Abstract
Alterations in plasma leptin have been reported in schizophrenia patients treated with antipsychotics, suggesting the hypothesis that impairments in leptin secretion or signaling might play a role in antipsychotic-induced weight gain. Plasma leptin was measured in 72 schizophrenia patients chronically treated with olanzapine (n=27), risperidone (n=24) or typical antipsychotics (n=21) and 124 healthy adult control subjects. ANCOVA was used to test effects of adiposity (body mass index kg/m2; BMI), subject group (treated patients vs untreated controls), and treatment group (specific medication groups and untreated controls) on plasma leptin concentrations. Additional analyses were performed in a subset of patients and controls individually matched for BMI to further assess group differences in plasma leptin independent of adiposity. BMI strongly predicted plasma leptin concentrations in the overall sample. In addition, a significant three-way interaction between BMI, subject group, and gender was observed. In the individually BMI-matched sample, modestly reduced plasma leptin levels (effect size 0.4 SD) were observed in treated patients in comparison to the BMI-matched healthy controls, with both groups including males and females. However, no differences in plasma leptin levels were observed in the matched sample when separately comparing male patients vs untreated male controls and female patients vs untreated female controls. Plasma leptin in chronically treated patients with schizophrenia is strongly predicted by adiposity, similar to untreated healthy individuals despite adequate power to detect a difference. The results argue against a role for defective leptin secretion or sensitivity in the weight gain induced by antipsychotic medications.
Similar content being viewed by others
INTRODUCTION
Leptin, the protein encoded by the ob gene, plays a major role in the regulation of appetite, adiposity and body weight. Leptin is primarily secreted by adipocytes, (Hamilton et al, 1995) with additional contributions from tissues including brain and stomach (Sobhani et al, 2002; Eikelis et al, 2004). However, the majority of plasma leptin is secreted from adipose tissue, with plasma leptin strongly and positively correlated with total-body adiposity (Klein et al, 1996). Other factors regulating leptin levels in rodents include insulin, β-adrenergic agonists, glucocorticoids and gender (Margetic et al, 2002). Leptin receptors are expressed in hypothalamic neurons in the arcuate nucleus that are associated with the regulation of energy intake (Baskin et al, 1999). Administration of leptin into the arcuate nucleus results in decreased food consumption (Campfield et al, 1995), while leptin deficiency (eg, the ob/ob mouse) leads to increased food intake (Zhang et al, 1994), suggesting a key role for leptin in the regulation of adiposity (Schwartz et al, 2000). Rare cases of leptin deficiency have produced obesity in humans (Montague et al, 1997a), but more commonly human obesity has been described as a state of leptin resistance (Schwartz et al, 2000). In this model, obesity is associated with elevated plasma leptin levels, but leptin actions on food intake are insufficiently expressed. This may be due to possible impairments in leptin transport into the arcuate nucleus or impairments in leptin signal transduction (Schwartz et al, 2000).
Obesity is occurring at epidemic rates in the US population (Mokdad et al, 2003), with overweight and obesity identified as major risk factors for the development of type 2 diabetes mellitus and cardiovascular disease (Klein et al, 2002). Increased adiposity, especially visceral abdominal adiposity, is associated with insulin resistance, elevated plasma glucose and lipid levels, and a systemic inflammatory state (Montague and O'Rahilly, 2000; Tracy, 2001). All of these conditions may contribute to the elevated cardiovascular mortality associated with obesity. Patients with mental illnesses such as schizophrenia are observed to have higher rates of obesity in comparison to the general population, related in part to treatment with psychoactive medications (Allison and Casey, 2001). Potentially related to increased adiposity as well as to other risk factors, schizophrenia patients also suffer from increased rates of cardiovascular mortality (Mortensen and Juel, 1993; Osby et al, 2000; Casey et al, 2004).
Treatment with antipsychotic medications can induce significant weight gain and related morbidity and mortality (Casey et al, 2004; Allison et al, 1999). The weight gain liability of individual first-generation (ie, typical) and second-generation (ie, atypical) antipsychotics varies substantially (Allison and Casey, 2001). The mechanisms by which treatment with antipsychotic medications contribute to weight gain and cardiovascular risk may include increased appetite and food intake (Casey and Zorn, 2001). In this context, investigators have become interested in the role of leptin in regulating appetite and adiposity during treatment with antipsychotics. Recent reports have suggested that increases in plasma leptin could be related to weight gain during antipsychotic treatment (Kraus et al, 1999; Melkersson et al, 2000; Hagg et al, 2001; Bromel et al, 1998). However, most studies have not controlled for adiposity, and increased adiposity is a major stimulus for increases in leptin secretion (Baptista and Beaulieu, 2002). Kraus et al (2001) reported lower plasma leptin levels in schizophrenia patients compared to adiposity-matched healthy controls, using the indirect adiposity measure of body mass index (BMI), arguing against leptin resistance and instead for the possibility of a decrease in leptin secretion or increased leptin clearance in this patient population. In contrast, Herran et al (2001) recently reported no difference in plasma leptin levels between treated schizophrenia patients and age, gender, and BMI-matched healthy controls. Recently, Zhang et al (2004) described increases in leptin levels after antipsychotic associated weight gain, but the study was not designed to assess if the observed increases in leptin secretion were appropriate for the amount of adiposity gained during treatment. Potential explanations for the discrepancies between these studies include the lack of statistical or experimental controls for potentially confounding variables such as gender and adiposity in some studies. For example, gender has been shown to be an important predictor of adiposity, with women having a higher percentage of body fat than men, but the effects of gender on adiposity and leptin secretion have not been well described in schizophrenia patients (Gallagher et al, 1996). The present study was motivated by recent interest in the possible role of abnormal leptin signaling as a contributor to antipsychotic-induced weight gain. This study was designed to test the a priori hypothesis that schizophrenia patients treated with different antipsychotic agents and untreated healthy controls would express the relationship between adiposity and plasma leptin concentration, either in the direction of hyposecretion of this satiety signal, or in the direction of hypersecretion suggestive of leptin resistance.
PATIENTS AND METHODS
Subjects
In all, 72 patients with schizophrenia receiving treatment with olanzapine (n=27), risperidone (n=24) or typical antipsychotics (n=21) and 124 healthy adult control subjects participated after giving written informed consent (Table 1). Subjects included individuals who had participated in previously reported studies of cognition and glucose metabolism (Fucetola et al, 1999; Newcomer et al, 1999). All the relevant studies involved both treated patients with schizophrenia and healthy untreated controls, with samples pooled simply to increase sample size for both groups. In addition, the original inclusion/exclusion criteria for all the studies were essentially identical, and recruitment was performed in the same settings by the same staff. Studies were approved by the Institutional Review Boards for Washington University School of Medicine (WUSM) and the Missouri Department of Mental Health. Patients with schizophrenia were recruited through outpatient clinics associated with WUSM, and studied on stable doses of clinically assigned antipsychotics, with treatment duration greater than 3 months (19 subjects ⩾2 years, 28 ⩾18 months, 43⩾1 year, 54⩾6 months). Healthy control subjects were recruited through advertising. Treatment groups were matched for age (F[3,192]=2.09, p=0.103) and balanced for ethnicity. A subset of subjects was created by individual subject matching based on BMI, producing a group of 49 untreated controls and 49 treated patients (olanzapine n=17, typicals n=16, risperidone n=16), with a mean BMI difference ±SD between individual patients and controls of 0.07±0.09 kg/m2 (Table 2).
All subjects received a medical screening and diagnostic evaluation, including the Diagnostic Interview for Genetic Studies (Nurnberger et al, 1994) (DIGS) and a review of available medical records, with a final research diagnosis made by a research psychiatrist using Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (American Psychiatric Association, 1994) algorithms. Subjects were excluded for (i) Axis I disorders except schizophrenia, and substance abuse and/or dependence occurring less than 6 months prior to study entry; (ii) medical conditions which could confound metabolic assessments, including history of diabetes mellitus, recognized cardiovascular and respiratory conditions with hemodynamic compromise or hypoxia, malignancy, epilepsy, endocrine disease (excluding corrected thyroid abnormalities), current fever, dehydration, nausea, body weight <80% of ideal, pregnancy or high-dose estrogen therapy, narcotic, corticosteroid or spironolactone therapy, sedative hypnotic withdrawal, or any changes in medications within 10 days of study. Similarly, no subjects were included for analysis who were treated with glucose or lipid-lowering medications. All subjects had baseline fasting and postglucose load glucose determinations, and 57 of the 72 schizophrenia subjects had glycated hemoglobin measurements. In order to exclude subjects with probable diabetes mellitus, subjects were excluded for fasting plasma glucose ⩾126 mg/dl (7 mmol/l), (The Expert Committee on the Diagnosis and Classification of Diabetes Mellitus, 2003) or for postglucose (eg, two values ⩾200 mg/dl [11.1 mmol/l]) and glycated hemoglobin values strongly suggestive of diabetes mellitus (ie, >6.1%) (World Health Organization, 1985; Davidson et al, 1999). All patients were additionally characterized using the Brief Psychiatric Rating Scale (Overall, 1974) (BPRS; 18-item, 1–7 scale).
Baseline clinical data as well as mean doses of the primary antipsychotic treatments for each patient group are listed in Table 1. Of the 72 patients, 21 were receiving typical antipsychotic therapy. Of these 21 subjects, seven were receiving oral agents only (two haloperidol, two trifluperazine, two thiothixene, one perphenazine), one was receiving oral agents in combination with depot preparations (fluphenazine decanoate 25 mg/4 weeks plus oral fluphenazine 5 mg/day), and 10 subjects were receiving haloperidol decanoate as their only antipsychotic treatment (mean mg/4 weeks ±SD=222.6±178.8). Three subjects were receiving fluphenazine decanoate as their only antipsychotic treatment (mean mg/2 weeks ±SD =50.0±43.30). Mean antipsychotic dose for typical oral agents (n=21; haloperidol equivalents) is listed in Table 1. In all, 11 of the 21 subjects on typical agents were receiving anticholinergics (seven benztropine mesylate mean daily mg±SD=2.7±1.25, four trihexyphenidyl mean daily mg±SD=5.5±3.42). Two of the 21 were receiving antidepressants (one sertraline 50 mg/day plus buspirone 10 mg/day, one amitriptyline 10 mg/day), and two were receiving benzodiazepines (one temazepam 30 mg/day, one clonazepam 1 mg/day).
Of the 72 patients, 27 were receiving olanzapine (Table 1). Of these, six were receiving anticholinergics (benztropine mesylate mean daily mg±SD=1.6±0.7), four were receiving antidepressants, (one doxepin 75 mg/day, one bupropion 400 mg/day, one nefazodone 600 mg/day, one citalopram 20 mg/day), two were receiving clonazepam (mean daily mg±SD=2±1.4), four were receiving lorazepam (mean daily mg=1.1±0.6), two were receiving divalproex (mean daily mg±SD=1000±707), one was receiving gabapentin (1800 mg/day), and one was receiving lamotrigine (450 mg/day). In addition, five subjects were also receiving adjunctive haloperidol (three decanoate mean mg/4 weeks ±SD=108.33±38.19, two hydrochloride mean daily mg±SD 15±7.1). One subject was receiving adjunctive fluphenazine decanoate (50 mg/2 weeks).
Of 72 patients, 24 were receiving risperidone (Table 1). Of those 24, seven were receiving anticholinergics (six benztropine mesylate mean daily mg±SD=1.8±1.26, 1-trihexyphenidyl 4 mg/day), six were receiving antidepressants (one clomipramine 75 mg/day, one fluoxetine 20 mg/day, two paroxetine 30 mg/day, two bupropion 300 mg/day), three were receiving lorazepam (mean daily mg±SD= 1.2±0.6), two were receiving divalproex (mean daily mg±SD=1000±707), and one was receiving lithium (600 mg/day). In addition, two subjects were receiving adjunctive haloperidol decanoate (mean mg/4 weeks ±SD=216.7±165.0). One subject was receiving adjunctive fluphenazine decanoate (25 mg/4 weeks), while one subject received adjunctive oral fluphenazine (20 mg/day).
Procedure
Study protocols were approved and conducted through the General Clinical Research Center (GCRC) at WUSM. Plasma leptin concentration was determined by radioimmunoassay (Linco Research, St Louis, MO) using purified recombinant human leptin as standard and radiolabel and a rabbit polyclonal antibody to human leptin, with a second antibody separation method. The assay limits of detection and linearity were 0.5 and 100 ng/ml in plasma (Ma et al, 1996), with leptin values >100 ng/ml reassayed on dilution. Intra- and inter-assay coefficients of variation were <7%, with no cross-reactivity with common peptide hormones.
Data Analysis
Initial analyses included all subjects. Analysis of covariance (ANCOVA) was used to test the primary study hypothesis that adiposity as well as subject group (treated patients vs untreated controls) and/or treatment group (specific medication groups and untreated controls) would predict plasma leptin levels. For the main models, ANCOVAs were constructed with leptin as the dependent variable and subject group or treatment group and the covariate of BMI as independent variables. The overall significance level was set at p=0.05 for tests of the main hypothesis, with two-tailed tests of significance in all relevant analyses.
As an additional precaution against confounds to the interpretation of the results, gender, cortisol, fasting insulin, fasting glucose, smoking status, and age were individually added as either potentially confounding covariate terms or factors to the main model. Data were analyzed using StatView/SuperAnova (SAS Institute Inc., Cary, NC).
RESULTS
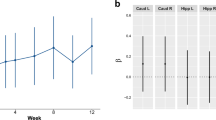
Plasma leptin levels were strongly predicted by BMI in the overall sample, as well as in all subject and treatment groups, with increasing adiposity associated with increasing plasma leptin. The effect of BMI on plasma leptin modestly varied in magnitude depending on treatment and/or disease condition. ANCOVA models in the overall sample, using plasma leptin as the dependent variable, BMI as the covariate term, and independent factors of either treatment group (risperidone, olanzapine, typicals, or untreated healthy controls) or subject group (treated patients or untreated controls) were performed. A robust main effect of BMI (F[1,194]=97.20, p<0.0001) was observed, with only limited interactions between BMI and both treatment group (F[3,188]=3.54, p=0.016) and subject group (F[1,192]=3.65, p=0.058, Figure 1). No additional significant main effects or interactions were detected when cortisol, fasting insulin, fasting glucose, smoking status, age or ethnicity were added to either the BMI × subject group or BMI × treatment group models in the overall sample. However, a significant three-way interaction between BMI, subject group, and gender was observed (F[1,188]=18.19, p<0.0001).
Using subject groups that are not matched for adiposity, potential group differences in plasma leptin are difficult to interpret. Therefore, individual treated subjects were closely BMI-matched on a 1 : 1 basis with untreated healthy controls, as described in the Patients and Methods, for all subsequent analyses. Controlling in this manner for the effects of adiposity, subject group (F[1,96]=4.57, p=0.035) but not treatment group (F[3,94]=2.09, p=0.107) modestly predicted plasma leptin concentrations, with treated patients apparently having slightly lower (∼0.4 SD) plasma levels in comparison to untreated healthy control subjects. No interactions with BMI and treatment group or subject group were detected.
In order to further pursue the question of why treated patients might have lower plasma leptin levels, other variables that regulate plasma leptin were considered. The three-way interaction between BMI, gender, and subject group that was present in the overall sample was also present in the BMI matched sample (F[1,90]=5.15, p=0.026). In order to decompose this three-way interaction, we examined patients and controls separately, and males and females separately (Figure 2). There was a significant BMI × sex interaction for leptin in controls but not patients. Also, there was a nonsignificant, trend-level interaction between BMI and subject group in females but not males. In these analyses, no main effect of subject group was detected, suggesting similar plasma leptin levels in male patients vs controls (F[1,60]=0.001, p=0.978) and female patients vs controls (F[1,34]=0.007, p=0.936) (Figure 3).
DISCUSSION
In contrast to previous reports, the results of this study indicate that adiposity-related elevations in plasma leptin concentrations in antipsychotic-treated patients with schizophrenia are highly comparable to those observed in untreated healthy control subjects. Carefully controlling for the effects of adiposity, gender and other potential confounds in a well-powered study, no evidence of differences in plasma leptin concentration were detected comparing antipsychotic-treated patients to untreated controls. The results of this study argue against the hypothesis that antipsychotic treatment or schizophrenia is associated with defects in leptin secretion, clearance or signaling as compared to untreated, otherwise healthy humans. While slightly lower plasma leptin levels were observed in BMI-matched treated patients in comparison to untreated healthy controls, this difference was not present when this comparison was made within males and females separately. Differences between males and females are likely due to gender-related differences in fat mass at any given level of BMI. This result underscores the need for direct measures of adiposity in future studies and may account for some of the discrepant results previously reported in the literature. With respect to leptin secretion, adiposity plays same physiologic role in schizophrenia patients as in the general population. Therefore, these results are relevant in predicting whether increases in adiposity in schizophrenia patients are associated with related impairments in glucose and lipid metabolism, and ultimately cardiovascular risk.
This study measured plasma leptin levels, which are thought to participate in CNS-mediated feedback control of satiety. However, pathways involved in the regulation of appetite, satiety, and leptin signaling are regulated by other neurotransmitter systems of interest to psychiatrists, including the histaminergic, serotonergic, and adrenergic systems (Morimoto et al, 2001; Del Rio, 2000; Heisler et al, 2002). In addition, there appears to be significant redundancy and buffering of complex homeostatic mechanisms involving multiple orexigenic and anorexigenic signals. Given antipsychotic medication interactions with relevant monoamine receptors, and with other signals (Fadel et al, 2002), it might be expected that antipsychotic medications can induce different degrees of weight gain with leptin serving a common counter-regulatory role.
This study was not designed to measure peripheral leptin effects. While leptin is considered a major CNS satiety signal, leptin may also play an important role in the peripheral control of deposition of unutilized dietary fat into adipose tissue (Unger, 2003b). The regulation of dietary fat deposition into adipose tissue may serve to protect nonadipose tissue such as skeletal muscle, heart, liver, and pancreas from lipotoxicity (cellular damage associated with deposition of fatty acids) (Unger, 2003a). The accumulation of fatty acids in nonadipose tissue has been linked to the metabolic syndrome, a prevalent but underdiagnosed condition in the US associated with cardiac morbidity and mortality (Ford et al, 2002). These peripheral effects of leptin have not been examined in schizophrenia patients, and may represent yet another hypothetical mechanism which could contribute to the high rates of cardiovascular mortality seen in schizophrenia. It should be noted that in addition to leptin, there are many other known and proposed satiety signals (Schwartz et al, 2000). As such, there may be redundant mechanisms controlling satiety, and perturbations in one system may be compensated by changes in other systems. Future studies testing hypothesized changes in satiety signaling in neuropsychiatric patients may need to consider dynamic measurement of multiple satiety signals such as insulin, leptin, ghrelin, and adiponectin.(Schwartz et al, 2000; Kershaw and Flier, 2004; de Graaf et al, 2004)
This study did not collect prospective serial measurements of changes in plasma leptin during the initial phase of antipsychotic treatment, limiting the ability to rule out changes in leptin signaling that might occur early in the process of weight change. While a prospective study design focused on the initial phase of antipsychotic treatment would provide this ability, the current study design permitted careful control for adiposity, including 1 : 1 BMI matching, so that the appropriateness of leptin levels in relation to adiposity could be carefully assessed. Both types of studies can therefore provide valuable information regarding the effects of medication and disease on leptin secretion and action. Future studies that aim to evaluate the regulation of plasma leptin must control for effects of adiposity. In addition, this study used indirect measurement of adiposity, and was not able to distinguish between visceral or subcutaneous adipose tissue. Differential expression of leptin mRNA is described among regions of adipose tissue in humans, with several investigators describing reduced leptin mRNA expression in visceral adipose tissue compared to subcutaneous fat (Hube et al, 1996; Montague et al, 1997b; Van Harmelen et al, 1998). Preferential deposition of fatty acids to subcutaneous vs visceral fat stores (a common pattern in obese women) could therefore result in different degrees of elevation of leptin secretion. For example, increases in visceral fat might be associated with smaller increases in leptin levels than would be associated with increases in subcutaneous fat. Differences in leptin levels between subject groups may relate to differences in adipose tissue distribution, given possibly variable secretion of leptin in subcutaneous vs visceral adipose tissue. Investigators have just begun to describe the distribution of adipose tissue during antipsychotic treatment of schizophrenia. Thakore et al (2002) have reported increased visceral adiposity using CT scanning and anthropomorphic measurements in both treated and untreated schizophrenia patients in comparison to age- and sex-matched, but not BMI-matched healthy controls. Zhang et al (2004) reported elevated leptin levels in female patients treated with antipsychotics, consistent with the higher ratio of subcutaneous : visceral adipose tissue seen in the female patients. Use of sensitive measures could help to explain some of the inconsistencies in this literature.
In conclusions, results of this study indicate that there are no large or clinically significant differences in the relationship between plasma leptin and adiposity in treated patients with schizophrenia as compared to untreated healthy controls. Consistent with the report by Herran et al (2001), these results do not support hypotheses concerning impaired leptin secretion or leptin resistance in treated schizophrenia patients compared to healthy controls. Owing to continuing problem of increased prevalence of overweight and obesity in mental illnesses like schizophrenia, and the known impact of obesity on long-term survival, future studies of satiety signals are needed in order to improve the health of patients with mental illness.
References
Allison DB, Casey DE (2001). Antipsychotic-induced weight gain: a review of the literature. J Clin Psychiatry 62 (Suppl 7): 22–31.
Allison DB, Mentore JL, Heo M, Chandler LP, Cappelleri JC, Infante MC et al (1999). Antipsychotic-induced weight gain: a comprehensive research synthesis. Am J Psychiatry 156: 1686–1696.
American Psychiatric Association (1994). Diagnostic and Statistical Manual of Mental Disorders, 4th edn American Psychiatric Association: Washington, DC.
Baptista T, Beaulieu S (2002). Are leptin and cytokines involved in body weight gain during treatment with antipsychotic drugs? Can J Psychiatry 47: 742–749.
Baskin DG, Hahn TM, Schwartz MW (1999). Leptin sensitive neurons in the hypothalamus. Horm Metab Res 31: 345–350.
Bromel T, Blum WF, Ziegler A, Schulz E, Bender M, Fleischhaker C et al (1998). Serum leptin levels increase rapidly after initiation of clozapine therapy. Mol Psychiatry 3: 76–80.
Campfield LA, Smith FJ, Guisez Y, Devos R, Burn P (1995). Recombinant mouse OB protein: evidence for a peripheral signal linking adiposity and central neural networks. Science 269: 546–549.
Casey DE, Haupt DW, Newcomer JW, Henderson DC, Sernyak MJ, Davidson M et al (2004). Antipsychotic-induced weight gain and metabolic abnormalities: implications for increased mortality in patients with schizophrenia. J Clin Psychiatry 65: 4–18.
Casey DE, Zorn SH (2001). The pharmacology of weight gain with antipsychotics. J Clin Psychiatry 62 (Suppl 7): 4–10.
Davidson MB, Schriger DL, Peters AL, Lorber B (1999). Relationship between fasting plasma glucose and glycosylated hemoglobin: potential for false-positive diagnoses of type 2 diabetes using new diagnostic criteria. JAMA 281: 1203–1210.
de Graaf C, Blom WA, Smeets PA, Stafleu A, Hendriks HF (2004). Biomarkers of satiation and satiety. Am J Clin Nutr 79: 946–961.
Del Rio G (2000). Adrenomedullary function and its regulation in obesity. Int J Obes Relat Metab Disord 24 (Suppl 2): S89–S91.
Eikelis N, Lambert G, Wiesner G, Kaye D, Schlaich M, Morris M et al (2004). Extra-adipocyte leptin release in human obesity and its relation to sympathoadrenal function. Am J Physiol Endocrinol Metab 286: E744–E752.
Fadel J, Bubser M, Deutch AY (2002). Differential activation of orexin neurons by antipsychotic drugs associated with weight gain. J Neurosci 22: 6742–6746.
Ford ES, Giles WH, Dietz WH (2002). Prevalence of the metabolic syndrome among US adults: findings from the third National Health and Nutrition Examination Survey. JAMA 287: 356–359.
Fucetola R, Newcomer JW, Craft S, Melson AK (1999). Age- and dose-dependent glucose-induced increases in memory and attention in schizophrenia. Psychiatry Res 88: 1–13.
Gallagher D, Visser M, Sepulveda D, Pierson RN, Harris T, Heymsfield SB (1996). How useful is body mass index for comparison of body fatness across age, sex, and ethnic groups? Am J Epidemiol 143: 228–239.
Hagg S, Soderberg S, Ahren B, Olsson T, Mjorndal T (2001). Leptin concentrations are increased in subjects treated with clozapine or conventional antipsychotics. J Clin Psychiatry 62: 843–848.
Hamilton BS, Paglia D, Kwan AY, Deitel M (1995). Increased obese mRNA expression in omental fat cells from massively obese humans. Nat Med 1: 953–956.
Heisler LK, Cowley MA, Tecott LH, Fan W, Low MJ, Smart JL et al (2002). Activation of central melanocortin pathways by fenfluramine. Science 297: 609–611.
Herran A, Garcia-Unzueta MT, Amado JA, de La Maza MT, Alvarez C, Vazquez-Barquero JL (2001). Effects of long-term treatment with antipsychotics on serum leptin levels. Br J Psychiatry 179: 59–62.
Hube F, Lietz U, Igel M, Jensen PB, Tornqvist H, Joost HG et al (1996). Difference in leptin mRNA levels between omental and subcutaneous abdominal adipose tissue from obese humans. Horm Metab Res 28: 690–693.
Kershaw EE, Flier JS (2004). Adipose tissue as an endocrine organ. J Clin Endocrinol Metab 89: 2548–2556.
Klein S, Coppack SW, Mohamed-Ali V, Landt M (1996). Adipose tissue leptin production and plasma leptin kinetics in humans. Diabetes 45: 984–987.
Klein S, Wadden T, Sugerman HJ (2002). AGA technical review on obesity. Gastroenterology 123: 882–932.
Kraus T, Haack M, Schuld A, Hinze-Selch D, Kuhn M, Uhr M et al (1999). Body weight and leptin plasma levels during treatment with antipsychotic drugs. Am J Psychiatry 156: 312–314.
Kraus T, Haack M, Schuld A, Hinze-Selch D, Pollmacher T (2001). Low leptin levels but normal body mass indices in patients with depression or schizophrenia. Neuroendocrinology 73: 243–247.
Ma Z, Gingerich RL, Santiago JV, Klein S, Smith CH, Landt M (1996). Radioimmunoassay of leptin in human plasma. Clin Chem 42: 942–946.
Margetic S, Gazzola C, Pegg GG, Hill RA (2002). Leptin: a review of its peripheral actions and interactions. Int J Obes Relat Metab Disord 26: 1407–1433.
Melkersson KI, Hulting AL, Brismar KE (2000). Elevated levels of insulin, leptin, and blood lipids in olanzapine-treated patients with schizophrenia or related psychoses. J Clin Psychiatry 61: 742–749.
Mokdad AH, Ford ES, Bowman BA, Dietz WH, Vinicor F, Bales VS et al (2003). Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA 289: 76–79.
Montague CT, Farooqi IS, Whitehead JP, Soos MA, Rau H, Wareham NJ et al (1997a). Congenital leptin deficiency is associated with severe early-onset obesity in humans. Nature 387: 903–908.
Montague CT, O'Rahilly S (2000). The perils of portliness: causes and consequences of visceral adiposity. Diabetes 49: 883–888.
Montague CT, Prins JB, Sanders L, Digby JE, O'Rahilly S (1997b). Depot- and sex-specific differences in human leptin mRNA expression: implications for the control of regional fat distribution. Diabetes 46: 342–347.
Morimoto T, Yamamoto Y, Yamatodani A (2001). Brain histamine and feeding behavior. Behav Brain Res 124: 145–150.
Mortensen PB, Juel K (1993). Mortality and causes of death in first admitted schizophrenic patients. Br J Psychiatry 163: 183–189.
Newcomer JW, Craft S, Fucetola R, Moldin SO, Selke G, Paras L et al (1999). Glucose-induced increase in memory performance in patients with schizophrenia. Schizophr Bull 25: 321–335.
Nurnberger JIJ, Blehar MC, Kaufmann CA, York-Cooler C, Simpson SG, Harkavy-Friedman J et al (1994). Diagnostic interview for genetic studies. Rationale, unique features, and training. NIMH Genetics Initiative. Arch Gen Psychiatry 51: 849–859; discussion 863–864.
Osby U, Correia N, Brandt L, Ekbom A, Sparen P (2000). Mortality and causes of death in schizophrenia in Stockholm county, Sweden. Schizophr Res 45: 21–28.
Overall JE (1974). A brief psychiatric rating scale in psychopharmacology research. In Pichot P (ed). Psychological Measurements in Psychopharmacology, Modern Problems in Pharmacopsychiatry, 7th edn. Karger: Basel. pp 67–78.
Schwartz MW, Woods SC, Porte DJ, Seeley RJ, Baskin DG (2000). Central nervous system control of food intake. Nature 404: 661–671.
Sobhani I, Buyse M, Goiot H, Weber N, Laigneau JP, Henin D et al (2002). Vagal stimulation rapidly increases leptin secretion in human stomach. Gastroenterology 122: 259–263.
Thakore JH, Mann JN, Vlahos I, Martin A, Reznek R (2002). Increased visceral fat distribution in drug-naive and drug-free patients with schizophrenia. Int J Obes Relat Metab Disord 26: 137–141.
The Expert Committee on the Diagnosis and Classification of Diabetes Mellitus (2003). Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care 26 (Suppl 1): S5–S20.
Tracy RP (2001). Is visceral adiposity the ‘enemy within’? Arterioscler Thromb Vasc Biol 21: 881–883.
Unger RH (2003a). Minireview: weapons of lean body mass destruction: the role of ectopic lipids in the metabolic syndrome. Endocrinology 144: 5159–5165.
Unger RH (2003b). The physiology of cellular liporegulation. Annu Rev Physiol 65: 333–347.
Van Harmelen V, Reynisdottir S, Eriksson P, Thorne A, Hoffstedt J, Lonnqvist F et al (1998). Leptin secretion from subcutaneous and visceral adipose tissue in women. Diabetes 47: 913–917.
World Health Organization (1985). Diabetes Mellitus: Report of a WHO Study Group. World Health Organization:Geneva.
Zhang Y, Proenca R, Maffei M, Barone M, Leopold L, Friedman JM (1994). Positional cloning of the mouse obese gene and its human homologue. Nature 372: 425–432.
Zhang ZJ, Yao ZJ, Liu W, Fang Q, Reynolds GP (2004). Effects of antipsychotics on fat deposition and changes in leptin and insulin levels. Magnetic resonance imaging study of previously untreated people with schizophrenia. Br J Psychiatry 184: 58–62.
Acknowledgements
This study was funded by K23 MH067795, MH63985, Washington University General Clinical Research Center USPHS MO1 RR00036, and Washington University Clinical Nutrition Research Unit Center Grant P30 DK56341.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Haupt, D., Luber, A., Maeda, J. et al. Plasma Leptin and Adiposity During Antipsychotic Treatment of Schizophrenia. Neuropsychopharmacol 30, 184–191 (2005). https://doi.org/10.1038/sj.npp.1300563
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.npp.1300563
Keywords
This article is cited by
-
Chronic treatment with olanzapine increases adiposity by changing fuel substrate and causes desensitization of the acute metabolic side effects
Naunyn-Schmiedeberg's Archives of Pharmacology (2014)
-
Olanzapine promotes fat accumulation in male rats by decreasing physical activity, repartitioning energy and increasing adipose tissue lipogenesis while impairing lipolysis
Molecular Psychiatry (2011)
-
Nestin in Human Skin: Exclusive Expression in Intramesenchymal Skin Compartments and Regulation by Leptin
Journal of Investigative Dermatology (2009)
-
Atypische Neuroleptika und metabolisches Syndrom
Wiener Medizinische Wochenschrift (2007)
-
The impact of hyperactivity and leptin on recovery from anorexia nervosa
Journal of Neural Transmission (2007)