Abstract
In the striatum, dopamine and acetylcholine (ACh) modulate dopamine release by acting, respectively, on dopamine D2 autoreceptors and nicotinic ACh (nACh) heteroreceptors localized on dopaminergic nerve terminals. The possibility that functional interactions exist between striatal D2 autoreceptors and nACh receptors was studied with in vivo microdialysis in freely moving rats. Local perfusion of nicotine in the ventral striatum (shell of the nucleus accumbens) produced a marked increase in the extracellular levels of dopamine, which was completely counteracted by co-perfusion with either the non-α7 nACh receptor antagonist dihydro-β-erythroidine or the D2−3 receptor agonist quinpirole. Local perfusion of the D2−3 receptor antagonist raclopride produced an increase in the extracellular levels of dopamine, which was partially, but significantly, counteracted by coperfusion with dihydro-β-erythroidine. These findings demonstrate a potent crosstalk between G protein-coupled receptors and ligand-gated ion channels in dopaminergic nerve terminals, with the D2 autoreceptor modulating the efficacy of non-α7 nACh receptor-mediated modulation of dopamine release. We further demonstrate physical interactions between β2 subunits of non-α7 nicotinic acetylcholine receptors and D2 autoreceptors in co-immunoprecipitation experiments with membrane preparations from co-transfected mammalian cells and rat striatum. These results reveal that striatal non-α7 nicotinic acetylcholine receptors form part of heteromeric dopamine autoreceptor complexes that modulate dopamine release.
Similar content being viewed by others
INTRODUCTION
In the central nervous system (CNS), ligand-gated ion channels can be found presynaptically, in nerve terminals, where they control neurotransmitter release (Engelman and MacDermott, 2004). Among them, nicotinic acetylcholine (nACh) receptors constitute a particular example, as nACh receptor-mediated modulation (stimulation) of neurotransmitter release is more pronounced than the relatively low numbers of neuronal nACh receptors might predict, suggesting that this is a main function of nACh receptors in the brain (Wonnacott, 1997). Thus, nACh receptors play mostly a modulatory role in the CNS, in contrast to neuromuscular junctions and autonomic ganglia, where nACh receptors mediate postsynaptic, fast, excitatory neurotransmission (Wonnacott, 1997; Vizi and Lendvai, 1999).
Neuronal nACh receptors are heteromeric pentamers made of a heterogeneous family of eight different subunits (α3−7, β2−4). Neuronal nACh receptors can be subdivided into α-bungarotoxin-sensitive or homomeric α7 nACh receptors and α-bungarotoxin-insensitive or heteromeric non-α7 nACh receptors. In the striatum, most nACh receptors are heteromeric, containing α and β subunits. Almost all of these heteromeric receptors contain the β2 subunit, whereas α4 and α6 are the most represented α subunits (Zoli et al, 2002). Dopaminergic terminals seem to be the predominant localization of striatal nACh receptors (Wonnacott et al, 2000; Jones et al, 2001; Zoli et al, 2002) and results obtained from numerous experiments performed both in vitro (striatal synaptosomes or slices) and in vivo (microdialysis) have demonstrated that stimulation of these presynaptic nACh receptors results in dopamine (DA) release (Mifsud et al, 1989; Nakamura et al, 1992; Toth et al, 1992; Nisell et al, 1994; Sacaan et al, 1995; Clarke and Reuben, 1996; Marshall et al, 1997; Wonnacott et al, 2000; Kulak et al, 2001; Zhou et al, 2001; Ferrari et al, 2002; Grady et al, 2002; Champtiaux et al, 2003).
G-protein-coupled receptors (GPCRs) can also be found in presynaptic nerve terminals. Dopaminergic nerve terminals possess DA D2 autoreceptors, which, when stimulated, inhibit dopaminergic neurotransmission. Multiple mechanisms have been suggested to be involved in the D2 autoreceptor-mediated modulation of DA release. These include the reduction of membrane excitability by increasing a K+ conductance (Cass and Zahniser, 1991; Congar et al, 2002), the decrease of DA synthesis and packaging (Onali et al, 1988; Pothos et al, 1998) and the upregulation of the DA transporter (Gulley and Zahniser, 2003). The present study demonstrates a new and important functional mechanism that allows D2 autoreceptors to decrease dopaminergic neurotransmission, based on the existence of functional and physical interactions between D2 autoreceptors and non-α7 nACh receptors in the striatum.
MATERIALS AND METHODS
Subjects and Drugs
Male Sprague–Dawley rats, weighing 300-350 g, were used in all experiments. Animals were maintained in accordance with guidelines of the Institutional Care and Use Committee of the Intramural Research Program, National Institute on Drug Abuse, NIH. (−)-Nicotine hydrogen tartrate salt ([−]-1-methyl-2-[3-pyridyl] pyrrolidine), quinpirole hydrochloride, and raclopride tartrate were purchased from Sigma Chemical Co. (St Louis, MO); dihydro-β-erythroidine hydrobromide (DHβE) was purchased from RBI (Research Biochemicals International, Natick, MA). Cocaine HCl was obtained from the National Institute on Drug Abuse (NIDA Pharmacy, Baltimore, MD).
In Vivo Microdialysis
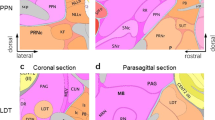
Concentric microdialysis probes were prepared as described previously (Pontieri et al, 1995). Animals were anesthetized with a solution of 4.44% chloral hydrate and 0.97% Na pentobarbital (NIDA Pharmacy, Baltimore, MD) and probes were implanted in the shell of the NAc (coordinates with respect to bregma: anterior, +2.2; lateral, −1.0; ventral, 7.7 from the dura). Experiments were performed on freely moving rats 24 h after probe implantation. All drugs were freshly dissolved in a Ringer solution (147 mM NaCl, 4 mM KCl, and 2.2 mM CaCl2) and pH was corrected when necessary. Ringer solution, either pure (during drug preperfusion and wash-out periods) or containing different concentrations of DA and nACh receptor agonists or antagonists alone or in combination (drug perfusion period), was pumped through the dialysis probe at a constant rate of 1 μl/min and samples were collected at 20-min intervals. Each animal was used to study the effect of one treatment by local administration (perfusion by reverse dialysis). At the end of the experiment, rats were killed with an overdose of Equithesin and methylene blue was perfused through the probe. The brain was removed and placed in a 10% formaldehyde solution, and coronal sections were cut to verify probe location. Dialysate DA content was measured by reverse high-performance liquid chromatography coupled to an electrochemical detector, as described in detail previously (Pontieri et al, 1995). The statistical analysis used was the ‘summary measures’ method (Matthews et al, 1990), using the mean of the three values previous to drug administration (basal value) and the mean of the three values during drug perfusion (perfusion value) per animal as the summary measures. Repeated measures analysis variance (ANOVA) (one-way and two-way) with Bonferroni post hoc comparisons were used to analyze differences within (basal vs perfusion) and between treatments (GraphPad-Prism version 4 software, San Diego, CA). The p-values shown in the figures refer to differences between basal vs perfusion values for each treatment.
Plasmid Constructs
The myc epitope (EQKLISEEDL) was introduced between Thr32 and Arg33, after the signal peptide (Met1-Ser27), of the human α4 subunit of the nACh receptor (kindly provided by JM Lindstrom, Department of Neuroscience, University of Pennsylvania Medical School, Philadelphia, PA) using a PCR mutagenesis approach (Ferré et al, 2002) and cloned into the HindIII/EcoRI sites of pcDNA3.1 (Invitrogen, Carlsbad, CA, USA). The cDNA encoding the human β2 subunit of the nACh receptor (also provided by JM Lindstrom) was cloned into the EcoRI site of pcDNA3.1. The human D2S receptor containing a hemaglutinin (HA) epitope (YPYDVPDYALV) between Asp2 and Pro3 (kindly provided by SL Milgram, Department of Cell and Molecular Physiology and the Curriculum in Neurobiology, The University of North Carolina at Chapel Hill, Chapel Hill, NC) was cloned into HindIII/XbaI sites of pcDNA3.1. The sequences of the cDNAs and their orientation in the vectors were confirmed by DNA sequencing.
Antibodies
The primary antibodies were: goat anti-α4 nACh receptor polyclonal antibody (A-20; Santa Cruz Biotechnology Inc., Santa Cruz, CA), rabbit anti-β2 nACh receptor polyclonal antibody (H-92; Santa Cruz Biotechnology), rat anti-β2 nACh receptor monoclonal antibody (Clone mAb270; Sigma), rabbit anti-D2 receptor polyclonal antibody (D2-246-316; previously; Bjelke et al, 1996), mouse anti-c-myc monoclonal antibody (Clone 9E10; Sigma), mouse anti-HA monoclonal antibody (Clone 12CA5; Roche Applied Sciences, Nutley, NJ). The secondary antibodies were: horseradish-peroxidase (HRP)-conjugated goat anti-rabbit IgG (Pierce, Rockford, IL), HRP-conjugated rabbit anti-goat IgG (Pierce), and HRP-conjugated anti-rabbit IgG TrueBlot™ (eBioscience, San Diego, CA).
Cell Culture, Transfection and Membrane Preparation
HEK-293 cells were grown in DMEM (Sigma) supplemented with 1 mM sodium pyruvate, 2 mM L-glutamine, 100 U/ml penicillin/streptomycin, 10% (v/v) foetal bovine serum at 37°C, and in an atmosphere of 5% CO2. Cells were passaged when 80–90% confluent. For the transient expression of proteins, HEK-293 cells growing in 25 cm2 flasks were transiently transfected with 3 μg of DNA by calcium phosphate precipitation (Jordan et al, 1996). Membrane suspensions from rat striatum or from transfected HEK cells were obtained as described previously (Casadó et al, 1990; Burgueño et al, 2004).
Immunoprecipitation and Western Blot
Rats were killed with an overdose of Equithesin and the brain was rapidly removed and striata dissected out. Membranes from transiently transfected HEK cells or rat striatum were solubilized in ice-cold lysis buffer (PBS, pH 7.4, containing 1% (v/v) Nonidet P-40) for 30 min on ice. Solubilized preparations were then centrifuged at 13 000g for 30 min. Supernatant (1 mg/ml) was processed for immunoprecipitation as described previously (Burgueño et al, 2003; Ferré et al, 2002), each step conducted with constant rotation at 0–4°C, and incubated overnight with the indicated antibody. Forty microliters of a suspension of protein G crosslinked to agarose beads were added and the mixture was incubated overnight. Beads were washed twice with ice-cold lysis buffer, twice with ice-cold lysis buffer containing 0.1% (v/v) Nonidet P-40, once with ice-cold Tris-buffered saline, pH 7.4, and aspirated to dryness with a 28-gauge needle. Subsequently, 30 μl of sodium dodecyl sulfate (SDS)-PAGE sample buffer (8 M Urea, 2% SDS, 100 mM DTT, 375 mM Tris, pH 6.8) was added to each sample. Immune complexes were dissociated by heating to 37°C for 2 h and resolved by SDS-polyacrylamide gel electrophoresis in 10% gels. Proteins were transferred to polyvinylidene difluoride (PVDF) membranes using a semidry transfer system and immunoblotted with the indicated primary antibody and then the appropriate HRP-conjugated goat secondary antibody. Immunoreactive bands were developed using a chemiluminescent detection kit.
RESULTS
Nicotine-Induced DA Release in the NAc Depends on Non-α7 nACh Receptors
Basal extracellular levels of dialysate DA from the shell of the NAc were 3.7±0.2 nM (n=65). Local perfusion of 1 and 10 mM of nicotine in the NAc markedly increased extracellular levels of DA (ANOVA: p<0.001 in both cases; maximal increases of about 600% and 300% from basal values, respectively). The concentration of 1 mM of nicotine produced a significantly more potent effect than 10 mM of nicotine (two-way ANOVA: p<0.05) (Figure 1). The most effective concentration of nicotine (1 mM) was chosen for the next experiments. Perfusion with 0.1 mM, but not 0.01 mM, of the broad-spectrum non-α7 nACh receptor antagonist DHβE (Chavez-Noriega et al, 1997) produced a small but significant decrease in the extracellular concentration of DA (ANOVA: p<0.05; a maximal decrease of about 30% from basal values) (Figure 2). The simultaneous perfusion of DHβE (0.1 mM) completely counteracted the DA release induced by 1 mM of nicotine (Figure 2).
Extracellular concentrations of DA in the shell of the NAc after local perfusion of nicotine (0 (control), 0.1, 1, and 10 mM). The horizontal line shows the period of perfusion. The results represent means±SEM of the percentage of basal values of the extracellular concentrations of DA (n=4–6 per group). Basal values were the means of three values before drug perfusion. Nicotine 1 and 10 mM produced a significant increase in the extracellular concentration of DA. Nicotine 1 mM was significantly more effective than nicotine 10 mM (two-way ANOVA: p<0.05). The p-values refer to the significant differences between basal vs perfusion values for each treatment.
Extracellular concentrations of DA in the shell of the NAc after local perfusion of the non-α7 nACh receptor antagonist DHβE with or without coperfusion with nicotine (1 mM). The horizontal lines show the periods of perfusion; the upper line corresponds to nicotine and the lower line corresponds to DHβE. The results represent means±SEM of the percentage of basal values of the extracellular concentrations of DA (n=5–6 per group). Basal values were the means of three values before drug perfusion. DHβE 0.1 mM produced a significant decrease in the extracellular concentration of DA and counteracted the increase in DA levels induced by nicotine 1 mM. The p-values refer to the significant differences between basal vs perfusion values for each treatment.
DA D2 Receptor Stimulation Counteracts Nicotine-Induced DA Release
Local perfusion of 0.001 and 0.01 mM of the D2−3 receptor agonist quinpirole produced a dose-dependent decrease in extracellular levels of DA in the NAc (ANOVA: p<0.05 and p<0.001, respectively; maximal decreases of about 20 and 50% from basal values, respectively). The concentration of 0.01 mM of quinpirole produced a significantly more potent effect than 0.001 mM of quinpirole (two-way ANOVA: p<0.05) (Figure 3). When coperfused with nicotine (1 mM), the lowest effective concentration of quinpirole (0.001 mM) completely counteracted nicotine-induced DA release (Figure 4). In contrast, quinpirole (1 μM) did not significantly modify the increase in extracellular levels of DA induced by the local perfusion of cocaine (0.01 mM). Thus, cocaine produced maximal increases of about 100% from basal values in the presence and absence of quinpirole (ANOVA: p<0.01 in both cases) (Figure 4).
Extracellular concentrations of DA in the shell of the NAc after local perfusion of the D2−3 receptor agonist quinpirole. (0.001 and 0.01 mM). The horizontal line shows the period of perfusion. The results represent means±SEM of the percentage of basal values of the extracellular concentrations of DA (n=4–5 per group). Basal values were the means of three values before drug perfusion. Quinpirole 0.001 and 0.01 mM produced a significant decrease in the extracellular concentration of DA. Quinpirole 0.01 mM was significantly more effective than quinpirole 0.001 mM (two-way ANOVA: p<0.05). The p-values refer to the significant differences between basal vs perfusion values for each treatment.
Extracellular concentrations of DA in the shell of the NAc after local perfusion of nicotine (0.1 mM) or cocaine (0.01 mM), with or without coperfusion with the D2−3 receptor agonist quinpirole (0.001 mM). The horizontal lines show the periods of perfusion; the upper line corresponds to cocaine or nicotine and the lower line corresponds to quinpirole. The results represent means±SEM of the percentage of basal values of the extracellular concentrations of DA (n=5–6 per group). Basal values were the means of three values before drug perfusion. Quinpirole (0.001 mM) completely counteracted the increase in DA levels induced by nicotine 1 mM. Cocaine produced a significant increase in the extracellular concentration of DA, which was not significantly modified by quinpirole. The p-values refer to the significant differences between basal vs perfusion values for each treatment.
Non-α7 nACh Receptor Blockade Counteracts DA Release Induced by DA D2 Receptor Blockade
Local perfusion with the D2−3 receptor antagonist raclopride produced a dose-dependent increase in extracellular levels of DA in the NAc, which was significant at concentrations of 0.001 and 0.01 mM (ANOVA: p<0.01 and p<0.001, respectively; maximal increases of about 100 and 200% from basal values, respectively) (Figure 5). When coperfused with the non-α7 nACh receptor antagonist DHβE (0.1 mM), the effect of raclopride (0.01 mM) was significantly decreased (two-way ANOVA: p<0.01; to a maximal increase of DA of about 80% from basal values) (Figure 5).
Extracellular concentrations of DA in the shell of the NAc after local perfusion of the D2−3 receptor antagonist raclopride (0.0001, 0.001, and 0.01 mM) with or without coperfusion with of the non-α7 nACh receptor antagonist DHβE (0.1 mM). The horizontal lines show the period of perfusion; the upper line corresponds to raclopride and the lower line corresponds to DHβE. The results represent means±SEM of the percentage of basal values of the extracellular concentrations of DA (n=5–6 per group). Basal values were the means of three values before drug perfusion. Raclopride 0.001 and 0.01 mM produced a significant increase in the extracellular concentration of DA. DHβE significantly decreased the increase in the extracellular concentration of DA induced by raclopride (0.01 mM) (two-way ANOVA: p<0.01). The p-values refer to the significant differences between basal vs perfusion values for each treatment.
Co-immunoprecipitation of Non-α7 nAChRs and D2 Autoreceptors from Co-Transfected HEK Cells and Striatal Tissue
The possible existence of heteromeric receptor complexes between α4 or β2 subunits of the non-α7 nACh receptors and the D2 autoreceptor, which corresponds to the short isoform of the D2 receptor or D2S (Khan et al, 1998; Usiello et al, 2000; Rougé-Pont et al, 2002), was first studied in transiently co-transfected HEK cells. In extracts of cells transfected with α4-myc subunit, mouse anti-c-myc antibody immunoprecipitate revealed a band of ∼70 kDa, which corresponds to the α4 subunit of the human nACh receptor (Figure 6a). In extracts of cells transfected with β2 subunit, rat anti- β2 nACh receptor antibody immunoprecipitate revealed a band of ∼55 kDa, which corresponds to the β2 subunit of the human nACh receptor (Figure 6a). In extracts of cells transfected with D2S-HA receptor, mouse anti-HA antibody immunoprecipitate revealed a broad band of ∼55–75 kDa, which corresponds to the human DA D2S receptor (Figure 6a). This broad immunoblot detection of D2S receptor most probably represents the different glycosylated states that this receptor shows when expressed in a heterologous system, as described previously (Fishburn et al, 1995). In extracts from cells co-transfected with α4-myc and β2 subunits, anti-c-myc antibody co-immunoprecipitated the β2 subunit of the nACh receptor and anti- β2 antibody co-immunoprecipitated the α4 subunit of the nACh receptor (Figure 6a). Thus, as expected, in co-transfected HEK cells, α4 and β2 subunits form heteromeric complexes. When D2S-HA receptor was co-transfected with both α4-myc and β2 subunits, anti-c-myc and anti- β2 antibodies were able to co-immunoprecipitate the D2S receptor and, conversely, mouse anti-HA antibody co-immunoprecipitated α4 and β2 subunits of the nACh receptor (Figure 6a). Importantly, the α4 subunit of the nACh receptor did not co-immunoprecipitate with D2S receptor in the absence of the β2 nACh receptor subunit (Figure 6a), indicating that the D2S receptor is able to establish heteromeric complexes with the nACh receptor by selectively interacting with the β2 subunit.
Co-immunoprecipitation of nACh and D2 receptors. (a) HEK-293 cells transiently transfected with the indicated human cDNAs were solubilized and processed for immunoprecipitation (IP) with mouse anti-myc (1 μg), rat anti-β2 nAch receptor (1 μg), and mouse anti-HA (1 μg) antibodies. Immunoprecipitates were analyzed by SDS-PAGE and immunoblotted (IB) using goat anti-α4 nACh receptor antibody (1/500), rabbit anti-β2 nACh recepor antibody (1/500), and rabbit anti-D2 receptor antibody (1/2000). The immunoreactive bands were visualized by chemiluminescence. (b) Rat striatal membranes were solubilized and processed for IP with rabbit irrelevant IgG (lane 1), rabbit anti-D2 receptor polyclonal antibody (lane 2), and rabbit anti-β2 nACh receptor polyclonal antibody (lane 3). Immunoprecipitates were analyzed by SDS-PAGE and IB using rabbit anti-D2 receptor antibody (1/2000) and rabbit anti-β2 nACh receptor antibody (1/500). A HRP-conjugated anti-rabbit IgG TrueBlot™ was used as a secondary antibody in order to avoid IgG crossreactivity. The immunoreactive bands were visualized by chemiluminescence.
We then analyzed the possible existence of heteromeric complexes in native brain preparations. To this end, we carried out similar co-immunoprecipitation experiments in soluble extracts from rat striatal membranes. As displayed in Figure 6b, the rabbit anti-β2 nACh receptor antibody immunoprecipitated a band of ∼55 kDa corresponding to the β2 nACh receptor (Figure 6b, lane 3, IB:β2) (similar results were found using the rat anti-β2 nACh receptor antibody, data not shown) and the rabbit anti-D2 receptor antibody immunoprecipitated a broad band of ∼75-90 kDa corresponding to the D2 receptor (Figure 6b, lane 2, IB:D2), as expected. Again, several glycosylated states of the D2 receptor tissue have been described in native brain (Clagett-Dame and McKelvy, 1989; Bjelke et al, 1996), which matches our current results. The divergence in D2 receptor size between native tissue and transient expression might reflect the different glycosylation machinery in both systems. Importantly, the anti-D2 receptor antibody was able to co-immunoprecipitate the β2 subunit of the nACh receptor (Figure 6b, lane 2, IB:β2) and, conversely, the rabbit anti-β2 nACh receptor antibody co-immunoprecipitated the D2 receptor (Figure 6b, lane 3, IB:D2) (similar results were found using the rat anti-β2 nAChR antibody, data not shown). Although the D2 receptor antibody used in these experiments does not differentiate between the short and long isoforms of D2 receptor (D2S and D2L, respectively), in the striatum the β2 subunits only colocalize with the D2S receptor in the dopaminergic cell terminals (see Discussion). Therefore, these results indicate that heteromeric receptor complexes of D2 autoreceptors and nACh receptors containing β2 subunits are present in the striatum in native tissue, corroborating the previous results in transiently transfected cells.
DISCUSSION
In agreement with previous findings (Mifsud et al, 1989; Nakamura et al, 1992; Toth et al, 1992; Nisell et al, 1994; Marshall et al, 1997; Ferrari et al, 2002), we found that local perfusion of nicotine in the striatum (NAc) significantly increases the extracellular concentration of DA. Two main mechanisms that may be involved in this effect of nicotine have been suggested: (1), a direct stimulation of DA release by the activation of non-α7 nACh receptors localized in dopaminergic terminals and (2), stimulation of DA release secondary to glutamate release (and activation of ionotropic glutamate receptors in the dopaminergic terminals) by the activation of α7 nACh receptors localized in glutamatergic terminals (Toth et al, 1992; Kaiser and Wonnacott, 2000; Wonnacott et al, 2000; Zhou et al, 2001; Champtiaux et al, 2003; Rassoulpour et al, 2005). Our finding that the non-α7 nACh receptor antagonist DHβE completely counteracted nicotine-induced DA release demonstrates that non-α7 nACh receptors play a fundamental role in the local DA-releasing effects of nicotine in the NAc. In fact, most striatal nACh receptors are heteromeric non-α7 nACh receptors (Zoli et al, 2002).
As in a recent study by Ferrari et al, (2002) we found that the extracellular concentration of DA in the NAc remained elevated during the whole period of nicotine perfusion (60 min) and went back to basal levels when nicotine perfusion was stopped. This effect was completely dependent on functional nACh receptors, as it was blocked with the nACh antagonist DHβE. These results are difficult to reconcile with the results obtained using in vitro models (fast voltametry in striatal slices), which suggest that exposure to DA induces a fast and potent desensitization of striatal non-α7 nACh that modulate DA release and that nicotine behaves as a non-α7 nACh receptor antagonist (Zhou et al, 2001; Rice and Cragg, 2004). This suggests that the in vitro models (striatal slices) do not adequately model the in vivo situation. Nevertheless, in our study, desensitization could play some role in the weaker effects of nicotine at higher concentrations.
In previous in vivo microdialysis experiments, local perfusion with the non-selective nACh receptor antagonist mecamylamine was reported to be ineffective or even to induce an increase in striatal extracellular levels of DA (Nakamura et al, 1992; Nisell et al, 1994; Marshall et al, 1997; Fu et al, 2000). However, mecamylamine is nonselective, acting on both α7 and non-α7 nACh receptors, and also has been shown to block NMDA receptors (Snell and Johnson, 1989). To our knowledge, this is the first report of the effects of local perfusion in the NAc of a selective non-α7 nACh receptor antagonist, DHβE, which produced a small but significant decrease in the extracellular concentration of DA. This indicates that endogenous ACh tonically modulates DA release by acting on non-α7 nACh receptors, as previously suggested by Zhou et al, (2001).
The effects of local and systemic administration of D2 receptor agonists and antagonists on striatal DA release have been repeatedly shown in the literature (for specific effects in the NAc see, for instance, See et al, 1991; Ferré and Artigas, 1995) and they have been demonstrated to depend on D2S autoreceptors (Khan et al, 1998; Usiello et al, 2000; Rougé-Pont et al, 2002). In agreement, we found that local perfusion of the D2−3 receptor agonist quinpirole significantly decreased, whereas the D2−3 receptor antagonist raclopride increased, the extracellular concentration of DA in the NAc. A major finding of the present study was that a concentration of quinpirole (1 μM) that slightly inhibited DA release (20% below basal values) completely counteracted the very large increase in the extracellular levels of DA (about 600% above basal values) induced by nicotine in the NAc. On the other hand, the same concentration of quinpirole (1 μM) did not significantly modify cocaine-induced DA release. These findings demonstrate a potent crosstalk between GPCRs and ligand-gated ion channels in dopaminergic nerve terminals, with the D2 autoreceptor modulating the efficacy of non-α7 nACh receptor-mediated modulation of DA release. Furthermore, the significant counteractive effect of DHβE on raclopride-induced increases in the extracellular concentrations of DA strongly suggests that inhibition of non-α7 nACh striatal receptor function is a main mechanism by which D2 autoreceptors control DA release.
An increasing number of receptor interactions are being demonstrated to depend on their physical association, forming functional heteromeric receptor complexes and often heterodimers (Bouvier, 2001; Devi, 2001; Agnati et al, 2003; Lee et al, 2003). This includes the possibility of heteromeric receptor complexes of GPCRs and ligand-gated ion channels, such as the DA D1-NMDA and the DA D5-GABAA receptor interactions (reviewed in Agnati et al, 2003). The present experiments with co-transfected HEK cells demonstrate that the D2S receptor is able to establish heteromeric complexes with the nACh receptor by selectively interacting with the β2 subunit when coexpressed in the same cells. Furthermore, an antibody against the β2 subunit of the nAch receptor was able to co-immunoprecipitate D2 receptors from membrane preparations of the rat striatum and, conversely, a D2 receptor antibody was able to co-immunoprecipitate the β2 subunit of the nAch receptor. Since in the striatum the β2 subunits of the nAch receptor are mostly localized in the dopaminergic cell terminals (Wonnacott et al, 2000; Jones et al, 2001; Zoli et al, 2002), where they are colocalized with D2S autoreceptors, the present results show that non-α7 nAChRs containing β2 subunits form part of a heteromeric D2S autoreceptor complex, which exerts strong control over striatal DA release.
The term autoreceptor was introduced to define those receptors localized in nerve terminals that respond to the neurotransmitter released by the same neuron (Langer, 1974). Later, the term autoreceptor also included receptors localized in the somatodendritic region that respond to somatodendritic neurotransmitter release (Aghajanian and Bunney, 1977). Functionally, autoreceptors act as a feedback mechanism inhibiting neurotransmitter release. The term heteroreceptor is used for presynaptic receptors capable of regulating (stimulating or inhibiting) the release of neurotransmitter other than their own, which is one of the main functions of nACh receptors in the central nervous system (Wonnacott, 1997). The term heteromeric autoreceptor complex expands the concepts of autoreceptor and heteroreceptor, to include them in a functional macromolecular complex. The present study shows that striatal dopaminergic neurotransmission is under the control of heteromeric autoreceptor complexes containing D2 autoreceptors and non-α7 ACh heteroreceptors. It still remains to be determined if the functional interaction between these two receptors depends on their physical interaction and if they establish a direct physical interaction (‘true heteromerization’), as co-immunoprecipitation does not discard the existence of intermediate linking proteins. Nevertheless, the experiments in co-transfected HEK cells favor the hypothesis of a selective direct interaction between β2 subunits of the nACh receptors and D2 autoreceptors, as the α4 subunit of the nACh receptor could co-immunoprecipitate with D2S receptor only in the presence of the β2 nACh receptor subunit. Otherwise, the heteromeric nACh-DA autoreceptor complexes should also contain some proteins that would be constitutively expressed in HEK cells and that would physically and specifically link the β2 nACh receptor subunit to the D2S receptor. It must also be pointed out that D2 autoreceptors and non-α7 nACh receptors are not only co-localized in the terminals of dopaminergic cells but also in their soma and dendrites (Aghajanian and Bunney, 1977), suggesting that heteromeric receptor complexes are also present in the ventral tegmental area. The present study provides new evidence against the generalized simplistic notion of the neurotransmitter receptor as a single functional entity and, to our knowledge, it is the first example of presynaptic heteromeric receptor complexes that include ligand-gated ion channels and GPCRs that modulate neurotransmitter release.
References
Aghajanian GK, Bunney BS (1977). Dopamine ‘autoreceptors’: pharmacological characterization by microiontophoretic single cell recording studies. Naunyn Schmiedeberg's Arch Pharmacol 297: 1–7.
Agnati LF, Ferré S, Lluis C, Franco R, Fuxe K (2003). Molecular mechanisms and therapeutical implications of intramembrane receptor/receptor interactions among heptahelical receptors with examples from the striatopallidal GABA neurons. Pharmacol Rev 55: 509–550.
Bjelke B, Goldstein M, Tinner B, Andersson C, Sesack SR, Steinbusch HWM et al (1996). Dopaminergic transmission in the rat retina: evidence for volume transmissión. J Chem Neuroanat 12: 37–50.
Bouvier M (2001). Oligomerization of G-protein-coupled transmitter receptors. Nat Rev Neurosci 2: 274–286.
Burgueño J, Canela EI, Mallol J, Lluis C, Franco R, Ciruela F (2004). Mutual regulation between metabotropic glutamate type 1alpha receptor and caveolin proteins: from traffic to constitutive activity. Exp Cell Res 300: 23–34.
Burgueño J, Enrich C, Canela EI, Mallol J, Lluis C, Franco R et al (2003). Metabotropic glutamate type 1alpha receptor localizes in low-density caveolin-rich plasma membrane fractions. J Neurochem 86: 785–791.
Casadó V, Canti C, Mallol J, Canela EI, Lluis C, Franco R (1990). Solubilization of A1 adenosine receptor from pig brain: characterization and evidence of the role of the cell membrane on the coexistence of high- and low-affinity states. J Neurosci Res 26: 461–473.
Cass WA, Zahniser NR (1991). Potassium channel blockers inhibit D2 dopamine, but not A1 adenosine, receptor-mediated inhibition of striatal dopamine release. J Neurochem 57: 147–152.
Champtiaux N, Gotti C, Cordero-Erausquin M, David DJ, Przybylski C, Lena C et al (2003). Subunit composition of functional nicotinic receptors in dopaminergic neurons investigated with knock-out mice. J Neurosci 23: 7820–7829.
Chavez-Noriega LE, Crona JH, Washburn MS, Urrutia A, Elliott KJ, Johnson EC (1997). Pharmacological characterization of recombinant human neuronal nicotinic acetylcholine receptors h alpha 2 beta 2, h alpha 2 beta 4, h alpha 3 beta 2, h alpha 3 beta 4, h alpha 4 beta 2, h alpha 4 beta 4 and h alpha 7 expressed in Xenopus oocytes. J Pharmacol Exp Ther 280: 346–356.
Clagett-Dame M, McKelvy JF (1989). N-linked oligosaccharides are responsible for rat striatal dopamine D2 receptor heterogeneity. Arch Biochem Biophys 274: 145–154.
Clarke PB, Reuben M (1996). Release of [3H]-noradrenaline from rat hippocampal synaptosomes by nicotine: mediation by different nicotinic receptor subtypes from striatal [3H]-dopamine release. Br J Pharmacol 117: 595–606.
Congar P, Bergevin A, Trudeau LE (2002). D2 receptors inhibit the secretory process downstream from calcium influx in dopaminergic neurons: implication of K+ channels. J Neurophysiol 87: 1046–1056.
Devi LA (2001). Heterodimerization of G-protein-coupled receptors: pharmacology, signaling and trafficking. Trends Pharmacol Sci 2: 532–537.
Engelman HS, MacDermott AB (2004). Presynaptic ionotropic receptors and control of transmitter release. Nat Rev Neurosci 5: 135–145.
Ferrari R, Le Novere N, Picciotto MR, Changeux JP, Zoli M (2002). Acute and long-term changes in the mesolimbic dopamine pathway after systemic or local single nicotine injections. Eur J Neurosci 15: 1810–1818.
Ferré S, Artigas F (1995). Clozapine decreases serotonin extracellular levels in the nucleus accumbens by a dopamine receptor-independent mechanism. Neurosci Lett 187: 61–64.
Ferré S, Karcz-Kubicha M, Hope BT, Popoli P, Burgueno J, Gutierrez MA et al (2002). Synergistic interaction between adenosine A2A and glutamate mGlu5 receptors: implications for striatal neuronal function. Proc Natl Acad Sci USA 99: 11940–11945.
Fishburn CS, Elazar Z, Fuchs S (1995). Differential glycosylation and intracellular trafficking for the long and short isoforms of the D2 dopamine receptor. J Biol Chem 270: 29819–29824.
Fu Y, Matta SG, Gao W, Sharp BM (2000). Local alpha-bungarotoxin-sensitive nicotinic receptors in the nucleus accumbens modulate nicotine-stimulated dopamine secretion in vivo. Neuroscience 101: 369–375.
Grady SR, Murphy KL, Cao J, Marks MJ, McIntosh JM, Collins AC (2002). Characterization of nicotinic agonist-induced [(3)H]dopamine release from synaptosomes prepared from four mouse brain regions. J Pharmacol Exp Ther 301: 651–660.
Gulley JM, Zahniser NR (2003). Rapid regulation of dopamine transporter function by substrates, blockers and presynaptic receptor ligands. Eur J Pharmacol 479: 139–152.
Jones IW, Bolam JP, Wonnacott S (2001). Presynaptic localisation of the nicotinic acetylcholine receptor beta2 subunit immunoreactivity in rat nigrostriatal dopaminergic neurones. J Comp Neurol 439: 235–247.
Jordan M, Schallhorn A, Wurm FM (1996). Transfecting mammalian cells: optimization of critical parameters affecting calcium-phosphate precipitate formation. Nucleic Acids Res 24: 596–601.
Kaiser S, Wonnacott S (2000). Alpha-bungarotoxin-sensitive nicotinic receptors indirectly modulate [(3)H]dopamine release in rat striatal slices via glutamate release. Mol Pharmacol 58: 312–318.
Khan ZU, Mrzljak L, Gutierrez A, de la Calle A, Goldman-Rakic PS (1998). Prominence of the dopamine D2 short isoform in dopaminergic pathways. Proc Natl Acad Sci USA 95: 7731–7736.
Kulak JM, McIntosh JM, Yoshikami D, Olivera BM (2001). Nicotine-evoked transmitter release from synaptosomes: functional association of specific presynaptic acetylcholine receptors and voltage-gated calcium channels. J Neurochem 77: 1581–1589.
Langer SZ (1974). Presynaptic regulation of catecholamine release. Biochem Pharmacol 23: 1793–1800.
Lee SP, O'Dowd BF, George SR (2003). Homo- and hetero-oligomerization of G protein-coupled receptors. Life Sci 4: 173–180.
Marshall DL, Redfern PH, Wonnacott S (1997). Presynaptic nicotinic modulation of dopamine release in the three ascending pathways studied by in vivo microdialysis: comparison of naive and chronic nicotine-treated rats. J Neurochem 68: 1511–1519.
Matthews JN, Altman DG, Campbell MJ, Royston P (1990). Analysis of serial measurements in medical research. BMJ 300: 230–235.
Mifsud JC, Hernandez L, Hoebel BG (1989). Nicotine infused into the nucleus accumbens increases synaptic dopamine as measured by in vivo microdialysis. Brain Res 478: 365–367.
Nakamura S, Goshima Y, Yue JL, Miyamae T, Misu Y (1992). Transmitter-like 3,4-dihydroxyphenylalanine is tonically released by nicotine in striata of conscious rats. Eur J Pharmacol 222: 75–80.
Nisell M, Nomikos GG, Svensson TH (1994). Systemic nicotine-induced dopamine release in the rat nucleus accumbens is regulated by nicotinic receptors in the ventral tegmental area. Synapse 16: 36–44.
Onali P, Olianas MC, Bunse B (1988). Evidence that adenosine A2 and dopamine autoreceptors antagonistically regulate tyrosine hydroxylase activity in rat striatal synaptosomes. Brain Res 456: 302–309.
Pontieri FE, Tanda G, Di Chiara G (1995). Intravenous cocaine, morphine, and amphetamine preferentially increase extracellular dopamine in the ‘shell’ as compared with the ‘core’ of the rat nucleus accumbens. Proc Natl Acad Sci USA 92: 12304–12308.
Pothos EN, Przedborski S, Davila V, Schmitz Y, Sulzer D (1998). D2-like dopamine autoreceptor activation reduces quantal size in PC12 cells. J Neurosci 18: 5575–5585.
Rassoulpour A, Wu HQ, Ferré S, Schwarcz R (2005). Nanomolar concentrations of kynurenic acid reduce extracellular dopamine levels in the striatum. J Neurochem 93: 762–765.
Rice ME, Cragg SJ (2004). Nicotine amplifies reward-related dopamine signals in striatum. Nat Neurosci 7: 583–584.
Rougé-Pont F, Usiello A, Benoit-Marand M, Gonon F, Piazza PV, Borrelli E (2002). Changes in extracellular dopamine induced by morphine and cocaine: crucial control by D2 receptors. J Neurosci 22: 3293–3301.
Sacaan AI, Dunlop JL, Lloyd GK (1995). Pharmacological characterization of neuronal acetylcholine gated ion channel receptor-mediated hippocampal norepinephrine and striatal dopamine release from rat brain slices. J Pharmacol Exp Ther 274: 224–230.
See RE, Sorg BA, Chapman MA, Kalivas PW (1991). In vivo assessment of release and metabolism of dopamine in the ventrolateral striatum of awake rats following administration of dopamine D1 and D2 receptor agonists and antagonists. Neuropharmacol 30: 1269–1274.
Snell LD, Johnson KM (1989). Effects of nicotinic agonists and antagonists on N-methyl-D-aspartate-induced 3H-norepinephrine release and 3H-(1-[1-(2-thienyl)cyclohexyl]-piperidine) binding in rat hippocampus. Synapse 3: 129–135.
Toth E, Sershen H, Hashim A, Vizi ES, Lajtha A (1992). Effect of nicotine on extracellular levels of neurotransmitters assessed by microdialysis in various brain regions: role of glutamic acid. Neurochem Res 17: 265–271.
Usiello A, Baik JH, Rouge-Pont F, Picetti R, Dierich A, LeMeur M et al (2000). Distinct functions of the two isoforms of dopamine D2 receptor. Nature 408: 199–203.
Vizi ES, Lendvai B (1999). Modulatory role of presynaptic nicotinic receptors in synaptic and non-synaptic chemical communication in the central nervous system. Brain Res Brain Res Rev 30: 219–235.
Wonnacott S (1997). Presynaptic nicotinic ACh receptors. Trends Neurosci 20: 92–98.
Wonnacott S, Kaiser S, Mogg A, Soliakov L, Jones IW (2000). Presynaptic nicotinic receptors modulating dopamine release in the rat striatum. Eur J Pharmacol 393: 51–58.
Zhou FM, Liang Y, Dani JA (2001). Endogenous nicotinic cholinergic activity regulates dopamine release in the striatum. Nat Neurosci 4: 1224–1229.
Zoli M, Moretti M, Zanardi A, McIntosh JM, Clementi F, Gotti C (2002). Identification of the nicotinic receptor subtypes expressed on dopaminergic terminals in the rat striatum. J Neurosci 22: 8785–8789.
Acknowledgements
This work was supported by the National Institute on Drug Abuse Intramural Research Funds. F Ciruela is currently holding a Ramón y Cajal research contract signed with the Ministerio de Educación y Ciencia. This work was supported by Grant SAF2002-03293 to RF and SAF2005-00903 to FC from Ministerio de Educación y Ciencia.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Quarta, D., Ciruela, F., Patkar, K. et al. Heteromeric Nicotinic Acetylcholine–Dopamine Autoreceptor Complexes Modulate Striatal Dopamine Release. Neuropsychopharmacol 32, 35–42 (2007). https://doi.org/10.1038/sj.npp.1301103
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.npp.1301103
Keywords
This article is cited by
-
Role of Dopamine D2/D3 Receptors in Development, Plasticity, and Neuroprotection in Human iPSC-Derived Midbrain Dopaminergic Neurons
Molecular Neurobiology (2018)
-
Nicotinic and opioid receptor regulation of striatal dopamine D2-receptor mediated transmission
Scientific Reports (2016)
-
Responses of limbic and extrapyramidal substance P systems to nicotine treatment
Psychopharmacology (2009)
-
Region‐specific effects of N,N′‐dodecane‐1,12‐diyl‐bis‐3‐picolinium dibromide on nicotine‐induced increase in extracellular dopamine in vivo
British Journal of Pharmacology (2008)
-
The serotonin2C receptor agonist Ro-60-0175 attenuates effects of nicotine in the five-choice serial reaction time task and in drug discrimination
Psychopharmacology (2007)