t(18)=2.89, p<0.05), and Rev3 (t(18)=3.17, p<0.05) discrimination problems. There were no other significant differences between PCP+veh and any haloperidol-treated groups. Thus, treatment with haloperidol did not attenuate the PCP-induced deficit in EDS performance and the highest dose of haloperidol increased cognitive impairments in four discrimination problems.
Performance of subjects in the attentional set-shifting procedure that were treated with subchronic (7 days) phencyclidine (PCP) or saline and acute administration of either haloperidol (0.01–0.1 mg/kg; top (a)), olanzapine (1.5–3.0 mg/kg, bottom (b)), or vehicle. Rats treated with subchronic PCP+veh were significantly impaired on extradimensional shift (EDS) trials to criterion compared to rats treated with subchronic saline+veh. Neither haloperidol nor olanzapine reversed the PCP-induced EDS impairment at any dose examined. The highest dose of haloperidol (0.1 mg/kg) significantly increased the trials required to complete the EDS and all reversal problems. (*p<0.05) (PCP+veh and saline+veh n=12 per group; haloperidol treatment groups n=8–10 per group; olanzapine treatment groups n=12 per group). Error bars represent one standard error of the mean (SE).
Examination of the effects of olanzapine (1.5–3.0 mg/kg, p.o.) (Figure 2 bottom) revealed a significant effect of discrimination problem (F(6, 198)=30.60, p<0.001) but no significant effect of olanzapine dose (F(2, 198)=1.62, p=0.21) or olanzapine dose × problem interaction (F(12, 240)=0.39, p=0.96). Thus, treatment with olanzapine did not attenuate the PCP-induced EDS deficit across the doses examined, and olanzapine was without effect across the doses examined.
Acute sertindole administration (0.63–2.5 mg/kg, p.o.) produced a significant effect of discrimination problem (F(6, 300)=21.86, p<0.001), a significant effect of sertindole dose (F(3, 300)=5.09, p=0.003) and sertindole dose × problem interaction (F(18, 300)=2.50, p<0.001) (Figure 3, top). Bonferroni post hoc analyses were performed to determine where performance on discrimination problems differed across groups. When compared to the subchronic PCP+veh group, the 1.2 mg/kg (t(22)=4.59, p<0.001) and 2.5 mg/kg (t(22)=3.68, p<0.01) doses of sertindole significantly attenuated the deficit in EDS performance. In addition, the lowest dose of sertindole (0.63 mg/kg) produced a significant increase in trials to criterion in the Rev1 problem (t(22)=3.06, p<0.01), but this effect was not observed in any other dose of sertindole, nor in any of the other reversal problems. As such, acute administration of the two higher doses (1.3 and 2.5 mg/kg) of sertindole attenuated the PCP-induced deficit in EDS learning. In order to clarify if the effect of sertindole was specific to subchronic PCP-treated rats we examined the effect of acute sertindole (2.5 mg/kg, p.o) in animals receiving subchronic saline treatment. Comparing the saline-sertindole group to the saline-vehicle group revealed no significant differences across any of the discrimination problems (all p's >0.05; Figure 3, top). Thus, the effects of sertindole were specific to our animal model of cognitive deficits.
Performance of subjects in the attentional set-shifting procedure that were treated with subchronic (7 days) phencyclidine (PCP) or saline and acute administration of either sertindole (0.63–2.5 mg/kg; top (a)), M100907 (0.08–0.32 mg/kg, bottom (b)), SB 271046 (10 mg/kg, bottom (b)), or vehicle. Rats treated with subchronic PCP+veh were significantly impaired on extradimensional shift (EDS) trials to criterion compared to rats treated with subchronic saline+veh. The two higher doses of sertindole (1.3 & 2.5 mg/kg) reversed the PCP-induced EDS impairment. The lowest dose (0.63 mg/kg) was without effect on EDS performance but impaired Rev1 performance. M100907 across all doses examined was without effect on EDS trials whereas SB 271046 reversed the PCP-induced EDS deficit (*p<0.05) (n=12 per group for all groups). Error bars represent one standard error of the mean (SE).
Lastly, we examined acute administration of the 5-HT2A antagonist M100907 (0.08–0.32 mg/kg, s.c.) and the 5-HT6 antagonist SB 271046 (10 mg/kg, s.c.) in PCP-treated animals (Figure 3, bottom). Analysis of the administration of M100907 produced a significant effect of discrimination problem (F(6, 282)=16.95, p<0.001), a significant effect of M100907 dose (F(3, 282)=5.23, p<0.01) but not a significant M100907 dose × problem interaction (F(18, 282)=1.31, p=0.19) (Figure 3, bottom). Bonferroni post hoc analyses indicated that M100907 did not significantly effect trials to criterion in any discrimination problem when compared to the PCP+veh control group. In comparison, acute administration of the 5-HT6 antagonist SB 271046 produced a significant main effect of discrimination problem (F(6, 144)=22.64, p<0.001), a significant main effect of SB 271046 dose (F(1, 144)=10.32, p=0.003), and a significant SB 271046 dose × problem interaction (F(6, 144)=3.99, p<0.001) (Figure 3, bottom). Bonferroni post hoc analyses indicated that SB 271046 significantly attenuated the PCP-induced EDS deficit compared to the PCP+veh group (t(22)=5.49, p<0.001). Thus, SB 271046, but not M100907, was effective in reversing the PCP-induced cognitive deficit.
Experiment 2: Effects of Repeated Antipsychotic Administration
We investigated repeated (21 days) administration of olanzapine (3.0 mg/kg, p.o.) and sertindole (1.3 mg/kg, p.o.) in an attempt to evaluate one inactive and one active drugs, respectively, from Experiment 1 (Figure 4). Analysis of the repeated administration of olanzapine produced a significant effect of discrimination problem (F(1, 132)=9.01, p<0.001), no significant effect of olanzapine treatment (F(1, 132)=1.54, p=0.23), and no significant olanzapine treatment × problem interaction (F(6, 132)=0.44, p=0.85). Thus, repeated olanzapine administration did not produce significant behavioral attenuation of the PCP-induced EDS deficit similar to results of acute administration.
Performance of subjects in the attentional set-shifting procedure that were treated with subchronic (7 days) phencyclidine (PCP) or saline and either repeated (21 days) sertindole (1.3 mg/kg), olanzapine (3.0 mg/kg), or vehicle. Rats treated with subchronic PCP+veh were significantly impaired on extradimensional shift (EDS) trials to criterion compared to rats treated with subchronic saline+veh. Repeated treatment with sertindole (1.3 mg/kg) reversed the PCP-induced deficit while repeated treatment with olanzapine (3.0 mg/kg) was without effect (*p<0.05) (n=12 per group for all groups). Error bars represent one standard error of the mean (SE).
Repeated administration of sertindole produced a significant main effect of discrimination problem (F(6, 132)=6.62, p<0.0001), no significant main effect of sertindole treatment (F(1, 132)=1.82, p=0.19), and a significant sertindole treatment × problem interaction (F(6, 132)=2.31, p<0.01). Bonferroni post hoc analyses suggested that repeated sertindole administration significantly attenuated the PCP-induced EDS deficit (t(22)=4.66, p<0.001) compared to the PCP+veh group. Thus, these data suggest that similar to acute administration, repeated administration of sertindole was effective in reversing the PCP-induced cognitive deficit.
Plasma Exposure
We examined circulating levels of drug in two of the acute sertindole dose groups and in the repeated sertindole treatment group. Plasma concentrations (mean±SE) of sertindole shortly after completion of the attentional set-shifting test session were 42 (±7.8; n=12) and 93 (±12; n=11) ng/ml after acute treatment with doses of 0.63 and 1.3 mg/kg, p.o., respectively. Plasma concentration was 107 (±9.2; n=10) ng/ml after daily oral treatment with 1.3 mg/kg sertindole for 3 weeks, a value slightly higher than that seen after acute treatment.
DISCUSSION
In the current set of studies, we examined the effects of classical and second-generation antipsychotics on cognitive deficits in a rodent model of executive function. The classical antipsychotic haloperidol (with preferential DA D2 antagonist properties) failed to reverse cognitive deficits in the EDS discrimination task and actually worsened performance at the highest dose tested. The second-generation antipsychotics clozapine, risperidone, and olanzapine were similarly without effect on PCP-induced deficits in EDS performance, whereas sertindole induced a dose-dependent reversal of set-shifting impairment. Results of repeated administration of sertindole and olanzapine in Experiment 2 fully replicated the differentiation between these drugs in acute administration observed in Experiment 1.
When comparing effects of different drugs, it is essential to examine a valid range of doses to avoid false negative results that could bias interpretations of the relative efficacy of different pharmacological agents. The validity of the dose selection can be evaluated by comparison to doses effective in other rodent models of psychosis, by confirming clinically relevant plasma levels and/or DA D2 receptor occupancies in vivo in the central nervous system. We selected dose ranges of haloperidol, olanzapine, and risperidone that did not produce behavioral disruption and that have been shown to induce DA D2 receptor occupancies that correspond to therapeutically effective levels reported previously (Zhang and Bymaster, 1999; Natesan et al, 2006; LTB Brennum, H Lundbeck, unpublished), and induce marked behavioral effects in various animal models of psychosis (for review, see Arnt and Skarsfeldt, 1998). Clozapine has weaker DA D2 in vivo binding potency, but the selected doses examined were within behaviorally active levels, and further dose increase leads to marked sedation (see Arnt and Skarsfeldt, 1998). Sertindole did show reversal of the EDS deficit in the dose range that also inhibited amphetamine-induced hyperactivity in rats (Arnt and Skarsfeldt, 1998). In addition, plasma levels of sertindole after the minimal effective dose (1.3 mg/kg) were within the range of exposures obtained in clinical studies of sertindole (35–100 ng/ml; Tamminga et al, 1997).
In addition to testing an appropriate range of doses, it is important to evaluate whether drugs reverse impairments relevant to the study of psychopathology or whether they lead to a general enhancement of cognitive function. Thus, we examined whether the effect of sertindole was specific for PCP-treated rats or whether it induced a general improvement in attentional set shifting. However, no effect of acute treatment with sertindole (2.5 mg/kg, p.o.) was observed in rats subchronically treated with saline instead of PCP. This supports the relevance of current findings in the search for pharmacological agents to treat deficits associated with schizophrenia.
A goal of the current study was to describe the pharmacological profile of agents with greatest efficacy for reversing cognitive deficits. The lack of effect of haloperidol suggests that DA D2 receptor antagonism does not play an important role in ameliorating cognitive deficits. In an attempt to understand the differentiation between clozapine, olanzapine, and risperidone vs sertindole, we performed an experiment exploring the profiles of a selective 5-HT2A (M100907; Zhang and Bymaster, 1999) and 5-HT6 antagonist (SB 271046; Lacroix et al, 2004; Woolley et al (2004)) at dose levels shown to be effective in relevant mechanistic in vivo models. Activity at 5-HT6 receptors has been postulated to be important in cognitive dysfunction (Mitchell and Neumaier, 2005) and psychopathology (East et al, 2002), and in the present study, the 5-HT6 antagonist reversed the PCP-induced impairment as did sertindole, while the 5-HT2A receptor antagonist treatment did not improve EDS performance significantly, very similar to effects observed with clozapine, olanzapine, and risperidone. Although a previous study reported that 5-HT6 receptor antagonist treatment improved performance in control rats (Hatcher et al, 2005), a more recent study found that selective 5-HT6 receptor antagonism reversed PCP deficits without influencing performance in control rats (Wunsch et al, 2006). These latter findings are consistent with those of the current study.
These data suggest that the high affinity of sertindole for 5-HT6 receptors may explain the superior effect observed in this cognitive task (Leysen, 2000). A potential complicating factor to this hypothesis is that, while risperidone is devoid of 5-HT6 receptor antagonism, both clozapine and olanzapine have high 5-HT6 receptor affinities (Leysen, 2000) but did not demonstrate significant effects on EDS performance. Of note, clozapine and olanzapine also have marked antimuscarinic activities, which may interfere with EDS performance. The selective muscarinic cholinergic antagonist scopolamine potently impairs EDS learning in normal control rats using the same experimental procedure (Chen et al, 2004) potentially reflecting nonfrontal cholinergic activity (Eichenbaum et al, 2003). As such, the potential benefits of clozapine and olanzapine treatment on EDS learning via their effects on 5-HT6 receptors may be counteracted by their antimuscarinic effects. Furthermore, 5-HT6 receptor antagonists have been reported to increase the extracellular levels of acetylcholine in hippocampus and cortex and counteract cognitive impairment induced by muscarinic receptor blockade. Thus, inhibition of cholinergic function may interfere with the expression of effects mediated by 5-HT6 receptor antagonism (see Mitchell and Neumaier, 2005; Hirst et al, 2006).
Only a few studies have compared the effects of several antipsychotics on cognitive deficits induced by subchronic PCP in a single model. To our knowledge, the only other broadly characterized model is the short-term operant reversal-learning paradigm (Abdul-Monim et al, 2006). Clozapine, olanzapine, and ziprasidone were all effective within a narrow dose range, while haloperidol and chlorpromazine were not. These data differ from the results obtained in the present study, and suggest that different cognitive tasks can be mediated by different receptor mechanisms. Indeed, different regions of prefrontal cortex mediate extradimensional attentional shifts and reversal learning (Birrell and Brown, 2000, McAlonan and Brown, 2003, Dias et al, 1996). It is possible that combined 5-HT2A and DA D2 antagonism of clozapine, olanzapine, and risperidone (Zhang and Bymaster, 1999; Sanchez and Arnt, 2000) can ameliorate deficits in the reversal learning paradigm, while improvement in EDS performance may require additional neurochemical effects, such as 5-HT6 antagonism and resulting increases in glutamatergic and cholinergic function.
Future research is needed to clarify the downstream pathways responsible for observed differences in drugs’ effects on distinct cognitive tasks. Combined 5-HT2A/DA D2 antagonism can increase extracellular levels of DA and acetylcholine in frontal cortex (Liegeois et al, 2002); whereas, 5-HT6 receptor antagonists also increase levels of glutamate (Dawson et al, 2001; Lacroix et al, 2004; Mitchell and Neumaier, 2005; Li et al, 2007) as well as DA and norepinephrine (Lacroix et al, 2004) in the frontal cortex without impacting 5-HT transmission. Sertindole and SB271046, but not risperidone, were recently found to significantly increase extracellular glutamate and acetylcholine in the frontal cortex (Mork et al, 2007). Thus, differential effects of 5-HT2A/DA D2 antagonism vs 5-HT6 receptor antagonism may be related to a complex interplay among neurotransmitter systems.
Results from our controlled preclinical experiment using an animal model of cognitive deficits are similar to results in clinical trials with patients with schizophrenia, supporting the ecological validity of our findings. Specifically, clozapine has demonstrated limited or no effects on executive function (Meltzer and McGurk, 1999; Hoff et al, 1996; Bellack et al, 2004). Risperidone has been shown either to be not effective (Bellack et al, 2004; Remillard et al, 2005; Lee et al, 2007) or slightly effective, as measured by Wisconsin Card Sorting Test (Meltzer and McGurk, 1999; Harvey et al, 2005), and olanzapine produces effects in the same range as risperidone (Meltzer and McGurk, 1999; Bilder et al, 2002; Keefe et al, 2007). In a small clinical trial, sertindole has shown superiority to haloperidol on executive function performance (Gallhofer et al, 2007). Findings of the current investigation extend these results from clinical trials (Gallhofer et al, 2007) by using a task that is sensitive for the evaluation of executive function in rodents and permits comparisons of several selective pharmacological treatments that are not feasible in clinical trials.
This study had several strengths. First, we utilized a behavioral task that is sensitive for the evaluation of executive function in rodents (Birrell and Brown, 2000; Fox et al, 2003). We produced a PCP-induced deficit in executive function that mirrors neuropsychological impairments observed in schizophrenia patients and permits investigation of selective pharmacological treatments without contamination of behavioral data from acute PCP administration. Our checks on both the differential acquisition of EDS vs IDS in control subjects as well as the production of a robust and selective EDS deficit observed in PCP-treated animals clearly supported the validity of our model. Second, we evaluated administration of numerous antipsychotic treatments over broad ranges of doses on the same cognitive task within a single study. Third, we examined selective 5-HT2A and 5-HT6 receptor antagonists to examine mechanistic explanations for the cognitive effects of atypical antipsychotic treatments. Fourth, we explored a repeated dosing regimen for selected compounds. This allowed us to replicate findings from acute drug administrations and more closely mimic effects in clinical treatment protocols. However, it should be noted that we did not explore repeated dosing of all compounds. Thus, we cannot be certain that repeated dosing of other agents, such as clozapine or M100907, would have no effect. Last, results of the current investigation support and extend findings from a recent clinical trial (Gallhofer et al, 2007). Recently, it has been noted that meaningful cognitive enhancement for individuals with schizophrenia will not likely come from traditional medications (Green, 2007) and even instances where positive effects are reported may be due to practice effects (Goldberg et al, 2007).
A possible limitation of this study concerns the validity of rodent model of executive function in schizophrenia. Certainly, no one animal protocol can effectively model a disease as complex and heterogeneous as schizophrenia, and previous reports (Pantelis et al, 1999) suggest that individuals with schizophrenia can demonstrate impairment on multiple aspects of cognition, including some non-EDS problems, an effect not addressed by our rodent model. However, the face validity of our model is augmented by previous reports of schizophrenia-like pathology, such as decreased parvalbumin expression (Abdul-Monim et al, 2007) and cortical metabolic hypofunction (Cochran et al, 2003) following PCP administration. Future research should determine whether differential pharmacological effects are replicated in another recently developed neurodevelopmental rodent model of schizophrenia, neonatal treatment with the neurotoxin MAM (methylazoxymethanol), which has been demonstrated to produce impairments in attentional set shifting (Featherstone et al, 2007). Another limitation is that we did not include selective antimuscarinic compounds in the current set of studies. Thus, hypotheses concerning the competing effects of 5-HT6 receptor antagonism and antimuscarinic activity of clozapine and olanzapine on EDS learning require testing in future studies.
In conclusion, the present study provides the first evidence for differential effects of second-generation antipsychotics on experimentally induced cognitive deficits in rodents. Furthermore, the results indicate that 5-HT6 receptor antagonism is important for the reversal of cognitive deficits, while 5-HT2A antagonism is suggested to provide a marginal benefit that did not significantly attenuate the PCP-induced cognitive deficit. 5-HT6 antagonistic activity combined with the absence of antimuscarinic activity, like that of sertindole, may represent key elements in the pharmacological profile for improved antipsychotic drug treatments. Clinical trials are needed to confirm the superiority of selective 5-HT6 antagonists and antipsychotics like sertindole on this cognitive domain.
References
Abdul-Monim Z, Neill JC, Reynolds GP (2007). Sub-chronic psychotomimetic phencyclidine induces deficits in reversal learning and alterations in parvalbumin-immunoreactive expression in the rat. J Psychopharmacol 21: 198–205.
Abdul-Monim Z, Reynolds GP, Neill JC (2006). The effect of atypical and classical antipsychotics on sub-chronic PCP-induced cognitive deficits in a reversal-learning paradigm. Behav Brain Res 169: 263–273.
Addington J, Addington D (1999). Neurocognitive and social functioning in schizophrenia. Schizophr Bull 25: 173–182.
Arnt J, Skarsfeldt T (1998). Do novel antipsychotics have similar pharmacological characteristics? A review of the evidence. Neuropsychopharmacology 18: 63–101.
Azorin JM, Strub N, Loft H (2006). A double-blind, controlled study of sertindole versus risperidone in the treatment of moderate-to-severe schizophrenia. Int Clin Psychopharmacol 21: 49–56.
Barense MD, Fox MT, Baxter MG (2002). Aged rats are impaired on an attentional set-shifting task sensitive to medial frontal cortex damage in young rats. Learn Mem 9: 191–201.
Bellack AS, Scholler NR, Marder SR, Kane JM, Brown CH, Yang Y (2004). Do clozapine and risperidone affect social competence and problem solving. Am J Psychiatry 161: 364–367.
Bilder RM, Goldman RS, Volavka J, Czobor P, Hoptman M, Sheitman B et al (2002). Neurocognitive effects of clozapine, olanzapine, risperidone, and haloperisdol in patients with chronic schizophrenia or schizoaffective disorder. Am J Psychiatry 159: 1018–1028.
Birrell JM, Brown VJ (2000). Medial frontal cortex mediates perceptual attentional set shifting in the rat. J Neurosci 20: 4320–4324.
Brewer W, Wood S, Phillips L, Francey S, Pantelis C, Yung A et al (2006). Generalized and specific cognitive performance in clinical high-risk cohorts: a review highlighting potential vulnerability markers for psychosis. Schizophr Bull 32: 538–555.
Chen KC, Baxter MG, Rodefer JS (2004). Central blockade of muscarinic cholinergic receptors disrupts affective and attentional set-shifting. Eur J Neurosci 20: 1081–1088.
Cleghorn JM, Kaplan RD, Szechtman B, Szechtman H, Brown GM (1990). Neuroleptic drug effects on cognitive function in schizophrenia. Schizophr Res 3: 211–219.
Cochran SM, Kennedy M, McKerchar CE, Steward LJ, Pratt JA, Morris BJ (2003). Induction of metabolic hypofunction and neurochemical deficits after chronic intermittent exposure to phencyclidine: differential modulation by antipsychotic drugs. Neuropsychopharmacology 28: 265–275.
Cutmore TRH, Beninger RJ (1990). Do neuroleptics impair learning in schizophrenic patients. Schizophr Res 3: 173–186.
Dawson LA, Nguyen HQ, Li P (2001). The 5-HT(6) receptor antagonist SB-271046 selectively enhances excitatory neurotransmission in the rat frontal cortex and hippocampus. Neuropsychopharmacology 25: 662–668.
Dias R, Robbins TW, Roberts AC (1996). Dissociation in prefrontal cortex of affective and attentional shifts. Nature 380: 69–72.
Didriksen M (1995). Effects of antipsychotics on cognitive behaviour in rats using the delayed non-match to position paradigm. Eur J Pharmacol 281: 241–250.
Didriksen M, Kreilgaard M, Arnt J (2006). Sertindole, in contrast to clozapine and olanzapine, does not disrupt water maze performance after acute or chronic treatment. Eur J Pharmacol 542: 108–115.
East SZ, Burnet PW, Leslie RA, Roberts JC, Harrison PJ (2002). 5-HT6 receptor binding sites in schizophrenia and following antipsychotic drug administration: autoradiographic studies with [125I]SB-258585. Synapse 45: 191–199.
Egerton A, Reid L, McKerchar CE, Morris BJ, Pratt JA (2005). Impairment in perceptual attentional set-shifting following PCP administration: a rodent model of set-shifting deficits in schizophrenia. Psychopharmacology 179: 77–84.
Eichenbaum HB, Ross R, Raji A, McGaughy JA (2003). Noradrenergic, but not cholinergic deafferentation of infralimbic/prelimbic cortex impairs attentional set-shifting. Program No. 940.7. 2003 Abstract Viewer/Itinerary Planner Society for Neuroscience: Washington, DC. 2003. Online.
Featherstone RE, Rizos Z, Nobrega JN, Kapur S, Fletcher PJ (2007). Gestational methylazoxymethanol actate treatment impairs select cognitive functions: parallels to schizophrenia. Neuropsychopharmacology 32: 483–492.
Fitton A, Heel RC (1990). Clozapine. A review of its pharmacological properties, and therapeutic use in schizophrenia. Drugs 40: 722–747.
Fox MT, Barense MD, Baxter MG (2003). Perceptual attentional set-shifting is impaired in rats with neurotoxic lesions of posterior parietal cortex. J Neurosci 23: 676–681.
Fulton B, Goa KL (1997). Olanzapine, a review of its pharmacological properties and therapeutic efficacy in the management of schizophrenia and related psychoses. Drugs 53: 281–298.
Gallhofer B, Jaanson P, Mittoux A, Tanghøj P, Lis S, Krieger S (2007). Course of recovery of cognitive impairment in patients with schizophrenia: a randomised double-blind study comparing sertindole and haloperidol. Pharmacopsychiatry 40: 275–286.
Goldberg TE, Goldman RS, Burdick KE, Malhotra AK, Lencz T, Patel RC, et al (2007). Cognitive improvement after treatment with second-generation antipsychotic medications in a first-episode schizophrenia: is it a practice effect? Arch Gen Psychiatry 64: 1115–1122.
Goldberg TE, Greenberg RD, Griffin SJ, Gold JM, Kleinman JE, Pickar D et al (1993). The effect of clozapine on cognition and psychiatric symptoms in patients with schizophrenia. Br J Psychiatry 162: 43–48.
Green ME (2007). Cognition, drug treatment, and functional outcome in schizophrenia: a tale of two transitions. Am J Psychiatry 164: 992–994.
Green MF (1996). What are the functional consequences of neurocognitive deficits in schizophrenia? Am J Psychiatry 153: 321–330.
Green MF, Kern RS, Braff DL, Mintz J (2000). Neurocognitive deficits and functional outcome in schizophrenia: are we measuring the ‘right stuff’? Schizophr Bull 26: 119–136.
Harvey PD, Parrella M, White L, Mohs RC, Davidson M, Davis KL (1999). Convergence of cognitive and adaptive decline in late-life schizophrenia. Schizophr Res 35: 77–84.
Harvey PD, Rabinowitz J, Eerdekens M, Davison M (2005). Treatment of cognitive impairment in early psychosis: a comparison of risperidone and haloperidol in a large long-term trial. Am J Psychiatry 162: 1888–1895.
Hatcher P, Brown V, Tait D, Bate S, Overend P, Hagan J et al (2005). 5-HT6 receptor antagonists improve performance in an attentional set shifting task in rats. Psychopharmacology 181: 253–259.
Hirst W, Stean T, Rogers D, Sunter D, Pugh P, Moss S et al (2006). SB-399885 is a potent, selective 5-HT6 receptor antagonist with cognitive enhancing properties in aged rat water maze and novel object recognition models. Eur J Pharmacol 553: 109–119.
Hoff AL, Faustman WO, Wieneke M, Espinoza S, Costa M, Wilkowitz O et al (1996). The effect of clozapine on symptom reduction, neurocognitive function, and clinical management in treatment-refractory state hospital schizophrenic inpatients. Neuropsychopharmacology 15: 361–369.
Javitt DC, Zukin SR (1991). Recent advances in the phencyclidine model of schizophrenia. Am J Psychiatry 148: 1301–1308.
Jentsch JD, Roth RH (1999). The neuropsychopharmacology of phencyclidine: from NMDA receptor hypofunction to the dopamine hypothesis of schizophrenia. Neuropsychopharmacology 20: 210–225.
Kane JM, Tamminga CA (1997). Sertindole (serdolect): preclinical and clinical findings of a new atypical antipsychotic. Exp Opin Investig Drugs 6: 1729–1741.
Keefe RSE, Bilder RM, Davis SM, Harvey PD, Palmer BW, Gold JM et al (2007). Neurocognitive effects of antipsychotic medications in patients with chronic schizophrenia in the CATIE trial. Arch Gen Psychiatry 64: 633–647.
Kraepelin E (1904). Lectures on Clinical Psychiatry. William Wood & Co: New York, NY. Lecture III: dementia praecox (pp. 21–29).
Lacroix L, Dawson L, Hagan J, Heidbreder C (2004). 5-HT6 receptor antagonist SB-271046 enhances extracellular levels of monoamines in the rat medial prefrontal cortex. Synapse 51: 158–164.
Lee S-M, Chou Y-H, Li M-H, Wan F-J, Yen M-H (2007). Effects of antipsychotics on cognitive performance in drug-naive schizophrenic patients. Prog Neuropsychopharmacol Biol Psychiatry doi 10.1016/j.pnpbp.03.016.
Leysen JE (2000). Receptor profile of antipsychotics. In: Ellenbroek BA, Cools AR (eds). Atypical Antipsychotics; Milestones In Drug Therapy. Birkhäuser Verlag: Basel, Boston, Berlin. pp 57–81.
Li Z, Huang M, Prus AJ, Dai J, Meltzer HY (2007). 5-HT6 receptor antagonist SB-399885 potentiates haloperidol and risperidone-induced dopamine efflux in the medial prefrontal cortex or hippocampus. Brain Res 1134: 70–78.
Liegeois JF, Ichikawa J, Meltzer HY (2002). 5-HT(2A) receptor antagonism potentiates haloperidol-induced dopamine release in rat medial prefrontal cortex and inhibits that in the nucleus accumbens in a dose-dependent manner. Brain Res 947: 157–165.
McAlonan K, Brown VJ (2003). Orbital prefrontal cortex mediates reversal learning and not attentional set shifting in the rat. Behav Brain Res 146: 97–103.
Meltzer HY, McGurk SR (1999). The effects of clozapine, risperidone, and olanzapine on cognitive function in schizophrenia. Schizophr Bull 25: 233–255.
Mitchell ES, Neumaier JF (2005). 5-HT6 receptors: a novel target for cognitive enhancement. Pharmacol Ther 108: 320–333.
Mork A, Witten LM, Arnt J (2007). Differentiating effects of sertindole and risperidone on extracellular levels of neurotransmitters in the frontal cortex of conscious rats. Program No.500. 13, 2007 Abstract Viewer/Itinerary Planner. Soc for Neurosci: San Diego, CA, 2007. Online.
Mortimer AM (1997). Cognitive function in schizophrenia—do neuroleptics make a difference? Pharmacol Biochem Behav 56: 789–795.
Natesan S, Reckless G, Nobrega J, Fletcher P, Kapur S (2006). Dissociation between in vivo occupancy and functional antagonism of dopamine D2 receptors: comparing aripiprazole to other antipsychotics in animal models. Neuropsychopharmacology 31: 1854–1863.
Olsen CK, Bennum LT, Kreilgaard M (2006). Pharmacokinetic-pharmacodynamic modeling as a tool for prediction of therapeutic effective plasma levels in antipsychotics. Program No. 95. 15, 2006 Abstract Viewer/Itinerary Planner. Soc for Neurosci: Atlanta, GA, 2006. Online.
Pantelis C, Barber FZ, Barnes TRE, Nelson HE, Owen AM, Robbins TW (1999). Comparison of set-shifting ability in patients with chronic schizophrenia and frontal lobe damage. Schizophr Res 37: 251–270.
Remillard S, Pourcher E, Cohen H (2005). The effect of neuroleptic treatments on executive function and symptomatology in schizophrenia: a 1-year follow up study. Schizophr Res 80: 99–106.
Rodefer JS (2006). The effects of antipsychotics on reversing PCP-induced deficits in a rodent attentional set-shifting task. Schizophr Res 81S: 130.
Rodefer JS, Murphy ER, Baxter MG (2005). PDE10A inhibition reverses subchronic PCP-induced deficits in attentional set-shifting in rats. Eur J Neurosci 21: 1070–1076.
Rodefer JS, Nguyen TN (2006). Naltrexone reverses age-induced cognitive deficits in rats. Neurobiol Aging, doi: 10.1016/j.neurobiolaging.2006.10.005.
Sanchez C, Arnt J (2000). Assessment of 5-HT2A and 5-HT2C antagonistic properties of newer antipsychotics. Behav Pharmacol 11: 291–298.
Sanchez C, Kreilgaard M (2004). R-citalopram inhibits functional and 5-HTP-evoked behavioural responses to the SSRI, escitalopram. Pharmacol Biochem Behav 77: 391–398.
Skarsfeldt T (1996). Differential effect of antipsychotics on place navigation of rats in the Morris water maze. Psychopharmacology 124: 126–133.
Tamminga CA, Mack RJ, Granneman GR, Silber CJ, Kashkin KB (1997). Sertindole in the treatment of psychosis in schizophrenia: efficacy and safety. Int Clin Psychopharmacol 12 (Suppl 1): S29–S35.
Tollefson GD (1996). Cognitive function in schizophrenic patients. J Clin Psychiatry 57: 31–39.
Weinberger DR, Gallhofer B (1997). Cognitive function in schizophrenia. Int Clin Psychopharmacol 12: S29–S36.
Woolley ML, Marsden CA, Fone KCF (2004). 5-HT(6) receptors. Curr Drug Targets CNS Neurol Disord 3: 59–79.
Wunsch AM, Nguyen T, Guynn L, Rodefer JR (2006). Effects of 5-HT6 antagonists on attenuating PCP-induced cognitive deficits in a rodent set-shifting (ED/ID) task. Program No. 264.24, 2006 Abstract Viewer/Itinerary Planner. Soc for Neurosci: Atlanta, GA, 2006. Online.
Zhang W, Bymaster FP (1999). The in vivo effects of olanzapine and other antipsychotic agents on receptor occupancy and antagonism of dopamine D1, D2, D3, 5-HT2A and muscarinic receptors. Psychopharmacology 141: 267–278.
Acknowledgements
This study was supported by funding and materials from H Lundbeck A/S. We thank Lindsey Guynn, Travis Moschak, Amanda Wunsch, and Matt Yorek for their technical assistance, and to Dr Keel and Dr Baxter for comments on an earlier version of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
DISCLOSURE/CONFLICTS OF INTEREST
Sertindole is a product of H Lundbeck A/S, which provided support for this study, and two authors (JJK & JA) are employed by H Lundbeck A/S. JR has previously received support from Johnson & Johnson, Roche, Pfizer, and Memory Pharmaceuticals. TN has no conflicts of interest to declare. The authors have no other actual or perceived conflicts of interest to declare.
Rights and permissions
About this article
Cite this article
Rodefer, J., Nguyen, T., Karlsson, JJ. et al. Reversal of Subchronic PCP-Induced Deficits in Attentional Set Shifting in Rats by Sertindole and a 5-HT6 Receptor Antagonist: Comparison Among Antipsychotics. Neuropsychopharmacol 33, 2657–2666 (2008). https://doi.org/10.1038/sj.npp.1301654
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.npp.1301654
Keywords
This article is cited by
-
Differential effects of d- and l-enantiomers of govadine on distinct forms of cognitive flexibility and a comparison with dopaminergic drugs
Psychopharmacology (2021)
-
Variations in Dysbindin-1 are associated with cognitive response to antipsychotic drug treatment
Nature Communications (2018)
-
The subchronic phencyclidine rat model: relevance for the assessment of novel therapeutics for cognitive impairment associated with schizophrenia
Psychopharmacology (2015)
-
Comparing the effects of subchronic phencyclidine and medial prefrontal cortex dysfunction on cognitive tests relevant to schizophrenia
Psychopharmacology (2015)
-
In vitro and in vivo characterisation of Lu AF64280, a novel, brain penetrant phosphodiesterase (PDE) 2A inhibitor: potential relevance to cognitive deficits in schizophrenia
Psychopharmacology (2014)