Abstract
Elevated basal intracellular calcium (Ca2+) levels ([Ca2+]B) in B lymphoblast cell lines (BLCLs) from bipolar I disorder (BD-I) patients implicate altered Ca2+ homeostasis in this illness. Chronic lithium treatment affects key proteins modulating intracellular Ca2+ signaling. Thus, we sought to determine if chronic exposure to therapeutic lithium concentrations also modifies intracellular Ca2+ homeostasis in this surrogate cellular model of signal transduction disturbances in BD. BLCLs from BD-I (N=26) and healthy subjects (N=17) were regrown from frozen stock and incubated with 0.75 mM lithium or vehicle for 24 h (acute) or 7 days (chronic). [Ca2+]B, lysophosphatidic acid (LPA)-stimulated Ca2+ mobilization ([Ca2+]S), and thapsigargin-induced store-operated Ca2+ entry (SOCE) were determined using ratiometric fluorometry with Fura-2. Compared with vehicle, chronic lithium exposure resulted in significantly higher [Ca2+]B (F=8.47; p=0.006) in BLCLs from BD-I and healthy subjects. However, peak LPA-stimulated [Ca2+]S and SOCE were significantly reduced (F=11.1, p=0.002 and F=8.36, p=0.007, respectively). Acute lithium exposure did not significantly affect measured parameters. In summary, the effect of chronic lithium to elevate [Ca2+]B in BLCLs while attenuating both receptor-stimulated and SOCE components of intracellular Ca2+ mobilization in BLCLs suggests that modulation of intracellular Ca2+ homeostasis may be important to the therapeutic action of lithium.
Similar content being viewed by others
INTRODUCTION
Lithium has been used in the management of bipolar disorder (BD) for over 50 years (Goodwin and Jamison, 1990), and despite its proven efficacy (Schou, 2001), the specific mechanism(s) by which it exerts its therapeutic effects in BD is still poorly understood (reviewed in Lenox et al, 1998; Manji et al, 2001). As the latency in onset of lithium's clinical action implicated plastic changes mediated through intracellular signaling processes, transcription regulation, and accompanying alterations in abundance and function of target proteins, intracellular signal transduction systems have come under closer scrutiny in search of the molecular basis of its therapeutic action in BD (Manji et al, 2001). Among these, the Ca2+ signaling system is of particular interest given its critical role in numerous cellular functions (for reviews see Ghosh and Greenberg, 1995; Berridge et al, 2000 and references therein).
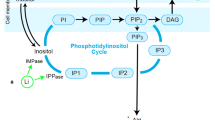
Intracellular Ca2+ signaling and homeostasis are maintained by an intricate array of processes acting in concert (Berridge et al, 2000; Putney et al, 2001) including, for example, inositol trisphosphate (IP3)- and ryanodine-stimulated release of Ca2+ from endoplasmic reticulum (ER) storage pools (Berridge, 1995; Barritt, 1999; Putney and Ribeiro, 2000), voltage- and ligand-gated ion channel mediated Ca2+ influx (Ghosh and Greenberg, 1995), store-operated Ca2+ entry (SOCE) (Putney et al, 2001), plasma membrane and sarcoplasmic/ER Ca2+-ATPase pumps (PMCAs and SERCAs) (Brini and Carafoli, 2000), and mitochondrial Ca2+ uptake, storage, and release (Brini and Carafoli, 2000; Fall and Keizer, 2001). Disturbances of intracellular Ca2+ signaling can critically affect cellular function due to calcium's essential role in vital cellular processes including gene expression (Ghosh and Greenberg, 1995), neurogenesis and plasticity (Mattson, 2000), and cell death (Szalai et al, 1999). It is of some interest then that lithium acts on several second messenger systems and intracellular signal transducing proteins (Manji et al, 1999; Williams and Harwood, 2000) that are involved in key cellular functions that affect neurogenesis, neuroplasticity, and cell death (Manji et al, 2000).
The notion that intracellular Ca2+ dynamics may be altered in BD has been suggested by studies using peripheral blood cells as surrogate models, as well as investigations on post-mortem brain. Elevated basal ([Ca2+]B) and agonist-stimulated ([Ca2+]S) intracellular Ca2+ levels in the platelets and lymphocytes of bipolar I disorder (BD-I) patients compared with healthy subjects (Dubovsky et al, 1989, 1992; Tan et al, 1990; Plenge et al, 1994; Berk et al, 1995; Emamghoreishi et al, 1997; Hough et al, 1999) are among the most widely replicated findings in psychobiological studies of BD. Several observations suggest that these abnormalities reflect intrinsic disturbances in cellular function. First, plasma ultrafiltrates from BD patients did not affect [Ca2+]B in platelets from healthy subjects (Dubovsky et al, 1994). More important, elevated [Ca2+]B (Emamghoreishi et al, 1997) and agonist-stimulated [Ca2+]S (Wasserman et al, 2003) have been reported in B lymphoblast cell lines (BLCLs) from BD patients. Finally, these abnormalities have been observed independent of state of illness (Tan et al, 1990; Kusumi et al, 1994; Emamghoreishi et al, 1997).
Post-mortem brain studies have also revealed changes that may reflect possible ‘signatures’ of abnormal Ca2+ homeostasis in BD. These include a marked blunting of G-protein activated phosphoinositide (PI) hydrolysis (Jope et al, 1996) and altered mRNA expression levels of two candidate proteins, which may have important roles in Ca2+ homeostasis, inositol monophosphatase (IMPase) type II (Yoon et al, 2001a), and a transient receptor potential channel, TRPM2 (TRPC7 in earlier nomenclature) (Yoon et al, 2001b), a ligand-gated plasma membrane ion channel which also mediates Ca2+ entry into cells.
Substantial evidence also links lithium treatment to the modulation of intracellular Ca2+ homeostasis. Lithium attenuates agonist-stimulated intracellular Ca2+ responses in a number of cellular paradigms, including astrocytes (Helman et al, 1986), C6 rat glioma cells (Yamaji et al, 1997), rat cerebellar granule cells (Nonaka et al, 1998), GH3 pituitary cells (Varney et al, 1992), rat hippocampal slices (Okamoto et al, 1995), human neutrophils (Forstner et al, 1994), and platelets (Dubovsky et al, 1991). As well, lithium inhibits IMPase uncompetitively (Hallcher and Sherman, 1980), an effect suggested to diminish overactive signaling through PI-linked second messengers and, in turn, Ca2+ (Berridge et al, 1982).
Current understanding of the molecular actions of lithium and other mood stabilizers has been gleaned almost entirely from preclinical work using tissue and cellular models of nonhuman origin, which do not express the disease phenotype. BLCLs from BD patients appear to stably express underlying abnormalities in Ca2+ homeostasis that may be more intimately linked to the pathophysiology of this disorder (Emamghoreishi et al, 1997; Yoon et al, 2001a, 2001b; Wasserman et al, 2003). As such, they afford a particularly pertinent species and disease relevant model in which to explore the mechanisms by which lithium modifies these intracellular Ca2+ disturbances and the relevance of such effects to its therapeutic action. Accordingly, in this study we have exploited this model to determine whether lithium, at a therapeutically relevant concentration, modulates intracellular Ca2+ homeostasis abnormalities identified in BLCLs from BD-I patients, and whether this effect requires chronic exposure. Towards this end, two key components of intracellular Ca2+ mobilization were scrutinized: (1) receptor-G-protein coupled agonist (lysophosphatidic acid (LPA)) stimulation of Ca2+ mobilization through the PI/IP3 signaling pathway, and (2) SOCE. We report here that chronic (7 days), but not acute (24 h), treatment of BLCLs from both BD-I patients and healthy subjects with lithium, at a therapeutically relevant concentration, significantly elevated [Ca2+]B and attenuated LPA-stimulated Ca2+ mobilization and SOCE. These results suggest that the modulation of intracellular Ca2+ homeostasis may be important to the therapeutic action of lithium.
MATERIALS AND METHODS
Subjects
BD-1 patients and healthy subjects were recruited and assessed as previously described (Emamghoreishi et al, 1997). Confirmation of diagnoses was performed using the Structured Clinical Interview for DSM-IV Axis I Disorders—Patient Edition (SCID-I/P) (First et al, 1995b) or Nonpatient Edition (SCID-I/NP) (First et al, 1995a) administered by a research psychiatrist or a trained psychiatric assistant. Subjects had no concurrent medical illness, diabetes or hypertension, no recent (>3 months) drug or alcohol abuse (BD-I patients), and were competent to provide informed written consent. Healthy subjects had no family history of psychiatric disorders in first-degree relatives. All subjects were screened with a systems review and a physical examination, where necessary, to rule out the presence of any chronic physical illness. The study was approved by the Human Subjects Review Board of the University of Toronto.
Cell Culture Materials, Reagents, and Drugs
Characterized fetal bovine serum (FBS) was from HyClone (Logan, UT). RPMI-1640, L-glutamine and trypan blue were obtained from Invitrogen Life Technologies (Burlington, ON). Penicillin (10 000 U/ml), streptomycin (10 mg/ml), pyruvate, dimethylsulfoxide (DMSO), MgCl2, 4-(2-hydroxyethyl)-1-piperazineethanesulfonic acid (HEPES), LPA (1-oleoyl-sn-glycero-3-phosphate), and ethylene glycol bis(2-aminoethyl ether)-N,N,N′N′-tetra-acetic acid (EGTA) were from Sigma (Oakville, ON). NaCl, KCl, CaCl2, and D-glucose were of analytical grade. Polyethylene glycol-8000 was from Mallinckrodt (Point-Claire, QC). Triton X-100 and lithium chloride (LiCl) were from JT Baker (Phillipsburgh, NJ). Thapsigargin (TG) was obtained from Calbiochem (La Jolla, CA) and Fura-2 acetoxymethyl ester (Fura-2 AM) from Molecular Probes (Eugene, OR).
Establishment of BLCLs
Epstein–Barr virus (EBV) transformed BLCLs were established using standard techniques (Emamghoreishi et al, 1997). The BLCLs for this study were selected from frozen stocks established from a cohort of BD-I patients and healthy comparison subjects participating in ongoing studies of signal transduction mechanisms in mood disorders in this laboratory (Emamghoreishi et al, 1997; Yoon et al, 2001a, 2001b). BLCLs were initially expanded in culture for 13–16 passages in a 95% air/5% CO2 humidified incubator at 37°C (2–3 days/passage) prior to freezing and storage in the vapor phase of liquid nitrogen.
BLCL Regrowth Conditions
BLCLs from BD patients and healthy controls were regrown in paired groups from subjects matched on the basis of age and sex. Cells were cultured for 6–10 passages (4–7 weeks) prior to initiating treatment with LiCl or vehicle. During regrowth, B cell media (BCM: RPMI 1640, 20% FBS, 2 mM L-glutamine, 1 mM pyruvate, 100 μg/ml streptomycin, 100 U/ml penicillin) was replenished every 2 days. Cell counts, and viability, as determined by trypan blue exclusion (Emamghoreishi et al, 1997), were estimated at each feeding.
Drug Treatment Protocol
Once BLCLs reached the required cell counts (>9 × 107 cells, >95% viability), they were divided equally into three groups: two (A and B) were fed with aqueous control medium consisting of BCM to which isotonic NaCl vehicle solution of the same volume as the lithium solution, (10 ml/l BCM) was added, while the other (C) was treated with BCM containing LiCl (final concentration 0.75 mM). Media was completely replaced by gentle sedimentation (50 g, 10 min) and resuspension of cells every other day for the first 6 days. At day 6, cells were gently sedimented, the supernatant was removed, and the cells were resuspended in RPMI-1640 containing either vehicle solution as above (A) or 0.75 mM LiCl (B). Cells that had been treated with BCM containing LiCl (C) for the first 6 days were also washed and taken up in 0.75 mM LiCl in RPMI-1640. After a further 24 h incubation, cells were harvested and endpoint Ca2+ mobilization assays were performed.
Ca2+ Mobilization Assays
Agonist (LPA) stimulation
The assay of LPA-stimulated Ca2+ mobilization was performed as previously described (Rosskopf et al, 1998) with modifications. Briefly, cells (1–3 × 106/ml in RPMI-1640) were loaded with Fura-2-AM (1 μM) or treated with an equivalent volume of DMSO (1 μl/ml cell suspension; blank sample) as previously described (Emamghoreishi et al, 1997). Following loading, cells were placed on ice until spectrophotofluorometric quantitation to reduce compartmentalization and dye leakage. Immediately prior to analysis, cells were transferred to a spectrophotofluorometric cuvette and allowed to equilibrate in the temperature-controlled chamber of a Perkin-Elmer L50B fluorometer, with gentle stirring for 3 min at 37°C. Free- and Ca2+-bound Fura-2 fluorescence intensities (excitation 340/380 nm, emission 500 nm) were determined as reported elsewhere (Emamghoreishi et al, 1997). After measuring a stable fluorescence ratio (R) for 30 s to establish a baseline level, a maximally stimulating concentration of LPA (100 μM, determined in preliminary concentration–response experiments) was injected directly into the sample as a bolus using a 50 μl Hamilton syringe. Subsequently, R was measured for an additional 270 s to determine peak response and initial decay phases of the stimulated [Ca2+]i mobilization. Determination of and correction for autofluorescence was performed using the DMSO blank samples processed in parallel (Emamghoreishi et al, 1997). For calibration of Fura-2 fluorescence intensities, equivalent aliquots of cells were lysed with 0.05% Triton X-100 in a 1 mM CaCl2 medium and Rmax was measured. EGTA (6 mM, 30 mM Tris, pH 8.5) was then added and Rmin was measured. [Ca2+]i was then calculated using the Grynkiewicz equation (Grynkiewicz et al, 1985). Determinations were performed on duplicate aliquots of BLCLs from each subject and the mean values were used in all subsequent data analyses.
Thapsigargin stimulation
Determination of Ca2+ leakage from the ER and store depletion-induced SOCE was performed as previously described (Putney and Ribeiro, 2000), with modifications. This technique exploits the effects of TG to deplete TG-sensitive ER Ca2+ storage pools thereby providing a stimulus for opening of plasma membrane store-operated Ca2+ channels (SOCC) and influx of extracellular Ca2+. Cells (1–3 × 106/ml) were incubated with Fura-2 AM or DMSO vehicle, after which they were washed, resuspended in nominally Ca2+-free HEPES (HEPES 10 mM, glucose 10 mM, NaCl 140 mM, KCl 5 mM, MgCl2 1 mM) buffer and transferred to a spectrophotofluorometric cuvette, equilibrated, and free- and Ca2+-bound Fura-2 fluorescence intensities determined as above. After measuring baseline R for 30 s, a maximally stimulating concentration of TG (200 nM, confirmed in preliminary experiments) was injected as a bolus into the sample. Subsequently, R was measured for an additional 360 s to ensure depletion of TG-sensitive ER Ca2+ storage pools and to allow Ca2+ levels to recede to a stable secondary baseline. Extracellular [Ca2+] was then rapidly raised to physiological concentrations by addition of CaCl2 to a final concentration of 1 mM. R was measured for an additional 300 s to assess the degree of SOCE induced by the ER Ca2+ depletion stimulus. Correction for autofluorescence and calibration of Fura-2 fluorescence intensities were performed using equivalent aliquots of cells and [Ca2+]i calculated as above. Determinations were performed on duplicate aliquots of BLCLs as above and the mean values were used in all subsequent data analyses.
Statistics
Data are presented as means±standard error of the mean (SEM). Differences in the proportion of males to females in each diagnostic group were analyzed by a χ2 test. After confirming homogeneity of variance (Levine's test), differences in dependent variables between subject groups were analyzed by repeated measures multivariate analysis of variance (MANOVA) with diagnostic group and drug treatment as factors. Subsequent repeated measures univariate analyses (ANOVA) were used to determine the differences in specific dependent variables. Dependent measures determined in the LPA-stimulated Ca2+ mobilization paradigm were analyzed separately from those of the TG-stimulation protocol. This was done to avoid the reduced power of a single MANOVA, using all dependent cellular measures, resulting from exclusion of records with missing values: the cumulative loss of samples due to procedural difficulties resulted in a number of missing values among each set of experimental parameters. Differences between acute and chronic lithium treatment were analyzed by repeated measures ANOVA followed by simple contrasts to distinguish effects of time of exposure compared with vehicle control. Potential effects of other factors, including mood state and type of mood stabilizer treatment at the time of study, familial history of mood disorders, and psychiatric comorbidities, were assessed statistically using repeated measures ANOVA with the demographic characteristic as the between-subject factor, followed by Tukey's HSD test for post hoc comparisons. Statistical differences with two-tailed probability values of p<0.05 were taken as significant. Statistical analyses were performed using the SPSS (version 9.5, Chicago, IL) statistical package.
RESULTS
Subjects
Table 1 summarizes the demographic characteristics of the BD-I patients and healthy comparison subjects from whom BLCLs were used in this study. While BLCL samples were regrown from 26 BD-I patients and 16 healthy subjects, the actual numbers of subject samples analyzed for each parameter were less due to methodological difficulties resulting in sample loss during one or the other of the assay protocols used. Patient and healthy subject groups did not differ statistically in proportion of females to males (χ2=1.27, p=0.26) or in mean age (t=0.994, p=0.33).
Effect of Chronic Lithium Treatment on Agonist-Stimulated Intracellular Ca2+ Mobilization
Figure 1a depicts a representative response to LPA stimulation in BLCLs incubated for 7 days with 0.75 mM LiCl or vehicle. LPA evoked a rapid rise in [Ca2+]i from [Ca2+]B reaching a peak response (peak [Ca2+]S) between 20 and 100 s after stimulation, following which it declined towards baseline levels. The decay phase reflects the restitution of Ca2+ towards baseline levels through homeostatic control mechanisms including plasma membrane and ER Ca2+ ATPase pumps (Brini and Carafoli, 2000) and Na+/Ca2+ exchangers (Blaustein and Lederer, 1999). The parameters examined for lithium modulation in this paradigm included the [Ca2+]B, peak [Ca2+]S, the absolute difference (Δ[Ca2+]S) between [Ca2+]S and [Ca2+]B, and the slope of the initial rate of rise in LPA-stimulated [Ca2+]S (d[Ca2+]S/dt).
Effect of Chronic Lithium Treatment on Agonist-Stimulated Ca2+ Mobilization and ER Store-Depletion-Induced Ca2+ Entry in BLCLs. Cells were pretreated for 7 days with LiCl (0.75 mM) or vehicle. Cytosolic Ca2+ levels ([Ca2+]i) were measured using the Ca2+-indicator Fura 2-AM as described in the Materials and methods. (a) Typical Ca2+ responses induced by 100 μM LPA in control (solid line) vs lithium-treated (broken line) cells from a healthy subject are shown. The arrow indicates the time of LPA administration. (b) Representative Ca2+ responses after the addition of 200 nM TG in Ca2+-free medium, followed by the reintroduction of 1 mM extracellular Ca2+ in control (solid line) vs lithium-treated (broken line) BLCLs from a healthy subject is shown. Arrows indicate the time of TG/extracellular Ca2+ administration.
The effect of chronic lithium treatment on the above parameters of Ca2+ mobilization in BLCLs from patients and healthy comparison subjects is presented in Figures 1a and 2. MANOVA revealed significant main effects of lithium treatment (F=7.18; df=3,31; p=0.001) and diagnosis (F=3.42; df=3,31; p=0.03), but no interaction (F=0.243; df=3,31; p=0.87) between these factors. Subsequent univariate ANOVAs revealed significant effects of lithium treatment on [Ca2+]B (F=8.47; df=1,33; p=0.006), peak [Ca2+]S (F=9.94; df=1,33; p=0.003), and Δ[Ca2+]S (F=11.1; df=1,33; p=0.002), but not d[Ca2+]S/dt (F=1.54; df=1,33; p=0.224) in the LPA-stimulation protocol. While exposure of BLCLs to lithium for 7 days resulted in a modest but significant elevation in [Ca2+]B in both the patient (11.1%) and the healthy subject (10.0%) groups, the same treatment caused a significant attenuation in both [Ca2+]S (12.2% lower in patients, 11.1% lower in healthy subjects) and Δ[Ca2+]S (14.1% lower in patients, 12.3% lower in healthy subjects) compared to vehicle treatment. The d[Ca2+]S/dt was also reduced in lithium-treated samples (11.5%) but the difference was not statistically significant.
Effect of Chronic Lithium Treatment on Parameters of LPA-Stimulated Intracellular Calcium Mobilization. Cells were incubated for 7 days with LiCl (0.75 mM) or vehicle. The [Ca2+]i was monitored prior to and following stimulation with 100 μM LPA as described in Figure 1a. Chronic lithium treatment increased basal intracellular Ca2+ levels ([Ca2+]B) (a) and attenuated the absolute difference between [Ca2+]S and [Ca2+]B (Δ[Ca2+]S) (b) in response to LPA stimulation in BLCLs from both healthy subjects and BD-I patients. The open bars (□) represent vehicle-treated BLCLs, while the solid bars (▪) represent BLCLs treated chronically with lithium. Values represent the mean and SEM of determinations made in 15 healthy subjects and 20 BD-I patients. *p<0.05 compared to vehicle-treated BLCLs (ANOVA with Tukey's post hoc tests).
To test whether the above lithium-induced changes were dependent on the duration of exposure, BLCLs from a subset of subjects (eight patients, two healthy) were treated for 24 h or 7 days with 0.75 mM lithium or vehicle, and LPA-stimulated Ca2+ responses determined. As shown in Figure 4a and b, acute lithium treatment did not significantly influence [Ca2+]B and peak [Ca2+]S in BLCLs (simple contrasts: F=1.73; df=1,9; p=0.22 and F=1.55; df=1,9; p=0.245, respectively) in contrast to the chronic lithium treatment paradigm (F=4.28; df=1,9; p=0.068 and F=21.0; df=1,9; p=0.001, respectively).
Effect of Acute vs Chronic Lithium Treatment on Basal Ca2+ levels, LPA-stimulated Ca2+ Mobilization, and Thapsigargin-Induced Store-Operated Ca2+ Entry. BLCLs were treated with vehicle (open bars) or with LiCl (0.75 mM) for 24 h (hatched bars) or 7 days (closed bars ▪). Cells loaded with Fura-2 were challenged with LPA (a, b) or TG-induced SOCC (c, d) as described in Figure 1. Values represent the mean and SEM of determinations made in two healthy subjects and eight BD-I patients (a, b) or five healthy and 10 BD-I patients (c, d). *p<0.05 and †p=0.068 compared to vehicle-treated BLCLs (repeated measures ANOVA with simple contrasts).
Effect of Chronic Lithium Treatment on Thapsigargin-Sensitive ER Ca2+ Release and Parameters of SOCE
Figure 1b demonstrates the time course of TG-induced depletion of intracellular Ca2+ stores and subsequent store depletion-stimulated influx of extracellular Ca2+ in BLCLs incubated for 7 days with 0.75 mM lithium or vehicle. In a Ca2+-free medium, the addition of TG (200 nM) caused a slow increase in BLCL [Ca2+]i to a new baseline ([Ca2+]B2). Subsequent addition of Ca2+ (1 mM) resulted in a rapid rise of [Ca2+]i confirming the well-known observation obtained in other cell types that sustained Ca2+ entry is linked to store depletion induced by TG (Putney et al, 2001). Parameters measured to characterize the TG-induced SOCE response include the [Ca2+]B, peak TG-sensitive [Ca2+]i accumulation ([Ca2+]TG), the baseline plateau before reintroduction of Ca2+ to the external medium ([Ca2+]B2, the peak of Ca2+ influx ([Ca2+]influx), the difference between [Ca2+]influx and [Ca2+]B2 (Δ[Ca2+]influx), and the slope of the initial phase of rise in [Ca2+]influx (d[Ca2+]influx/dt).
The effects of chronic lithium treatment on the parameters of the ‘TG-Ca2+ add back protocol’ in BLCLs from the BD patients and healthy comparison subjects are presented in Figures 1b and 3. Repeated measures MANOVA of these parameters revealed a significant effect of lithium treatment (F=8.36; df=5,30; p=0.00005) but not diagnosis (F=1.28; df=5,30; p=0.30), and no significant interaction (F=0.551; df=5,30; p=0.74) between these two factors. Subsequent univariate ANOVAs revealed significant effects of chronic lithium treatment on [Ca2+]B (F=9.42; df=1,34; p=0.004), [Ca2+]B2 (F=10.1; df=1,34; p=0.003), [Ca2+]influx (F=8.36; df=1,34; p=0.007), and Δ[Ca2+]influx (F=11.7; df=1,34; p=0.002), but not [Ca2+]TG (F=1.22; df=1,34; p=0.278) or d[Ca2+]influx/dt (F=2.49; df=1,34; p=0.124), in TG-stimulated BLCLs. [Ca2+]B and [Ca2+]B2were significantly higher in BLCLs treated with lithium compared with vehicle control in both the patient (12.0 and 8.8%, respectively) and healthy subjects (7.0 and 13.3%, respectively). As well, chronic lithium treatment modestly, but significantly, attenuated both [Ca2+]influx (9.0% in BD-I, 7.9% in healthy subjects) as well as Δ[Ca2+]influx (10.6% lower in BD-I, 10.4% lower in healthy subjects). As with LPA-stimulated Ca2+ mobilization, there was no difference in [Ca2+]B between vehicle and acute lithium-treated samples (F=1.45; df=1,13; p=0.25; Figure 4c), whereas the difference between vehicle and chronically treated samples was statistically significant (F=4.36; df=1,9; p=0.05). Similarly, while [Ca2+]B2 in BLCLs treated for 24 h with lithium were not significantly reduced (F=3.15; df=1,13; p=0.10), those treated for 7 days demonstrated higher [Ca2+]B2 compared with vehicle (12.5%, F=8.65; df=1,13; p=0.01; data not shown). Finally, while [Ca2+]influx did not differ between vehicle and acute lithium treatment conditions (F=1.39; df=1,13; p=0.26; Figure 4d), it was in fact reduced in chronic lithium-treated BLCLs compared with the vehicle-treated condition (F=5.17; df=1,13; p=0.04).
Effect of Chronic Lithium Treatment on Parameters of Thapsigargin-Induced Store Depletion and Store-Operated Ca2+ Entry. Cells were incubated for 7 days with LiCl (0.75 mM) or vehicle. Store-operated Ca2+ entry was monitored using the ‘TG-Ca2+ add back’ protocol as described in Figure 1b. Chronic lithium exposure increased the basal intracellular Ca2+ levels prior to ([Ca2+]B) (a) and following TG challenge ([Ca2+]B2) (b) and attenuated the absolute difference between [Ca2+]influx and [Ca2+]B2 (Δ[Ca2+]influx) (c) in response to the readdition of extracellular Ca2+, in BLCLs from both healthy subjects and BD-I patients. Open bars (□) represent vehicle-treated BLCLs, while solid bars (▪) represent BLCLs treated chronically with lithium. Values represent the mean and SEM of determinations made in 13 healthy subjects and 24 BD-I patients. *p<0.05 compared to vehicle-treated BLCLs (ANOVA with Tukey's post hoc tests).
Relationship Between Calcium Mobilization Parameters and Bipolar Patient Characteristics
Other than the observation of significantly higher [Ca2+]B in BLCLs from bipolar patients on lithium monotherapy at the time of the study compared with healthy subjects (F=3.11; df=3,24; p=0.04) there were no statistically significant differences found in the LPA- and TG-induced Ca2+ mobilization indices measured within the patient group stratified on factors of mood state of illness at time of study (healthy subjects, and euthymic, depressed, and hypomanic/manic bipolar patients, F's=0.06–1.69; df=3,26; p's>0.2), psychiatric comorbidity (healthy subjects and bipolar patients with no comorbidity, alcohol abuse/dependence, or other comorbidity, F's=0.41–1.63; df=3,26; p's>0.21) and family history of mood disorders (healthy subjects, positive, negative, or unknown, F's=0.26–2.56; df=3,26; p's ⩾0.08) (data not shown).
DISCUSSION
The principal findings of this study are that chronic, but not acute, treatment of BLCLs from both BD-I patients and healthy subjects with a therapeutically relevant concentration of lithium significantly attenuated LPA-stimulated Ca2+ responses (a G-protein-coupled receptor activated signaling pathway), and TG-evoked store-depletion-induced Ca2+ influx (a measure of SOCE). At the same time, [Ca2+]B was significantly elevated by chronic, but not acute, lithium treatment. Taken together, these findings support the notion that lithium alters key processes regulating intracellular Ca2+ homeostasis, effects which may be particularly relevant to understanding the molecular and cellular actions responsible for its therapeutic effects.
As the pharmacological agents used to probe intracellular Ca2+ homeostatic control in this study act on cascades of interacting proteins and second messengers, the loci at which lithium acts to produce the observed effects can only be surmised in broad terms. It is unlikely, however, that the attenuating effects of lithium are related to factors that modify the rate of Ca2+ mobilization following agonist stimulation or the rate of Ca2+ influx induced by store depletion as these changes occurred without statistically significant differences in d[Ca2+]S/dt and d[Ca2+]influx/dt, the initial rates of activation of these responses. Furthermore, they do not appear to be related to an effect of lithium to reduce the size of the TG-sensitive ER stores, since neither acute nor chronic lithium treatment had any significant effect on [Ca2+]TG.
As SOCE may contribute to the net Ca2+ entry in the LPA (Warsh et al, unpublished data) as well as in the TG-stimulation paradigms (Putney et al, 2001), an effect of lithium on mechanisms regulating SOCE could be expected to attenuate both responses. As TG induces store depletion through an IP3 receptor (IP3R)-independent mechanism, the effect of lithium on this SOCE component is likely to be related to actions distinct from its well-established modulatory effect on PI signaling (Hallcher and Sherman, 1980; Berridge et al, 1982). The SOCE apparatus is complex, involving the orchestrated action of SOCC, IP3Rs, and SERCAs (Barritt, 1999; Putney et al, 2001). Functional interactions between mitochondria and ER can also influence Ca2+ mobilization through SOCE (Fall and Keizer, 2001). While knowledge is sparse on the effects of lithium on these families of membrane proteins, the observed increase in [Ca2+]B would not be expected if the attenuating effect of lithium on the stimulated Ca2+ mobilization were due to upregulation of the levels and/or function of PMCAs or SERCAs. Similarly, the lack of differences in [Ca2+]TG argues against an effect of lithium on the functional activity of the SERCAs.
The potential involvement of TRPM2 or other members of the family of TRP proteins in the effect of lithium to attenuate LPA- and TG-stimulated Ca2+ mobilization also merits consideration. TRPM2 mRNA levels were significantly reduced in BLCLs from BD patients showing elevated BLCL [Ca2+]B and varied inversely with [Ca2+]B (Yoon et al, 2001b). Furthermore, in preliminary experiments, sustained elevation of BLCL [Ca2+]i by ionomycin treatment suppressed TRPM2 mRNA levels (Yoon, 2002). While chronic lithium treatment suppresses TRPC3 protein levels in BLCLs from BD patients (Andreopoulos et al, 2003), the extent to which protein and mRNA levels of TRPM2 and other TRP proteins expressed in BLCLs are also downregulated and the relationship of any such changes to the altered functional indices demonstrated in this work remain to be elaborated.
It is also possible that the effect of chronic lithium treatment to attenuate LPA-stimulated Ca2+ mobilization is mediated through a process distinct from that which affects the TG-evoked SOCE response. In addition to inhibiting IMPase (Hallcher and Sherman, 1980), lithium could attenuate LPA-stimulated Ca2+ mobilization by inhibiting Gβγ-mediated responses. Chronic lithium administration has been demonstrated to interfere with the dissociation of Gi into its active components, thereby removing the tonic inhibitory influence on adenylyl cyclase and diminishing signal transduction through the PI/IP3 system (Masana et al, 1992; Wang and Friedman, 1999). Chronic lithium treatment has also been shown to reduce receptor G-protein coupling (Wang and Friedman, 1999) and decrease both receptor- and postreceptor-stimulated PI hydrolysis (reviewed in Hudson et al, 1993; Jope and Williams, 1994).
The extent to which the modulatory effect of lithium on intracellular Ca2+ mobilization in the current cellular paradigm represents a primary effect on one or more of the elements in the PI/Ca2+ signaling system, as opposed to a secondary one mediated through cross-talk mechanisms also merits consideration. For example, cAMP-mediated signaling promotes the inhibition of Ca2+ influx (Rasmussen, 1986), modulates IP3Rs (Supattapone et al, 1988; Patel et al, 1999), and enhances the removal of Ca2+ from the cytosol by promoting the action of PMCA pumps (Helman et al, 1986). As well, protein kinase A (PKA) can modulate the PI/Ca2+ signaling system through the phosphorylation of several intracellular targets including receptors, G proteins, PI kinase, and phospholipase C (Supattapone et al, 1988; Hajnoczky et al, 1993; Galas and Harden, 1997). Abnormalities of the cAMP-PKA signaling cascade have also been implicated in the pathophysiology of BD and as a target of lithium action (Perez et al, 2000; Chang et al, 2002). Furthermore, the cAMP system is, in turn, subject to cross-regulation by Ca2+ signaling through regulation at a variety of points in the cAMP signaling cascade (Choi et al, 1993; Cooper et al, 1995). Thus, it may be that multiple actions of lithium on diverse signal transduction systems are essential to its therapeutic efficacy in BD.
While the decrements in LPA-stimulated Ca2+ mobilization and TG-induced Ca2+ influx caused by chronic lithium treatment were modest, the true magnitude of the attenuating effects may have been underestimated. Fura-2, which has a Kd for Ca2+ in the order of 224 nM (at 37°C) (Nuccitelli, 1994), becomes increasingly saturated at high [Ca2+]i, such as attained with the LPA and TG protocols used in this study. Thus, at such high Ca2+ concentrations (eg 700–1000 nM), Fura-2 would be relatively less sensitive to changes in [Ca2+]i providing only an approximation of the true magnitude of the Ca2+ changes. Although higher affinity fluorescence Ca2+ chelating dyes are available (Nuccitelli, 1994), their use would have been at the expense of accurately estimating the [Ca2 +]B. Second, because the Ca2+ assay employed gives a ‘static’ measure, averaged across the entire population of cells in the light beam path of the fluorometer, it does not provide a dynamic picture of the effects that may occur in subpopulations of responding cells in which differences may be more pronounced. Finally, differences observed in this study may also have been affected by phenotypic heterogeneity of the BD patient population studied, a known confounding factor in genetic and molecular investigations of BD (Goodwin and Jamison, 1990; Lenox et al, 2002).
The attenuating effects of lithium on LPA- and TG-induced Ca2+ mobilization were only evident after 7 days but not 24 h of exposure suggesting that these effects are a result of chronic exposure to lithium. This duration of treatment, which has been widely used in studies of mood stabilizer actions in cell lines (Varney et al, 1992; Ozaki and Chuang, 1997; Yamaji et al, 1997; Nonaka et al, 1998; Wang et al, 2001), is one through which drug exposure can be managed without inducing significant cellular toxicity (BLCL viability after 7 days exposure >95%). While this time interval is still shorter than that required for full clinical response to lithium, antimanic effects of lithium are evident at as early as 1 week of treatment (Schou, 1968). Also, unlike the clinical situation, in which pharmacokinetic factors contribute, in part, to latency of onset of action, cells studied in the ex vivo paradigm here are directly and immediately exposed to a constant therapeutic concentration of lithium, thus presumably expediting the onset of biochemical actions. Finally, the lithium concentration used in this study (0.75 mM) falls in the mid-therapeutic range of serum concentrations (0.5–1.0 mM) used to guide lithium dosing clinically (Gelenberg et al, 1989) and within the range of those achieved in brain during therapeutic dosing (Kato et al, 1993; Plenge et al, 1994). However, the use of a single lithium concentration in this study precludes conclusions regarding whether the observed effects of lithium on parameters of Ca2+ mobilization were dose-dependent or maximal.
The lack of a differential effect of lithium on the Ca2+ mobilization in BLCLs from BD patients as compared with those from healthy subjects also merits consideration as it might question the therapeutic implications of lithium-induced Ca2+ mobilization changes observed. However, this could be related to several factors, including insensitivity to detect a small effect in a relatively small subject sample population, the limited sensitivity of the Ca2+ indicator used at high [Ca2+]S, as noted above, and the relatively large variance in the assay of LPA-stimulated Ca2+ mobilization. While the duration of exposure to lithium is sufficient to demonstrate certain chronic effects, as argued above, it may still be too short to capture cellular and molecular changes that evolve more slowly, in perhaps a diagnosis-specific fashion.
The alterations seen following chronic lithium treatment in this nonexcitable cell paradigm likely represent only one of a sequence of changes that, in neurons, act in conjunction to ‘correct’ disturbed Ca2+ homeostasis. In this regard, chronic lithium treatment also inhibits NMDA receptor-induced Ca2+ influx possibly by decreasing NR2B tyrosine phosphorylation (Hashimoto et al, 2002), effects that may underlie its protective actions against glutamate-induced excitotoxicity. Finally, the effects of lithium to attenuate stimulus-induced Ca2+ mobilization at the same time as elevating resting levels recalls the ‘bimodal hypothesis’ (Jope, 1999) that lithium normalizes the balance between positive and negative regulators of intracellular signal transduction processes, thereby stabilizing and maintaining their function within an optimal range. In this context, Ca2+ signaling modulates gene expression and protein function through spatially regulated changes in frequency and amplitude of intracellular Ca2+ waves (Ghosh and Greenberg, 1995). Stabilization of fluctuations in intracellular Ca2+ levels by lithium could significantly modify the transcriptional regulation and expression of key neuronal proteins that, in turn, correct aberrant neuronal activity in critical brain regions involved in mood regulation. As the integrity of intracellular Ca2+ homeostasis is critical to cell survival, these effects of lithium on Ca2+ signaling processes may also be relevant mechanistically to its neuroprotective effects, now thought to be important in the clinical action of this agent (Manji et al, 2000).
In conclusion, the findings of the current study suggest that chronic lithium treatment modifies processes that impact on intracellular Ca2+ signaling and homeostasis. Taken together with our recent report suggesting Ca2+ signaling may be hyperactive in BLCLs from patients with BD (Wasserman et al, 2003), a cellular model that may report disturbances particularly relevant to the pathophysiology of this disorder, these observations suggest that the regulation of intracellular Ca2+ homeostasis may be especially pertinent to the therapeutic action of lithium. In this regard, lithium's modulation of intracellular Ca2+ signaling, be it direct or indirect, could have important implications in terms of stabilizing gene expression, cellular communication, and perhaps excitotoxic or apoptotic cell death.
References
Andreopoulos S, Wasserman MJ, Li PP, Warsh JJ (2003). Bipolar disorder-specific reduction of transient receptor potential channel-3 levels in B lymphoblasts exposed chronically to lithium. Bipolar Disord 5: 29.
Barritt GJ (1999). Receptor-activated Ca2+ inflow in animal cells: a variety of pathways tailored to meet different intracellular Ca2+ signaling requirements. Biochem J 337: 153–169.
Berk M, Bodemer W, Oudenhove TV, Butkow N (1995). The platelet intracellular calcium response to serotonin is augmented in bipolar manic and depressed patients. Hum Psychopharmacol 10: 189–193.
Berridge MJ (1995). Inositol trisphosphate and calcium signaling. Ann NY Acad Sci 766: 31–43.
Berridge MJ, Downes CP, Hanley MR (1982). Lithium amplifies agonist-dependent phosphatidylinositol responses in brain and salivary glands. Biochem J 206: 587–595.
Berridge MJ, Lipp P, Bootman MD (2000). The versatility and universality of calcium signaling. Nat Rev Mol Cell Biol 1: 11–21.
Blaustein MP, Lederer WJ (1999). Sodium/calcium exchange: its physiological implications. Phys Rev 79: 763–854.
Brini M, Carafoli E (2000). Calcium signaling: a historical account, recent developments and future perspectives. Cell Mol Life Sci 57: 354–370.
Chang A, Li PP, Warsh JJ (2002). cAMP signal transduction in the pathophysiology of mood disorders: contributions from postmortem studies. In: Agam G, Everall IP, Belmaker RH (eds). The Postmortem Brain in Psychiatric Research. Kluwer Academic Publishers: Boston. pp 341–361.
Choi SJ, Xia Z, Villacres EC, Storm DR (1993). The regulatory diversity of the mammalian adenylyl cyclases. Curr Opin Cell Biol 5: 269–273.
Cooper DM, Mons N, Karpen JW (1995). Adenylyl cyclases and the interaction between calcium and cAMP signaling. Nature 347: 421–424.
Dubovsky SL, Christiano J, Daniell LC, Franks RD, Murphy J, Adler L et al (1989). Increased platelet intracellular calcium concentration in patients with bipolar affective disorders. Arch Gen Psychiatry 46: 632–638.
Dubovsky SL, Lee C, Christiano J, Murphy J (1991). Lithium decreases platelet intracellular calcium concentration in bipolar patients. Lithium 2: 167–174.
Dubovsky SL, Murphy J, Thomas M, Rademacher J (1992). Abnormal intracellular calcium ion concentration in platelets and lymphocytes of bipolar patients. Am J Psychiatry 149: 118–120.
Dubovsky SL, Thomas M, Hijazi A, Murphy J (1994). Intracellular calcium signaling in peripheral cells of patients with bipolar affective disorder. Eur Arch Psychiatry Clin Neurosci 243: 229–234.
Emamghoreishi M, Schlichter L, Li PP, Parikh S, Sen J, Kamble A et al (1997). High intracellular calcium concentrations in transformed lymphoblasts from subjects with bipolar I disorder. Am J Psychiatry 154: 976–982.
Fall CP, Keizer JE (2001). Mitochondrial modulation of intracellular Ca(2+) signaling. J Theor Biol 210: 151–165.
First M, Spitzer R, Gibbon M, Williams JBW (1995a). Structured Clinical Interview for DSM-IV Axis I Disorders—Nonpatient Edition (SCID-I/NP, Version 2.0). Biometrics Research Department, New York Psychiatric Institute: New York, NY.
First M, Spitzer RL, Robert L, Gibbon M, Williams JBW (1995b). Structured Clinical Interview for DSM-IV Axis I Disorders—Patient Edition (SCID-I/P, Version 2.0). Biometrics Research Department, New York State Psychiatric Institute: New York, NY.
Forstner U, Bohus M, Gebickeharter PJ, Baumer B, Berger M, Van Calker D (1994). Decreased agonist-stimulated Ca2+ response in neutrophils from patients under chronic lithium therapy. Eur Arch Psychiatry Clin Neurosci 243: 240–243.
Galas MC, Harden TK (1997). Cyclic AMP-induced desensitization of G-protein-regulated phospholipase C in turkey erythrocyte membranes. Eur J Pharmacol 314: 157–164.
Gelenberg AJ, Carroll JA, Baudhuin MG, Jefferson JW, Greist JH (1989). The meaning of serum lithium levels in maintenance therapy of mood disorders: a review of the literature. J Clin Psychiatry 50(Suppl): 17–22.
Ghosh A, Greenberg ME (1995). Calcium signaling in neurons: molecular mechanisms and cellular consequences. Science 268: 239–247.
Goodwin FK, Jamison KR (1990). Manic-Depressive Illness. Oxford University Press: New York.
Grynkiewicz G, Poenie M, Tsien RY (1985). A new generation of Ca2+ indicators with greatly improved fluorescence properties. J Biol Chem 260: 3440–3450.
Hajnoczky G, Gao E, Nomura T, Hoek JB, Thomas AP (1993). Multiple mechanisms by which protein kinase A potentiates inositol 1,4,5-trisphosphate-induced Ca2+ mobilization in permeabilized hepatocytes. Biochem J 293: 413–422.
Hallcher LM, Sherman WR (1980). The effects of lithium ion and other agents on the activity of myo-inositol-1-phosphatase from bovine brain. J Biol Chem 255: 10896–10901.
Hashimoto R, Hough C, Nakazawa T, Yamamoto T, Chuang DM (2002). Lithium protection against glutamate excitotoxicity in rat cerebral cortical neurons: involvement of NMDA receptor inhibition possibly by decreasing NR2B tyrosine phosphorylation. J Neurochem 80: 589–597.
Helman J, Kuyatt BL, Takuma T, Seligmann B, Baum BJ (1986). ATP-dependent calcium transport in rat parotid basolateral membrane vesicles. Modulation by agents which elevate cyclic AMP. J Biol Chem 261: 8919–8923.
Hough C, Lu S-J, Davis CL, Chuang D-M, Post RM (1999). Elevated basal and thapsigargin-stimulated intracellular calcium of platelets and lymphocytes from bipolar affective disorder patients measured by a fluorometric microassay. Biol Psychiatry 46: 247–255.
Hudson CJ, Young LT, Li PP, Warsh JJ (1993). CNS transmembrane signal transduction in the pathophysiology and pharmacology of affective disorders and schizophrenia. Synapse 13: 278–293.
Jope RS (1999). A bimodal model of the mechanism of action of lithium. Mol Psychiatry 4: 21–25.
Jope RS, Song L, Li PP, Young LT, Kish SJ, Pacheco MA et al (1996). The phosphoinositide signal transduction system is impaired in bipolar affective disorder brain. J Neurochem 66: 2402–2409.
Jope RS, Williams MB (1994). Lithium and brain signal transduction systems. Biochem Pharmacol 47: 429–441.
Kato T, Shioiri T, Inubushi T, Takahashi S (1993). Brain lithium concentrations measured with lithium-7 magnetic resonance spectroscopy in patients with affective disorders—relationship to erythrocyte and serum concentrations. Biol Psychiatry 33: 147–152.
Kusumi I, Koyama T, Yamashita I (1994). Serotonin-induced platelet intracellular calcium mobilization in depressed patients. Psychopharmacology (Berl) 113: 322–327.
Lenox RH, Gould TD, Manji HK (2002). Endophenotypes in bipolar disorder. Am J Med Genet 114: 391–406.
Lenox RH, McNamara RK, Papke RL, Manji HK (1998). Neurobiology of lithium: an update. J Clin Psychiatry 59(Suppl 6): 37–47.
Manji HK, McNamara R, Chen G, Lenox RH (1999). Signaling pathways in the brain: cellular transduction of mood stabilization in the treatment of manic-depressive illness. Aust NZ J Psychiatry 33(Suppl): S65–S83.
Manji HK, Moore GJ, Chen G (2001). Bipolar disorder: leads from the molecular and cellular mechanisms of action of mood stabilizers. Br J Psychiatry 41(Suppl): s107–s119.
Manji HK, Moore GJ, Rajkowska G, Chen G (2000). Neuroplasticity and cellular resilience in mood disorders. Mol Psychiatry 5: 578–593.
Masana MI, Bitran JA, Hsiao JK, Potter WZ (1992). In vivo evidence that lithium inactivates Gi modulation of adenylate cyclase in brain. J Neurochem 59: 200–205.
Mattson MP (2000). Apoptosis in neurodegenerative disorders. Nat Rev Mol Cell Biol 1: 120–129.
Nonaka S, Hough CJ, Chuang DM (1998). Chronic lithium treatment robustly protects neurons in the central nervous system against excitotoxicity by inhibiting N-methyl-D-aspartate receptor-mediated calcium influx. Proc Natl Acad Sci USA 95: 2642–2647.
Nuccitelli R (1994). Methods in Cell Biology, Volume 40: A Practical Guide to the Study of Calcium in Living Cells. Academic Press: New York.
Okamoto Y, Kagaya A, Motohashi N, Yamawaki S (1995). Inhibitory effects of lithium ion on intracellular Ca2+ mobilization in the rat hippocampal slices. Neurochem Int 26: 233–238.
Ozaki N, Chuang DM (1997). Lithium increases transcription factor binding to AP-1 and cyclic AMP-responsive element in cultured neurons and rat brain. J Neurochem 69: 2336–2344.
Patel S, Joseph SK, Thomas AP (1999). Molecular properties of inositol 1,4,5-trisphosphate receptors. Cell Calcium 25: 247–264.
Perez J, Tardito D, Mori S, Racagni G, Smeraldi E, Zanardi R (2000). Abnormalities of cAMP signaling in affective disorders: implication for pathophysiology and treatment. Bipolar Disord 2: 27–36.
Plenge P, Stensgaard A, Jensen HV, Thomsen C, Mellerup ET, Henriksen O (1994). 24-hour lithium concentration in human brain studied by Li-7 magnetic resonance spectroscopy. Biol Psychiatry 36: 511–516.
Putney JW, Broad LM, Braun FJ, Lievremont JP, Bird GS (2001). Mechanisms of capacitative calcium entry. J Cell Sci 114: 2223–2229.
Putney JW, Ribeiro CM (2000). Signaling pathways between the plasma membrane and endoplasmic reticulum calcium stores. Cell Mol Life Sci 57: 1272–1286.
Rasmussen H (1986). The calcium messenger system (1). N Engl J Med 314: 1094–1101.
Rosskopf D, Daelman W, Busch S, Schurks M, Hartung K, Kribben A et al (1998). Growth factor-like action of lysophosphatidic acid on human B lymphoblasts. Am J Physiol 274: C1573–C1582.
Schou M (1968). Lithium in psychiatric therapy and prophylaxis. J Psychiatr Res 6: 67–95.
Schou M (2001). Lithium treatment at 52. J Affect Disord 67: 21–32.
Supattapone S, Danoff SK, Theibert A, Joseph SK, Steiner J, Snyder SH (1988). Cyclic AMP-dependent phosphorylation of a brain inositol trisphosphate receptor decreases its release of calcium. Proc Natl Acad Sci USA 85: 8747–8750.
Szalai G, Krishnamurthy R, Hajnoczky G (1999). Apoptosis driven by IP(3)-linked mitochondrial calcium signals. EMBO J 18: 6349–6361.
Tan CH, Javors MA, Seleshi E, Lowrimore PA, Bowden CL (1990). Effects of lithium on platelet ionic intracellular calcium concentration in patients with bipolar (manic-depressive) disorder and healthy controls. Life Sci 46: 1175–1180.
Varney MA, Godfrey PP, Drummond AH, Watson SP (1992). Chronic lithium treatment inhibits basal and agonist-stimulated responses in rat cerebral cortex and GH3 pituitary cells. Mol Pharmacol 42: 671–678.
Wang HY, Friedman E (1999). Effects of lithium on receptor-mediated activation of G proteins in rat brain cortical membranes. Neuropharmacology 38: 403–414.
Wang L, Liu X, Lenox RH (2001). Transcriptional down-regulation of MARCKS gene expression in immortalized hippocampal cells by lithium. J Neurochem 79: 816–825.
Wasserman MJ, Warsh JJ, Li PP, Pennefather P, Sibony D (2003). Hyperactive intracellular calcium mobilization in B lymphoblasts from patients with bipolar I disorder. Biol Psychiatry 53(Suppl): 79S.
Williams RS, Harwood AJ (2000). Lithium therapy and signal transduction. Trends Pharmacol Sci 21: 61–64.
Yamaji T, Kagaya A, Uchitomi Y, Yokota N, Yamawaki S (1997). Chronic treatment with antidepressants, verapamil, or lithium inhibits the serotonin-induced intracellular calcium response in individual C6 rat glioma cells. Life Sci 60: 817–823.
Yoon I-S (2002). Molecular analysis of altered calcium homeostas in bipolar disorder using differential and candid geno approach. PhD Thesis, University of Toronto.
Yoon IS, Li PP, Siu KP, Kennedy JL, Cooke RG, Parikh SV et al (2001a). Altered IMPA2 gene expression and calcium homeostasis in bipolar disorder. Mol Psychiatry 6: 678–683.
Yoon IS, Li PP, Siu KP, Kennedy JL, Macciardi F, Cooke RG et al (2001b). Altered TRPC7 gene expression in bipolar-I disorder. Biol Psychiatry 50: 620–626.
Acknowledgements
A preliminary report of this work was presented at the 57th annual meeting of the Society for Biological Psychiatry, Philadelphia, PA. This work was supported by the Canadian Institutes of Health Research (grants MOP12851 (JJW) and MOP53323 (JJW and PPL)). MJW is a recipient of a Research Studentship from the Ontario Mental Health Foundation and TWC was supported by a Natural Sciences & Engineering Research Council postgraduate scholarship and University of Toronto scholarship. We gratefully acknowledge the contributions of the physicians and research staff at the Centre for Addiction and Mental Health for their assistance in recruiting potential patient subjects for participation in these studies. Arvind Kamble and Kin Po Siu contributed to the technical laboratory aspects of this work and Bronwen Hughes in the clinical data collection and analysis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wasserman, M., Corson, T., Sibony, D. et al. Chronic Lithium Treatment Attenuates Intracellular Calcium Mobilization. Neuropsychopharmacol 29, 759–769 (2004). https://doi.org/10.1038/sj.npp.1300400
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.npp.1300400
Keywords
This article is cited by
-
Bipolar disorder-iPSC derived neural progenitor cells exhibit dysregulation of store-operated Ca2+ entry and accelerated differentiation
Molecular Psychiatry (2023)
-
Cellular calcium in bipolar disorder: systematic review and meta-analysis
Molecular Psychiatry (2021)
-
Lithium chloride enhances serotonin induced calcium activity in EGFP-GnIH neurons
Scientific Reports (2020)
-
The Oxford study of Calcium channel Antagonism, Cognition, Mood instability and Sleep (OxCaMS): study protocol for a randomised controlled, experimental medicine study
Trials (2019)
-
TRPC Channels: Prominent Candidates of Underlying Mechanism in Neuropsychiatric Diseases
Molecular Neurobiology (2016)