Abstract
Broad evidence from preclinical and clinical research indicates that cholinergic neurotransmission contributes significantly to the generation of rapid eye movement (REM) sleep. However, a potential role of different acetylcholine receptor (AChR) subtypes for the regulation of three main aspects of REM sleep, (1) REM onset, (2) REM maintenance, and (3) generation of REMs, are not clear. In the present double-blind, randomized and placebo-controlled study, we investigated the differential effects of the M1 muscarinic AChR (mAChR) agonist RS-86 and the ACh-esterase inhibitor donepezil to further specify the AChR subtype function on REM sleep regulation in n=20 healthy volunteers. We found that RS-86 selectively shortened REM latency (multivariate analysis of variance post hoc contrast p=0.024 compared to placebo, not significant for donepezil) and that donepezil specifically enhanced the duration of REM sleep (% sleep period time, p=0.000 compared to placebo; p=0.003 compared to RS-86) and the number of REMs (p=0.000 compared to placebo; p=0.000 compared to RS-86). These results provide evidence that the onset of REM sleep is, in part, mediated by M1 mAChR activity, whereas the maintenance of REM sleep and the number of REMs are mediated by non-M1, but presumably M2 mAChR activity. These findings are of interest for the understanding of sleep regulation and of neuropsychiatric disorders, such as Alzheimer's dementia and depressive disorders, whose etiopathology may involve alterations in cholinergic neurotransmission.
Similar content being viewed by others
INTRODUCTION
Broad evidence from preclinical and clinical research indicates that cholinergic neurotransmission contributes significantly to the generation of rapid eye movement (REM) sleep. Preclinical studies show that the medial pontine reticular formation (mPRF) plays a key role in REM sleep generation. In this region, microinjection of cholinergic agonists causes a REM sleep-like state that is blocked by muscarinic acetylcholine receptor (mAChR) antagonists (reviewed in Baghdoyan and Lydic, 2002). In the same region, in vivo microdialysis data reveal that acetylcholine (ACh) release is enhanced during REM sleep (Leonard and Lydic, 1997). ACh release in the mPRF arises from the more rostral and dorsal cell groups comprising the laterodorsal (LDT) and the pedunculopontine tegmental (PPT) nuclei (Lydic and Baghdoyan, 1993). Consistently, LDT/PPT neurons demonstrate higher discharge rates during REM sleep (el Mansari et al, 1989). In humans, REM sleep is enhanced after administration of ACh-esterase inhibitors (Sitaram et al, 1976; Riemann et al, 1994) or cholinergic agonists (Spiegel, 1984; Riemann et al, 1988) and inhibited by anticholinergics (Sagales et al, 1969).
Recent studies show that different aspects of REM sleep, including (1) the number of rapid eye movements (number of REMs), (2) maintenance (REM sleep duration), and (3) onset (REM latency), can be individually evoked (eg Quattrochi and Hobson, 1999). In this process, differential activation of ACh receptor (AChR) subtypes may play a crucial role. In a widely accepted view, mAChRs are more relevant for REM sleep regulation than nicotinic AChRs (reviewed in Baghdoyan and Lydic, 2002). Actually, five mAChRs (M1–M5) have been molecularly and pharmacologically identified (Caulfield and Birdsall, 1998), with the M1 and M2 mAChRs being the most abundant subtypes in mammalian cortex (Levey et al, 1991). The lack of specific ligands for each subtype makes pharmacological studies difficult, but inferences can be made for a specific function by comparing the potencies of different compounds with known affinities for M1–M5 mAChRs.
REMs represent higher level analogs of ponto-geniculo-occipital (PGO) waves (Pare et al, 1990). The number of REMs is predominantly determined by M2 mAChRs. Microinjections of the unspecific cholinergic agonist carbachol in anterior parts of the caudal peribrachium (C-PB) of the rat enhance PGO wave activity (Datta et al, 1992; Calvo et al, 1992). Cholinergically evoked PGO waves were blocked by the M2 mAChR antagonist methoctramine, suggesting mediation via this receptor subtype (Datta et al, 1993).
Also, REM sleep maintenance (REM duration) appears to be predominantly mediated by M2 mAChRs. Microinjecting the ACh-esterase inhibitor neostigmine into medial regions of the mouse PRF causes a REM sleep-like state that is blocked by the M2/M4 antagonist methoctramine but not by the M1/M4 antagonist pirenzepine, indicating M2 mAChR mediation (Coleman et al, 2004). Additionally, the M3 mAChR subtype in the perilocus coeruleus alpha region of the cat pons contributed to REM sleep generation (Sakai and Onoe, 1997). Findings from studies in cats (Shuman et al, 1995; Baghdoyan and Lydic, 1999) and rats (Marks and Birabil, 2000) support that the cholinergically induced REM sleep-like state is mediated substantially by signal transduction pathways coupled to M2 (and less M4) but not M1 mAChRs. Consistently, of the five mAChR subtypes (M1–M5), the M2 subtype is predominant in the PRF of cats (Baghdoyan et al, 1994), rats (Baghdoyan, 1997), and humans (Cortes et al, 1986).
Owing to paucity of preclinical data, mAChR subtypes involved in the initiation of REM sleep (REM latency) are less well known. In humans, numerous ACh-esterase inhibitors (eg physostigmine: Sitaram et al, 1976; galanthamine: Riemann et al, 1994) and selective M1 mAChR agonists, like pilocarpine (Berkowitz et al, 1990) or RS-86 (Riemann et al, 1988), shorten REM latency. Gillin et al (1991) demonstrated that low doses of the M1 antagonist biperiden selectively enhanced REM latency without affecting REM duration. Only higher doses of biperiden associated with reduced M1 selectivity and increasing M2 antagonism decreased the duration of REM sleep. The number of REMs was consistently not altered by M1-selective agents in healthy volunteers. These findings indicate that the initial occurrence of REM sleep during night sleep relates to M1 mAChR activity. However, insufficient data are available to specify the impact of other mAChR subtypes.
Direct parallels between preclinical and human studies are not always possible. In preclinical studies, pharmacological agents are typically administered to discrete neuronal populations, such as the mPRF. In human studies, agents have to be administered systemically, making it more difficult to define the location of action. Given the decisive role of pontine M2 mAChRs on REM sleep regulation in preclinical studies, we presume that orally administered cholinergic agents in humans exert parallel effects at the brainstem level. However, other effects may be mediated by AChRs located in other areas of the brain. Importantly, recent functional neuroimaging studies support a role for limbic and paralimbic structures in REM sleep function (Nofzinger et al, 1997; Maquet et al, 1996; Braun et al, 1997), raising the possibility that mAChRs in these regions mediate, in part, the effects of systemically administered cholinergic agents. Notably, limbic and paralimbic areas are rich in M1 mAChRs (Mash et al, 1988; Cortes et al, 1986), raising the possibility that M1 mAChRs modulate REM sleep via an indirect pathway on limbic receptors.
The aim of the present study was to further specify the role of mAChR subtypes involved in REM sleep regulation in humans. For this purpose, RS-86 and donepezil were chosen as pharmacological agents due to their convenient pharmacokinetic and pharmacodynamic properties. RS-86 is a direct M1 mAChR agonist with low affinities to M2–M5 mAChRs, nicotinic AchRs, or other receptors (in vitro and in vivo studies: Palacios et al, 1986; Wanibuchi et al, 1990; Rupniak et al, 1992). Donepezil enhances nonspecifically the neurotransmission on all M1–M5 mAChR and nicotinic AChR by inhibiting the Ach-esterase. Since specific M2 mAChR agonists are lacking and given that nicotinic and M3–M5 AChRs are less involved in REM sleep regulation, the comparison of RS-86 and donepezil provides an indirect paradigm to investigate the effects of M1 and M2 mAChRs on REM sleep regulation in humans. Following the preclinical and clinical data presented above, we hypothesized that donepezil would shorten REM latency and enhance the duration of REM sleep and the number of REMs, and that RS-86 would selectively shorten REM latency but not affect REM sleep duration or the number of REMs.
SUBJECTS AND METHODS
Subjects
Twenty healthy volunteers, 10 men and 10 women, aged 21–37 years (mean±standard deviation (SD), 27.1±4.6 years), were included in the present study. All participants underwent an extensive physical examination, including an electrocardiogram (ECG), electroencephalogram (EEG), and routine laboratory screening to rule out any somatic disorder. In addition, a urine drug screening demonstrated that all participants were free of any benzodiazepines, barbiturates, amphetamines, or opiates. Only women with a negative pregnancy test and sufficient contraception were included. No participant presented any contraindication for cholinergic drugs. All subjects underwent an extensive psychiatric evaluation, including a Structured Clinical Interview for Diagnosis (SCID) and a thorough clinical evaluation of the family history by an experienced psychiatrist. Subjects with a personal or family history of psychiatric disorders or primary sleep disorders according to DSM-IV were excluded. All subjects were completely free of any medication, drank no alcohol during the period of the study, and were nonsmokers. Caffeine intake was limited to one cup of coffee in the morning. A sleep diary ensured that subjects' typical sleep schedules approximated the imposed sleep schedule in the laboratory. All participants were informed in detail and provided their written and valid informed consent prior to the onset of the study. The study had been approved by the local ethic committee and has been carried out in accordance with the Declaration of Helsinki.
Experimental Design
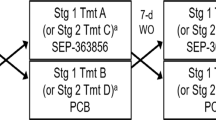
All participants spent two blocks of three nights in the sleep laboratory (blocks I and II). Between the two blocks in the sleep laboratory, participants slept at home for 2 weeks. The first night in each block served as adaptation to the sleep laboratory conditions. Furthermore, the first night in the sleep laboratory was used to rule out any sleep abnormalities. In the second and third night of each block, participants received 1.5 mg RS-86 or placebo (block I) and 10 mg donepezil or placebo (block II) at 2200 hours, 1 h prior to ‘light-off’ time at 2300 hours. The administration of RS-86/placebo and donepezil/placebo followed a randomized double-blind protocol within each block. For statistical analyses of EEG sleep data, the placebo night of block I, the RS-86 night of block I, and the donepezil night of block II were used. Owing to the long half-life of donepezil (approximately 70 h), the placebo condition of block II was excluded from analyses. Since there was no intervention between blocks I and II in the sleep laboratory that might affect baseline EEG sleep measures, we used the placebo night of block I as a control night of sleep for both the RS-86 and donepezil intervention nights.
Substance Description and Properties
RS-86
The spiro-piperidyl derivate RS-86 is a specific and direct M1 mAChR agonist with low or no affinities to other receptors (in vitro and in vivo studies: Palacios et al, 1986; Wanibuchi et al, 1990; Rupniak et al, 1992). It is efficiently absorbed with oral administration, reaches peak plasma concentrations in 2–3 h, and has an elimination half-life of 6–8 h (Spiegel, 1984). Owing to its pharmacodynamic profile, RS-86 causes no or only minor peripheral side effects in doses up to 2 mg. Side effects in higher doses include cholinomimetic symptoms, such as increased salivation, sweating, nausea, or diarrhea. No serious side effects were observed in studies using up to 20 mg RS-86 (Spiegel, 1984). Based on pharmacological data and following previous studies (eg Riemann et al, 1988), 1.5 mg RS-86 was administered orally at 2200 hours, 1 h prior to ‘light-off’ time at 2300 hours.
Donepezil
Donepezil is widely used in the treatment of Alzheimer's dementia. It is a piperidine derivate that selectively and reversibly inhibits the enzyme ACh-esterase enhancing neurotransmission on all AChR subtypes. Donepezil is well absorbed with oral administration, reaches peak plasma concentrations in 3–4 h, and has an elimination half-life of around 70 h. Potential side effects include cholinomimetic symptoms, like nausea, vomiting, and diarrhea (in up to 5% of subjects). Following pharmacological properties and in parallel to RS-86 (double-blind design), 10 mg donepezil were administered orally at 2200 hours, 1 h prior to ‘light-off’ time at 2300 hours.
Sleep Recordings
Sleep recordings were performed from 2300 to 0700 hours and scored according to standard criteria (Rechtschaffen and Kales, 1968) by experienced and blinded raters. All raters participate in weekly meetings discussing and solving scoring problems. Inter-rater reliability for all technicians involved in scoring polysomnograms is checked bimonthly. Coefficients of agreement between two raters are required to be higher than 85%. The following variables of sleep continuity and architecture were assessed: sleep onset latency was defined as the period between when the lights were turned out and the first 30 s epoch of sleep stage 2 (sleep latency); sleep period time was defined as the period between sleep onset and the final awakening (SPT); sleep efficiency was defined as the ratio of time in bed to total sleep time × 100% (SE); time spent in waking referred to SPT in percent, waking (%SPT); and time spent in sleep stages 1, 2, and slow wave sleep (SWS) (combined stages 3 and 4) referred to SPT in percent, 1 (%SPT), 2 (%SPT), and SWS (%SPT). REM sleep variables: REM sleep duration in percent referred to sleep period time REM (%SPT); averaged duration of single REM sleep periods (DREMPs); number of REMs across the whole night (number of REMs); REM density was calculated as the ratio of 3 s miniepochs per REM period including REMs to the total amount of miniepochs per REM period × 100% (REMD); REM sleep latency was defined as the period between sleep onset and the occurrence of the first 30 s epoch of REM sleep, including intermittent waking times (REM latency); and number of REM/NREM cycles (REM/NREM). Note that the number of REM/NREM cycles requires the occurrence of NREM sleep after REM sleep and may, thus, be lower (−1) than the number of REM periods when REM sleep was the last sleep stage of a night.
Data Analysis
Descriptive presentation of the data includes the mean values and SDs. To evaluate the effects of RS-86 and donepezil on sleep variables in comparison with the placebo, a multivariate analysis of variance (MANOVA) was conducted, treating the three conditions (placebo, RS-86, and donepezil) as a repeated measure. To determine differences between the conditions, post hoc contrasts were calculated for the three conditions. For the exploratory analysis of the latencies of subsequent REM periods (Figure 4), t-tests for dependent samples were used. All statistical analyses were performed with the SPSS 12 program package. The level of significance was set at p<0.05 (two-tailed).
RESULTS
REM Sleep Parameters
A repeated measures ANOVA revealed a significant intervention effect (placebo, RS-86, and donepezil) for multivariate testing (Wilk's Lambda, F(12,66)=5.7; p=0.000). As can be seen in Table 1, Donepezil enhanced the duration of REM sleep referred to sleep period time (SPT REM%) across the whole night and the number of REMs (REMs) compared to both placebo and RS-86. Furthermore, donepezil increased the averaged duration of single REM sleep periods (DREM period) in comparison to RS-86, but not to placebo. In contrast, RS-86 did not alter the parameters of REM sleep duration or the number of REMs. As the increase in the number of REMs after administration of donepezil exceeded the increase in REM sleep duration, REM density was significantly increased in the donepezil condition in relation to placebo and RS-86. RS-86, but not donepezil, significantly reduced REM latency relative to the placebo night (averaged reduction 22.9 min), but not to the donepezil night. This effect persisted after the exclusion of a REM latency in one subject (250 min) that exceeded a normal range (post hoc contrasts placebo-RS-86: p=0.044; placebo–donepezil: p=0.113). Subjects in the RS-86 condition had an increased number of REM/NREM cycles compared to the placebo, but not to the donepezil condition.
Figures 1, 2 and 3 depict single values of the main findings of the present study: the number of REMs, REM duration (%SPT), and REM latency.
Figure 4 demonstrates the cyclic pattern of REM/NREM sleep regulation. All time spans from sleep onset to the occurrence of the first (see above) and subsequent REM sleep periods (REM latency 2, 3, and 4) were significantly shortened after the administration of RS-86 compared to baseline, but not compared to donepezil (Table 2). However, the calculated multiple t-tests for dependent samples have just exploratory but not confirmative value. Given that RS-86 did not alter the averaged duration of single REM sleep periods, RS-86 appeared to advance the onset of the REM/NREM cycle. Donepezil did not significantly influence the temporal distribution of single REM sleep periods.
Sleep Continuity and Sleep Architecture of NREM Sleep
A repeated measures ANOVA revealed a significant substance effect (placebo, RS-86, and donepezil) for multivariate testing (Wilk's Lambda, F(12,64)=5.6; p=0.000). As can be seen in Table 3, parameters of sleep continuity (sleep latency, sleep period time, sleep efficiency, waking time %) were not relevantly altered after the administration of RS-86 or donepezil. The only significant effect on NREM sleep architecture was observed for donepezil, leading to a significant reduction of stage 2 (% SPT) referred to placebo and RS-86 (post hoc contrasts p=0.003; p=0.000, respectively).
DISCUSSION
The present study was designed to further specify the role of AChR subtypes on different components of human REM sleep by using the ACh-esterase inhibitor donepezil and the M1 mAChR agonist RS-86 as pharmacological challenges in comparison to placebo. The results support the initial hypotheses that the number of REMs and the duration of REM sleep are predominantly mediated by non-M1, but presumably M2 mAChR activation and that the initiation of REM sleep (REM latency) is, to a significant extent, mediated by activation of M1 mAChRs.
Prior to discussing these effects on REM sleep regulation in more detail, it is important to note that no changes in sleep continuity, such as sleep onset latency, sleep period time, or awakenings, were observed. The following alterations in REM sleep parameters, therefore, are due to REM sleep-generating mechanisms and not to alterations in sleep continuity.
Evidence that the number of REMs and REM sleep maintenance (REM sleep duration of the whole night and averaged duration of single REM sleep periods) are mediated by AChRs others than M1 mAChRs is that in the present study, the nonspecific activation of AChRs by donepezil largely enhanced the number of REMs and REM sleep maintenance, whereas the selective M1 mAChR agonist RS-86 did not alter these parameters (Figures 1 and 2). These findings are consistent with those from previous clinical (Sitaram et al, 1976; Riemann et al, 1994; Schredl et al, 2001; Kanbayashi et al, 2002) and preclinical studies (eg Calvo et al, 1992). They showed an increase of the number of REMs and REM sleep maintenance after the administration of numerous ACh-esterase inhibitors. Also, preclinical (Velazquez-Moctezuma et al, 1991; Coleman et al, 2004) and clinical (Riemann et al, 1988; Gillin et al, 1991) studies have shown that compounds with a selective affinity for M1 mAChRs did not affect these parameters. In contrast, the ACh-esterase inhibitor tacrin did not significantly affect REM density or duration (Riemann et al, 1996). This raises the possibility that differences between compounds with the same pharmacodynamic profile might be related to differences in pharmacokinetic properties between agents, such as the short half-life of tacrin (2 h). Furthermore, the frequently used parameter REM density is less adequate to reflect alterations in the generation of REMs itself since it depends on the REM sleep duration. Given that the M1 and M2 mAChR subtype are the most abundant AChR subtypes in the mammalian cortex (Levey et al, 1991), and given that there is broad evidence from preclinical studies indicating that the number of REMs and REM maintenance are predominantly mediated by M2 mAChR activity in the brain stem (Velazquez-Moctezuma et al, 1991; Coleman et al, 2004), it is likely to assume that the increases in the number of REMs and REM sleep duration observed after the administration of donepezil in the present study are mediated, to a large extent, by M2 mAChR activation at the brain stem level.
Evidence that the onset of REM sleep is mediated, at least in part, by M1 mAChR activity is that the selective M1 mAChR agonist RS-86 significantly shortened REM latency compared to placebo (mean reduction 22.9 min). This finding is consistent with those of previous studies investigating the effects of RS-86 on REM latency in healthy subjects (Riemann et al, 1988; Lauer et al, 2004). The finding that numerous ACh-esterase inhibitors shorten REM latency (eg physostigmine; Sitaram et al, 1976) is consistent but does not further contribute to the discussion of the involvement of AChR subtypes. As in previous studies in younger healthy subjects (Kanbayashi et al, 2002; Perlis et al, 2002), donepezil did not significantly alter REM sleep latency in comparison to placebo. The tendency towards a reduction in REM latency by donepezil in our sample (p=0.063) may reflect a weak activation of M1 mAChRs that may reach significance if a larger sample size were studied. The absence of a statistically significant reduction in REM latency by donepezil, therefore, may represent a false-negative result, or a type II error. The finding that donepezil clearly shortened REM latency in depressed subjects (Perlis et al, 2002) points to a differential responsiveness to cholinergic agents based on history of depressive disorder. Interestingly, RS-86, after advancing the onset of the first REM period, also appeared to advance the occurrence of succeeding REM periods relative to sleep onset even when the duration of each REM/NREM cycle was unaffected. This constellation resulted in a significant increase of the number of REM/NREM cycles per night in the RS-86 compared to placebo condition (Table 1). This advance in the REM/NREM cycle without affecting the phase duration was also observed in a previous RS-86 study (Riemann et al, 1988). In this study, the observed increase in averaged REM sleep duration was clearly related to the advancement of the REM sleep cycle and the resulting increase of the number of REM/NREM cycles, rather than to an increase in the duration of single REM sleep periods. However, the observation that the M1 mAChR agonism by RS-86 advances the onset of succeeding REM periods was in our study tested only on an exploratory level (repeated t-tests for nonprimary hypotheses). This finding requires replication.
The present study has several limitations: First, as specific ligands for each nicotinic and M1–M5 mAChR subtype are lacking, the present study provides direct evidence only for the M1 mAChR function. Owing to this, it seemed plausible to link the donepezil data of the present study to preclinical findings and postulate indirectly a mediation of REMs and REM sleep maintenance by M2 mAChRs. However, other nicotinic or mAChRs may be involved. Secondly, the finding that donepezil did not significantly shorten REM latency may be related to its pharmacokinetic properties since it reaches plasma peak concentrations 3–4 h after administration (RS-86: 2–3 h). This pharmacokinetic profile makes it even more plausible that the absence of a statistically significant reduction in REM latency by donepezil represents a false-negative result. However, it is important to note that the pharmacokinetic properties of RS-86 and donepezil do not impede the main conclusions of the present study (M1 mAChR involvement in REM sleep onset; non-M1 but presumably M2 mAChR involvement in REM sleep maintenance and generation of REMs). The third limitation is that it is not possible to determine the location of action of the systematically administered compounds. M2 mAChRs are predominantly located in the brainstem leading to the hypothesis that the effects observed in the present study are, in part, evoked in this area. However, M2 mAChRs are located in other areas of the brain and have been localized not only postsynaptically but also to the presynaptic terminals of cortical neurons (reviewed in Levey, 1996). Interestingly, recent functional neuroimaging studies have demonstrated that limbic and paralimbic structures are activated during REM sleep (Nofzinger et al, 1997; Maquet et al, 1996; Braun et al, 1997). Studies using receptor autoradiography show that these areas are rich in M1 mAChR sites (Mash et al, 1988; Cortes et al, 1986). Given the consistently demonstrated reduction of REM latency after administration of M1 AChR agonists, it may be that these limbic and paralimbic areas play an important role in the onset of REM sleep. This hypothesis seems worth further testing in preclinical studies. As a minor limitation, it is to note that RS-86 and donepezil were administered in a fixed order (block I: RS-86; block II: donepezil). However, it is plausible to assume that the resulting uncontrolled exposure to the laboratory setting did not specifically influence the main outcome parameters of REM sleep regulation. With regard to the clinic, the specification of AChR subtype function is of interest to further elucidate the presumed cholinergic alterations in various disorders that may have distinct patterns of alterations in different aspects of REM sleep, or that may be differentially affected by cholinergic agents with varying levels of specificity for AChR subtypes, such as Alzheimer's dementia and depressive disorders.
In conclusion, the present study suggests that M1 mAChRs are mediating, in part, the onset of REM sleep in healthy human subjects and that the activation of non-M1, but presumably M2 mAChRs, maintains REM sleep and evokes the occurrence of REMs.
References
Baghdoyan HA (1997). Location and quantification of muscarinic receptor subtypes in rat pons: implications for REM sleep generation. Am J Physiol 273: 896–904.
Baghdoyan HA, Lydic R (1999). M2 muscarinic receptor subtype in the feline medial pontine reticular formation modulates the amount of rapid eye movement sleep. Sleep 22: 835–847.
Baghdoyan HA, Lydic R (2002). Neurotransmitters and neuromodulators regulating sleep. In: Bazil CW et al (eds). Sleep and Epilepsy: The Clinical Spectrum. Elsevier Science: New York. pp 17–44.
Baghdoyan HA, Mallios VJ, Duckrow RB, Mash DC (1994). Localization of muscarinic receptor subtypes in brain stem areas regulating sleep. Neuroreport 5: 1631–1634.
Berkowitz A, Sutton L, Janowsky DS, Gillin JC (1990). Pilocarpine, an orally active muscarinic cholinergic agonist, induces REM sleep and reduces delta sleep in normal volunteers. Psychiatry Res 33: 113–119.
Braun AR, Balkin TJ, Wesenten NJ, Carson RE, Varga M, Baldwin P et al (1997). Regional cerebral blood flow throughout the sleep-wake cycle. An H2(15)O PET study. Brain 120: 1173–1197.
Calvo JM, Datta S, Quattrochi J, Hobson JA (1992). Cholinergic microstimulation of the peribrachial nucleus in the cat. II. Delayed and prolonged increases in REM sleep. Arch Ital Biol 130: 285–301.
Caulfield MP, Birdsall NJ (1998). International Union of Pharmacology. XVII. Classification of muscarinic acetylcholine receptors. Pharmacol Rev 50: 279–290.
Coleman CG, Lydic R, Baghdoyan HA (2004). M2 muscarinic receptors in pontine reticular formation of C57BL/6J mouse contribute to rapid eye movement sleep generation. Neuroscience 126: 821–830.
Cortes R, Probst A, Tobler HJ, Palacios JM (1986). Muscarinic cholinergic receptor subtypes in the human brain. II. Quantitative autoradiographic studies. Brain Res 362: 239–253.
Datta S, Calvo JM, Quattrochi J, Hobson JA (1992). Cholinergic microstimulation of the peribrachial nucleus in the cat. I. Immediate and prolonged increases in ponto-geniculo-occipital waves. Arch Ital Biol 130: 263–284.
Datta S, Quattrochi JJ, Hobson JA (1993). Effect of specific muscarinic M2 receptor antagonist on carbachol induced long-term REM sleep. Sleep 16: 8–14.
el Mansari M, Sakai K, Jouvet M (1989). Unitary characteristics of presumptive cholinergic tegmental neurons during the sleep–waking cycle in freely moving cats. Exp Brain Res 76: 519–529.
Gillin JC, Sutton L, Ruiz C, Golshan S, Hirsch S, Warmann C et al (1991). Dose dependent inhibition of REM sleep in normal volunteers by biperiden, a muscarinic antagonist. Biol Psychiatry 30: 151–156.
Kanbayashi T, Sugiyama T, Aizawa R, Saito Y, Ogawa Y, Kitajima T et al (2002). Effects of donepezil (Aricept) on the rapid eye movement sleep of normal subjects. Psychiatry Clin Neurosci 56: 307–308.
Lauer CJ, Modell S, Schreiber W, Krieg JC, Holsboer F (2004). Prediction of the development of a first major depressive episode with a rapid eye movement sleep induction test using the cholinergic agonist RS 86. J Clin Psychopharmacol 24: 356–357.
Leonard TO, Lydic R (1997). Pontine nitric oxide modulates acetylcholine release, rapid eye movement sleep generation, and respiratory rate. J Neurosci 17: 774–785.
Levey AI (1996). Muscarinic acetylcholine receptor expression in memory circuits: implications for treatment of Alzheimer disease. Proc Natl Acad Sci USA 93: 13541–13546.
Levey AI, Kitt CA, Simonds WF, Price DL, Brann MR (1991). Identification and localization of muscarinic acetylcholine receptor proteins in brain with subtype-specific antibodies. J Neurosci 11: 3218–3226.
Lydic R, Baghdoyan HA (1993). Pedunculopontine stimulation alters respiration and increases ACh release in the pontine reticular formation. Am J Physiol 264: 544–554.
Maquet P, Peters J, Aerts J, Delfiore G, Degueldre C, Luxen A et al (1996). Functional neuroanatomy of human rapid-eye-movement sleep and dreaming. Nature 383: 163–166.
Marks GA, Birabil CG (2000). Infusion of adenylyl cyclase inhibitor SQ22,536 into the medial pontine reticular formation of rats enhances rapid eye movement sleep. Neuroscience 98: 311–315.
Mash DC, White WF, Mesulam MM (1988). Distribution of muscarinic receptor subtypes within architectonic subregions of the primate cerebral cortex. J Comp Neurol 278: 265–274.
Nofzinger EA, Mintun MA, Wiseman M, Kupfer DJ, Moore RY (1997). Forebrain activation in REM sleep: an FDG PET study. Brain Res 770: 192–201.
Palacios JM, Bolliger G, Closse A, Enz A, Gmelin G, Malanowski J (1986). The pharmacological assessment of RS 86 (2-ethyl-8-methyl-2,8-diazaspiro-[4,5]-decan-1,3-dion hydrobromide). A potent, specific muscarinic acetylcholine receptor agonist. Eur J Pharmacol 125: 45–62.
Pare D, Curro DR, Datta S, Steriade M (1990). Brainstem genesis of reserpine-induced ponto-geniculo-occipital waves: an electrophysiological and morphological investigation. Exp Brain Res 81: 533–544.
Perlis ML, Smith MT, Orff HJ, Andrews PJ, Gillin JC, Giles DE (2002). The effects of an orally administered cholinergic agonist on REM sleep in major depression. Biol Psychiatry 51: 457–462.
Quattrochi JJ, Hobson JA (1999). Carbachol microinjection into the caudal peribrachial area induces long-term enhancement of PGO wave activity but not REM sleep. J Sleep Res 8: 281–290.
Rechtschaffen A, Kales A (1968). A Manual of Standardized Terminology, Techniques and Scoring System for Sleep Stages of Human Subjects. US Department of Health Education and Welfare: Bethesda.
Riemann D, Gann H, Dressing H, Muller WE, Aldenhoff JB (1994). Influence of the cholinesterase inhibitor galanthamine hydrobromide on normal sleep. Psychiatry Res 51: 253–267.
Riemann D, Joy D, Hochli D, Lauer C, Zulley J, Berger M (1988). Influence of the cholinergic agonist RS 86 on normal sleep: sex and age effects. Psychiatry Res 24: 137–147.
Riemann D, Lis S, Fritsch-Montero R, Meier T, Krieger S, Hohagen F et al (1996). Effect of tetrahydroaminoacridine on sleep in healthy subjects. Biol Psychiatry 39: 796–802.
Rupniak NM, Tye SJ, Iversen SD (1992). Comparison of the effects of selective and nonselective muscarinic agonists on cognition and thermoregulation in primates. J Neurol Sci 110: 222–227.
Sagales T, Erill S, Domino EF (1969). Differential effects of scopolamine and chlorpromazine on REM and NREM sleep in normal male subjects. Clin Pharmacol Ther 10: 522–529.
Sakai K, Onoe H (1997). Critical role for M3 muscarinic receptors in paradoxical sleep generation in the cat. Eur J Neurosci 9: 415–423.
Schredl M, Weber B, Leins ML, Heuser I (2001). Donepezil-induced REM sleep augmentation enhances memory performance in elderly, healthy persons. Exp Gerontol 36: 353–361.
Shuman SL, Capece ML, Baghdoyan HA, Lydic R (1995). Pertussis toxin-sensitive G proteins mediate carbachol-induced REM sleep and respiratory depression. Am J Physiol 269: 308–317.
Sitaram N, Wyatt RJ, Dawson S, Gillin JC (1976). REM sleep induction by physostigmine infusion during sleep. Science 191: 1281–1283.
Spiegel R (1984). Effects of RS 86, an orally active cholinergic agonist, on sleep in man. Psychiatry Res 11: 1–13.
Velazquez-Moctezuma J, Shalauta M, Gillin JC, Shiromani PJ (1991). Cholinergic antagonists and REM sleep generation. Brain Res 543: 175–179.
Wanibuchi F, Konishi T, Harada M, Terai M, Hidaka K, Tamura T et al (1990). Pharmacological studies on novel muscarinic agonists, 1-oxa-8-azaspiro[4.5]decane derivatives, YM796 and YM954. Eur J Pharmacol 187: 479–486.
Acknowledgements
This research was not industry supported. All authors declare no competing interests, financial or otherwise, that might have biased their work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nissen, C., Nofzinger, E., Feige, B. et al. Differential Effects of the Muscarinic M1 Receptor Agonist RS-86 and the Acetylcholine-Esterase Inhibitor Donepezil on REM Sleep Regulation in Healthy Volunteers. Neuropsychopharmacol 31, 1294–1300 (2006). https://doi.org/10.1038/sj.npp.1300906
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.npp.1300906
Keywords
This article is cited by
-
Modulation of arousal and sleep/wake architecture by M1 PAM VU0453595 across young and aged rodents and nonhuman primates
Neuropsychopharmacology (2020)
-
No effect of α‑GPC on lucid dream induction or dream content
Somnologie (2017)
-
Altered Sigma-1 Receptor Expression in Two Animal Models of Cognitive Impairment
Molecular Imaging and Biology (2015)
-
Rapid eye movements during sleep in mice: High trait-like stability qualifies rapid eye movement density for characterization of phenotypic variation in sleep patterns of rodents
BMC Neuroscience (2011)