Abstract
While oral naltrexone is effective in treating alcohol and opiate dependencies, poor patient adherence and widely fluctuating plasma levels limit its efficacy. To overcome these problems, an extended-release formulation of naltrexone (Vivitrex®) was developed by encapsulating naltrexone into injectable, biodegradable polymer microspheres. Pharmacokinetic studies in rats demonstrated that this formulation produced stable, pharmacologically relevant plasma levels of naltrexone for approximately 1 month following either subcutaneous or intramuscular injections. While rats receiving placebo microspheres demonstrated a pronounced analgesic response to morphine in the hot-plate test, morphine analgesia was completely blocked in rats treated with extended-release naltrexone. This antagonism began on day 1 following administration and lasted for 28 days. Rats reinjected with extended-release naltrexone 34 days after the initial dose and tested for another 35 days showed consistent suppression of morphine analgesia for an additional 28 days. μ-Opioid receptor density, as measured by [3H]DAMGO autoradiography, increased up to two-fold following a single injection of extended-release naltrexone. Saturation binding assays using [3H]DAMGO showed changes in the midbrain and striatum at 1 week after extended-release naltrexone administration, and after 1 month in the neocortex. These receptor increases persisted for 2–4 weeks after dissipation of the morphine antagonist actions of naltrexone. These data suggest that therapeutically relevant plasma levels of naltrexone can be maintained using monthly injections of an extended-release microsphere formulation, and that changes in μ-opioid receptor density do not impact its efficacy in suppressing morphine-induced analgesia in the rat. Clinical trials of extended release naltrexone for treating alcohol and opiate dependency are currently ongoing.
Similar content being viewed by others
INTRODUCTION
Alcohol and opiate dependence represent serious medical problems in the United States and throughout the world. In the US alone, it is estimated that 10–14 million people are alcohol-dependent, while 1 million people suffer from opiate addiction (Grant, 1997). Evidence implicating the functional involvement of the endogenous opioid system in mediating many of the reinforcing aspects of drug consumption (Spanagel et al, 1992; Herz, 1997) has led to the use of opioid receptor antagonists as a pharmacothe-rapeutic intervention for treating drug dependency syndromes (Martin et al, 1973; Litten and Allen, 1998; Garbutt et al, 1999). The opiate antagonist naltrexone (Resnick et al, 1974) is effective and approved by the FDA for treating opiate and alcohol dependence (Food and Drug Administration NDA 18-932/S-010, 1994). Despite its utility, the efficacy of oral naltrexone in treating drug dependencies is limited by at least two deficiencies. The first involves poor adherence to the prescribed daily dosing schedule (Volpicelli et al, 1997). Although adherence is important in achieving efficacy with all drugs, it is particularly important in treating alcohol and opiate dependence. In these syndromes, the compulsion to self-administer drugs directly conflicts with the need to remain abstinent. This daily conflict further exacerbates problems of poor adherence, contributing to the ‘spiral towards relapse’ common to both maladies. Indeed, a recent study of alcoholics (Volpicelli et al, 1997) found that patients who were highly adherent benefited significantly from naltrexone, while nonadherent patients responded no differently than those receiving placebo. Moreover, it is not uncommon for less than 30% of the opioid-dependent patients to continue with antagonist therapy for more than 6 months (Greenstein et al, 1984; Capone et al, 1986; D'Ippoliti et al, 1998). These data argue that the efficacy of naltrexone might be significantly enhanced if adherence could be improved. A second deficiency with oral naltrexone involves the widely fluctuating plasma levels that occur with daily oral dosing (Verebey, 1980). These daily fluctuations may cause side effects during peak plasma levels (Croop et al, 1997; King et al, 1997), while compromising efficacy during the nadir in plasma concentration (Verebey, 1980).
One approach for improving upon the effectiveness of naltrexone would be to develop an injectable formulation that would maintain plasma levels within the therapeutic range for several weeks, but below levels that induce serious side effects. Polymers such as poly-lactide co-glycolide (PLG, (Shive and Anderson, 1997)) can be formulated into small-diameter (<100 μm), injectable microspheres that incorporate active moieties to provide extended release for several weeks (Lewis, 1990). Such an extended-release formulation of naltrexone might provide several advantages over oral naltrexone, including a significant reduction in daily high plasma peaks and a decrease in the gastrointestinal exposure and first-pass hepatic metabolism associated with oral delivery (Kranzler et al, 1998). These improvements could reduce the incidence of adverse effects associated with oral naltrexone administration. Similarly, the ability to maintain therapeutically relevant plasma levels of naltrexone continuously should provide for a more uniform occupation of opioid receptors, and therefore, a more consistent pharmacodynamic response throughout the course of treatment. Finally, adherence would be assured for an entire month after each injection, providing yet another important advantage.
Owing to these potential advantages, we formulated naltrexone into PLG-microspheres using Alkermes' proprietary Medisorb® technology to provide a product intended to deliver therapeutic levels of naltrexone for a full month following each injection. The following experiments describe preclinical pharmacokinetic and pharmacodynamic results from such an extended-release microsphere formulation of naltrexone (ie Vivitrex®), demonstrating that it provides plasma concentrations of naltrexone that are consistently elevated above therapeutic levels for approximately a 1-month period following each injection. Moreover, the plasma levels of naltrexone show a close, temporal correlation with a sustained pharmacodynamic response (morphine-induced analgesia as measured in the hot-plate test) that reflects an effective opioid receptor blockade.
MATERIALS AND METHODS
Subjects
Male Sprague–Dawley rats (450±50 g; Taconic Farms, Germantown, NY) were used in all studies. Rats were pair-housed in polypropylene cages with free access to food and water. The vivarium was maintained on a 12 h light : dark cycle with a room temperature of 22±1°C and relative humidity level of 50±5%. All studies were approved by Alkermes Institutional Animal Care and Use Committee and were conducted in adherence with the NIH ‘Guide for the Care and Use of Laboratory Animals, 1996'.
Drug Treatments and Experimental Design
Naltrexone-containing microspheres (Vivitrex®) were fabricated from the PLG polymer using a proprietary process (Lewis, 1990) to provide loading densities of approximately 35% (w/w) naltrexone base. Placebo (nonloaded) microspheres were prepared in an identical manner, except that naltrexone was omitted.
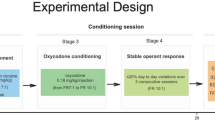
Microspheres were suspended in 1 ml of an aqueous diluent (0.9% saline, 0.1% Tween-20 and 3.0% low-viscosity carboxymethylcellulose) and injected using a 22 G needle to provide a total of 50 mg/kg naltrexone, or a comparable mass of placebo microspheres. In the first series of experiments, animals received either a subcutaneous (s.c.) or intramuscular (i.m.) injection of placebo or naltrexone-loaded microspheres. Animals received an intraperitoneal (i.p.) injection of morphine (1 mg/kg) or saline 1, 3, 7, 14, 21, 28, and 35 days after microsphere administration and were retested on the hot plate 30 min after each morphine injection.
Rats receiving i.m. injections were also used in studies further exploring the relationships between extended-release naltrexone, morphine antagonism, and changes in brain μ-opioid receptor binding and immunoreactivity. Half of the animals receiving extended-release naltrexone i.m. were killed 36 days after injection, a time when the behavioral effects of naltrexone were diminished. The placebo and remaining extended-release naltrexone-treated animals received a second, identical microsphere injection 34 days after the first. These animals were retested on the hot plate 1, 7, 14, 21, 28, 30, 32, 34, and 36 days later and were sacrificed on day 37, a time when the pharmacodynamic effects of naltrexone had completely disappeared.
Injections of extended-release naltrexone or placebo were well tolerated by the rats, independent of the route or number of injections. This was evidenced by the absence of local site reactions (redness, swelling, exudation, or skin scratching) upon clinical examination, both in vivo and ex vivo. Body weights of rats receiving extended release naltrexone and placebo microspheres were measured weekly for 35 days. The body weight of extended-release naltrexone-treated rats was 2.8±0.27% lower than placebo-treated rats over this period (P<0.01, two-way ANOVA).
Quantitation of Plasma Levels of Naltrexone
Blood samples were collected from all animals immediately after each behavioral test (see below). Animals were briefly anesthetized with 1–2% isoflurane and blood samples (approximately 500 μl of whole blood) were collected via a lateral tail vein into tubes containing EDTA. The tubes were centrifuged for 10 min at 1000 g to separate plasma, which was subsequently stored at −70°C until levels of naltrexone were determined by LC-MS (Naidong et al, 2002). The lower limit of quantitation (LOQ) for these studies was 1.0 ng/ml, and the coefficient of variation for the assay was <4.4%.
Hot-Plate Testing
Morphine-induced (1 mg/kg) analgesia was used to determine the ability of extended-release naltrexone to block opioid receptors in the central nervous system. Analgesia was monitored using a commercially available hot-plate apparatus (Columbus Instruments, Columbus, OH). Rats were individually placed on the hot plate (surface temperature=48°C) and the latency (60 s maximum) to lick either hind paw was recorded. Animals received two baseline trials on the hot-plate test and were then randomly assigned to treatment groups. The effect of placebo or extended-release naltrexone formulations on morphine-induced analgesia was assessed on the indicated days after injection by administering morphine, starting at 1000 h. Each rat was tested on the hot plate 20 min after morphine injection, and then returned to its cage. The testing order was randomized over the course of the investigation.
μ-Opioid Receptor Changes Following Administration of Extended-Release Naltrexone to Rats
Increases in μ-opioid receptor density are commonly observed in response to antagonist administration (Lahti and Collins, 1978; Zukin et al, 1982). Therefore, the status of μ-opioid receptor density following the administration of an extended-release naltrexone preparation was investigated as a biochemical measure of pharmacodynamic efficacy. The time course of the changes in μ-opioid receptor density and expression following the administration of extended-release naltrexone microspheres was investigated using two different radioligand binding assays and immunohistochemical techniques. For the saturation radioligand binding assays, male Sprague–Dawley rats were injected once i.m. with 79.2 mg of microspheres (placebo or naltrexone, approximately 50 mg/kg naltrexone) suspended in 0.75 ml of diluent. The rats were then killed 3, 5, 7, 28, 30, 32, 36, or 40 days after naltrexone, and 3, 7, 38, or 40 days after placebo administration. The brains were rapidly removed, placed in isotonic sucrose (0–4°C), the cortex, midbrain (from approximately bregma −5 to −10 mm), and striatum dissected free on ice, rapidly frozen on dry ice, and stored at −80°C until use. For autoradiographic and immunohistochemical studies, rats were injected twice with extended-release naltrexone (see above).
μ-Opioid receptor binding
[3H]DAMGO (D-ala2, N-methyl-phe4, glycol5) enkephalin; specific activity=55.0 Ci/mmol; Amersham Pharmacia Biotech, Arlington Heights, IL) binding to μ-opioid receptors in the midbrain, striatum, and cortex was performed using a modification of a previously described technique (Goldstein and Naidu, 1989). At the time of the assay, these regions were homogenized using a probe sonicator in 10 vol of 50 mM Tris-HCl, 1 mM EDTA, and 280 mM sucrose buffer, pH 7.4, then centrifuged at 20 000 g for 20 min. The pellet was retained and resuspended in 50 mM Tris-HCl pH 7.4 buffer alone and then recentrifuged. The latter step was repeated a total of four times.
The equilibrium binding constants (Kd and Bmax) for [3H]DAMGO binding to μ receptors in brain homogenates were determined using saturation binding assays consisting of 0.5–10 nM concentrations of [3H]DAMGO, tissue (0.08–0.7 mg protein), 10 μM naltrexone (for determination of nonspecific binding), and sufficient 50 mM Tris-HCl buffer to yield a final volume of 250 μl. The assays were performed in duplicate in polystyrene 96-well plates incubated at 25°C for 1 h, and terminated by filtration. The Bmax and Kd values were determined by nonlinear regression fitting of saturation isotherms to the data (Prism, GraphPad Software, San Diego, CA).
μ-Opioid receptor autoradiography
At the conclusion of behavioral testing (see above), animals were killed, their brains removed, flash frozen, and stored at −80°C. Frozen brains were cut into 20 μm thick sections using a cryostat, the sections thaw-mounted onto glass slides, and stored at −80°C until they were used for quantitative autoradiography of μ-opioid receptor binding (Morris et al, 2001). Brain sections were prewashed in 120 mM NaCl and 50 mM Tris-HCl buffer, then incubated in a solution containing 5 nM [3H]DAMGO and 120 mM NaCl in Tris-HCl buffer (pH 7.4, 1 h, 25°C). Nonspecific binding was determined using 1 μM DAMGO. At the end of the incubation period, the sections were washed 5 × 1 min in Tris buffer (pH 7.4, 0–4°C) with a final rinse in distilled H2O (0–4°C), then dried under a cool stream of air. The sections were apposed to film (Hyperfilm-3H; Amersham Pharmacia Biotech), together with a tritium standard calibration slide (American Radiolabeled Chemicals, St Louis, MO) and nonspecific control sections. The films were stored at −80°C and developed 9 weeks later. The optical density of autoradiographic exposures was quantified using an MCID 4 image analysis system (Imaging Research, St Catherines, Ontario, Canada).
μ-Opioid receptor immunoreactivity
Brain sections adjacent to those used for receptor binding were processed for μ-opioid receptor immunoreactivity (Unterwald et al, 1998). Sections were immersion fixed in 6% paraformaldehyde, 20% sucrose, 20% ethanol, 20% ethylene glycol, and 10% glycerol in 0.05 M phosphate buffer (Jones et al, 1992), then washed in phosphate-buffered saline. Subsequently, the sections were treated to suppress endogenous peroxidase activity and the nonspecific sites were blocked. The slides were then incubated with the primary antibody to μ-opioid receptors (Ab-1, Oncogene Research Products, Cambridge, MA; 1 : 2500) in a humidifying chamber for 24 h. The next day, the slides were washed and incubated for 2 h with the secondary antibody (I125 anti-rabbit IgG; Amersham Biosciences, Piscataway, NJ, 1 : 100) in the humidifying chamber. The sections were then washed and dried under a stream of cool air. Nonspecific immunoreactivity was assessed by deleting either the primary antibody or using sections treated with antibody preabsorbed to the antigenic peptide (Opioid μ-Receptor Control Peptide, Oncogene). These sections, together with an I125 microscale standard (Amersham Biosciences), were apposed to film (Hyperfilm-ßmax, Amersham Biosciences) for 7 days. The films were developed and the autoradiographs analyzed using the MCID 4 image analysis system.
RESULTS
Quantitation of Plasma Levels of Naltrexone in Rats
Plasma naltrexone levels were below the LOQ in all rats tested prior to treatment. The route of administration (i.m. or s.c.) had no significant effect on either the plasma naltrexone levels (P=0.72, two-way ANOVA, Figure 1a and Figure 2a), or the area under the curves (332 vs 360 ng day/ml, i.m. vs s.c., respectively). However, plasma naltrexone concentrations changed significantly with time (P<0.01, Two-way ANOVA), increasing to approximately one-half of the maximum within 24 h of injection, with maximum levels (15±1.4 and 19±3.6 ng/ml, s.c. and i.m., respectively) observed by 3 days. Plasma concentrations of naltrexone did not differ significantly from each other between 3 and 14 days (i.m.) or 21 days (s.c.) postinjection, with detectable levels of naltrexone maintained to 35 days. A similar pattern was observed in animals that received a second i.m. injection of extended-release naltrexone microspheres (Figure 2a, Rx 2). There were no significant differences in plasma naltrexone levels during the plateau phase between the first and second injections. Moreover, naltrexone was no longer quantifiable in the plasma (<1 ng/ml) 35 days after the second injection.
(a) Plasma levels of naltrexone in rats following a single, s.c. injection of extended-release naltrexone microspheres (50 mg/kg naltrexone). Blood was sampled from the tail vein immediately after the hot-plate test. Note that the plasma levels of naltrexone were maintained for 21 days and were above the LOQs for at least 28 days. Each point represents the mean±SEM of plasma naltrexone concentrations (ng/ml) from eight rats. (b) Pharmacodynamic effects of a single s.c. injection of extended-release naltrexone microspheres. This was assessed by testing naltrexone (circles) or placebo formulation (squares)-treated rats on the hot plate 30 min after an injection of morphine (1 mg/kg i.p., closed symbols) or saline (open symbols). Rats receiving placebo microspheres manifested a pronounced analgesic response to morphine that consistently approached the maximum latency of 60 s. In contrast, animals pretreated with naltrexone microspheres showed substantial block of morphine analgesia, responding at or near the level of saline-treated animals. Data represent the mean±SEM of the latency to lick a hind paw measured in eight rats. **Performance of the naltrexone+morphine group is significantly different from placebo+morphine, placebo+saline, and naltrexone+saline groups, P<0.01, two-way ANOVA followed by Tukey's post hoc analysis. (a) Performance of the naltrexone+morphine group is significantly different from placebo+morphine and placebo+saline groups, P<0.01, two-way ANOVA followed by Tukey's post hoc analysis. (b) Performance of the naltrexone+morphine group is significantly different from placebo+saline and naltrexone+Saline GROUPS, P<0.01, two-way ANOVA followed by Tukey's post hoc analysis. B: baseline conditions.
(a) Plasma levels of naltrexone in rats following either a single i.m. injection of extended-release microspheres (open circles) or a second, identical injection 34 days following the first treatment (closed circles). Plasma levels of naltrexone were maintained for approximately 21 days following a single injection, an effect that was repeated with a second injection after an additional 34 days. Each point represents the mean±SEM naltrexone plasma concentration (ng/ml) from nine rats. LOQ: lower limit of quantitation (<1 ng/ml). (b) Analgesic actions of morphine (1 mg/kg i.p.) following either one or two i.m. injections of extended-release naltrexone microspheres in rats as tested on the hot plate. Naltrexone, whether administered for 1 or 2 months i.m., was capable of antagonizing morphine-induced analgesia, with responses equivalent to those observed under baseline conditions. The analgesic actions of morphine in rats treated once with naltrexone increased to levels observed in the placebo+morphine by 41 days. In contrast, two naltrexone treatments consistently suppressed morphine-induced analgesia for a total of 68 days. Data represent the mean±SEM of latency to lick a hind paw by nine rats. **Performance of the naltrexone+morphine, 1 or 2 months groups, are significantly different from the placebo+morphine group, P<0.01, two-way ANOVA followed by Tukey's post hoc analysis. (a) Performance of the naltrexone+morphine 1 month group is significantly different from the naltrexone+morphine 2 months group, P<0.01, two-way ANOVA followed by Tukey's post hoc analysis. B: Baseline conditions. Rx 1, 2: Times of first and second naltrexone injections.
Hot-Plate Testing
The pharmacodynamic effects of extended-release naltrexone corresponded well with the pharmacokinetic profile derived from the same animals. Extended-release naltrexone significantly suppressed the analgesia produced by morphine, independent of the route of microsphere administration (Treatment Effect, P<0.01, Route Effect, P=0.35, Multiway ANOVA, Figure 1b and Figure 2b). Morphine induced a profound analgesia in rats receiving placebo microspheres, as evidenced by hot-plate times approaching the maximum duration (57±0.60 s). In contrast, the analgesic effects of morphine were suppressed in rats previously administered extended-release naltrexone (Figure 1b and Figure 2b). Over a 21-day period, the rats receiving extended-release naltrexone+morphine showed hot-plate response times (40±0.54 s) that were approximately 70% of the level of those that received extended release placebo+saline (34±0.80 s). After 28 days, the morphine-associated response latencies of the extended-release naltrexone-treated rats increased to the level of those rats receiving placebo microspheres (59±0.84 vs 57±1.8 s, placebo+morphine vs naltrexone+morphine). Rats receiving extended-release naltrexone i.m. had hot-plate response times after morphine treatment (36±0.40 s) that were statistically indistinguishable from saline-treated animals (eg placebo+saline=31±5.1 s; naltrexone+saline= 34±3.5 s). Animals receiving a second i.m. injection of extended-release naltrexone on day 34 continued to exhibit complete antagonism of the analgesic effects of morphine throughout the second month (36 s, Figure 2b). The analgesic effects of morphine on naltrexone-treated rats reverted to the level of the placebo-treated rats (59±0.48 vs 59±0.58 s, placebo+morphine vs naltrexone+morphine) by 35 days after treatment (Figure 2b).
Opioid Receptor Changes Following Extended-Release Naltrexone in Rats
Radioligand binding assays
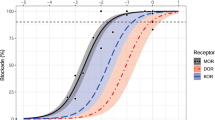
Saturation binding assays revealed that the Bmax for [3H]DAMGO binding to the midbrain and the striatum was significantly increased (110 and 110% vs placebo treatment, P<0.01, 0.05, respectively, ANOVA followed by Tukey's post hoc comparison test) by 1 week after administration of extended-release naltrexone (Figures 3b, c). Evidence of increased μ-opioid receptor density was observed as early as 5 days after administration. These increases in receptor density were sustained throughout the subsequent 33 days, at least 1 week after the significant decline in pharmacodynamic effectiveness of the extended-release preparation. Interestingly, the density of cortical μ-opioid receptors did not begin to increase until 30 days after extended-release naltrexone administration (Figure 3a), reaching significance at 40 days (120% increase vs placebo, P<0.01, ANOVA followed by Tukey's post hoc comparison test). No significant changes in radioligand affinity for the receptors were observed in any brain region at any time, regardless of treatment (cortex: 7.1±0.40; midbrain: 4.2±0.30; striatum: 3.1±0.10 nM).
Regional changes in the Bmax of [3H]DAMGO binding to μ-opioid receptors in the brain following a single i.m. dose of extended-release naltrexone. Data represent the mean±SEM of data from eight rats (panels a, b) or eight sets of striata pooled from 16 rats (panel c). Significant increases in the density of μ receptors in the cerebral cortex were not observed until 32 (relative to t0 control) to 40 (relative to contemporaneous placebo control) days after naltrexone administration (panel a). In contrast, μ-opioid receptor density in the midbrain (panel b) and striatum (panel c) was significantly increased by 7 days (relative to contemporaneous placebo) after naltrexone administration. (a) Significantly different from t0 control, P<0.05; *, **significantly different from contemporaneous placebo control, P<0.05, 0.01, two-way ANOVA followed by Tukey's post hoc comparison matrix.
Similar results, albeit with higher regional resolution, were obtained using radioligand binding autoradiography. In this study, rats received either one or two injections of extended-release naltrexone spaced 34 days apart, and the changes in μ-opioid receptor density quantified at 1 month and 24 h after the antagonism of morphine's analgesic effects had dissipated (ie 2 months from initial injection). Autoradiography revealed that radioligand binding to μ-opioid receptors was significantly increased above control in all brain regions examined, ranging from 90% in the habenular nucleus to 160% in the dorsal raphe nucleus (Table 1, Figure 4) after 1 month. In most regions, these densities continued to increase at 2 months, from 100% in the subiculum to 220% in the dorsal raphe.
Representative photomicrographs of brain sections incubated with [3H]DAMGO from rats receiving i.m. injections of either naltrexone-containing or placebo microspheres for approximately 2 months (see text for details). Note the marked increase in the density of μ-opioid receptor binding in the prefrontal cortex, striatum, thalamus, hippocampus, and superior colliculus in those animals receiving extended-release naltrexone relative to rats receiving placebo microspheres. See Table 1 for quantitative data.
Immunohistochemistry
Immunohistochemistry using brain sections adjacent to those used in the radioligand autoradiography also revealed significantly increased μ-opioid receptor immunoreactivity (Table 2, Figure 5). After 1 month of treatment with extended-release naltrexone, immunoreactivity was significantly increased above control levels in only two of 15 brain regions studied, including the nucleus accumbens (20%) and the substantia nigra (20%, Table 2). Following 2 months of treatment, increased immunoreactivity over placebo controls was observed in 14 of 15 brain regions examined. However, the magnitude of these increases was lower than those observed with radioligand receptor binding, ranging from 10% in the perirhinal cortex to 40% in the substantia nigra (Table 2).
Representative photomicrographs of brain sections processed for immunohistochemical visualization of opioid receptors using a radiolabeled secondary antibody for autoradiographic quantitation. Brain sections adjacent to those described above for binding studies (Figure 4) were used. The regions showing increased opioid receptor immunoreactivity following naltrexone treatment (ie striatum, hypothalamus, hippocampus, and superior colliculus) were similar to those observed using radioligand autoradiography. However, the amplitude of the elevations was less robust than the increases in receptor density determined by radioligand binding assays. See Table 2 for quantitative data.
DISCUSSION
Naltrexone has repeatedly been shown to be effective in suppressing a number of indices of ethanol consumption in animal models, including decreasing ad libitum (Altshuler et al, 1980; Davidson and Amit, 1997; Boyle et al, 1998) and limited access (Stromberg et al, 1998) ethanol intake, while delaying the acquisition of voluntary ethanol consumption (Davidson and Amit, 1997). Moreover, naltrexone has been shown to be effective in several human studies in reducing alcohol consumption and relapse to heavy drinking when combined with psychosocial treatment (Garbutt et al, 1999; O'Malley et al, 1992; Volpicelli et al, 1992). Nonetheless, the efficacy of naltrexone in treating alcohol dependence has not been consistent between studies (eg Krystal et al, 2001). This variability in treatment effect is likely related, in part, to issues of patient adherence (Volpicelli et al, 1997). Significant effort is required to maintain an alcoholic patient on the daily, oral dose regimen of naltrexone rigorously for the several months required to achieve maximal efficacy (O'Malley et al, 1996). Additional deficiencies and variability in oral naltrexone's effects likely result from its suboptimal pharmacokinetic profile. This profile is characterized by transiently high plasma levels within 4 h after each oral dose, followed by concentration troughs at 8–10 h after administration that persist until the next dose is taken the following day. Additional deficiencies with oral naltrexone include substantial first-pass metabolism (Verebey, 1980; Wall et al, 1981; Reuning et al, 1989) and adverse effects (eg nausea, vomiting) likely associated with the blockade of μ-opioid receptors in the gut (Croop et al, 1997). For these reasons, a parenteral, extended-release formulation of naltrexone would be of great utility in the treatment of alcohol and opiate dependence.
The idea of developing an extended-release formulation of naltrexone is not novel, and several attempts have been made to produce such a preparation over the past two decades. To date, none of these formulations have shown clear evidence of clinical success, for reasons including inconsistent initial and sustained release rates (Chiang et al, 1984; Kranzler et al, 1998), inadequate duration of release, suboptimal physical characteristics (dose size/volume, naltrexone loading), and local site reactions (Macgregor et al, 1983; Misra and Pontani, 1981; Reuning et al, 1981). The limited success achieved by these seminal efforts nonetheless emphasizes both the importance of clearly specifying the characteristics required of a successful formulation, as well as the technical difficulties of achieving these characteristics. Therefore, to develop an acceptable and effective sustained-release formulation of naltrexone, it must: be impervious to patient manipulation; rapidly achieve plasma levels above the minimum therapeutic range (>2 ng/ml, Verebey, 1980); maintain these levels for approximately 1 month following each injection; be easily administered; and be well tolerated with no serious reactions at the injection site. We now report on the pharmacokinetic and pharmacodynamic performance of an extended-release preparation of naltrexone (Vivitrex®) in a rat model that meets these criteria and should be applicable to clinical use.
Naltrexone was formulated into PLG copolymer microspheres. This matrix has been extensively used in implantable materials and causes little local inflammatory response (Sanders et al, 1986; Johnson et al, 1996; Shive and Anderson, 1997). The release of naltrexone from the PLG matrix, as indicated by plasma naltrexone concentrations, was relatively independent of the route of administration (ie s.c. vs i.m.). The peak plasma levels (15–19 ng/ml) reached by day 3 were approximately 40% higher than the sustained plasma concentrations of 12 ng/ml, which were observed by 8 days after administration. Plasma naltrexone levels were consistently maintained at this level for the following 14 days, and at pharmacologically relevant levels (>2 ng/ml, Kranzler et al, 1998; Lee et al, 1988; Verebey, 1980) for a full month. Administering a second dose of the formulation resulted in similar plasma levels over the same time frame, suggesting that there was no enhancement of metabolic clearance of naltrexone.
Given the involvement of endogenous opioid pathways in the mediation of reinforcement in substance abuse, we used the blockade of morphine-induced supraspinal analgesia as measured in the hot-plate test as a surrogate, pharmacodynamic index of the ability of the extended release naltrexone preparation to block these pathways. The plasma naltrexone levels established by this preparation were sufficient to inhibit the analgesic actions of morphine fully for 1 month following each injection. The extent of inhibition of morphine analgesia was closely correlated with the plasma levels of naltrexone, which fell below the LOQs (<1 ng/ml) by 34 days. However, full inhibition of morphine analgesia could be retained for an additional month by administration of a second dose of extended-release naltrexone.
A compensatory increase in μ-opioid receptor density is commonly observed following the chronic administration of opioid receptor antagonists (Lahti and Collins, 1978; Morris et al, 1988; Overstreet et al, 1999), including naltrexone (Zukin et al, 1982; Bardo et al, 1982; Yoburn et al, 1989). Moreover, the elevation in μ-opioid receptors is observed regardless of whether naltrexone is administered orally (Parkes and Sinclair, 2000) or parenterally (Zukin et al, 1982; Yoburn et al, 1989; Giordano et al, 1990). Therefore, we monitored the status of μ-opioid receptor density following administration of our extended-release naltrexone formulation as a biochemical index of pharmacodynamic efficacy. Consistent with previous observations, a significant, two- to three-fold elevation in the density of μ-opioid receptors was observed in several brain regions following administration of extended-release naltrexone. [3H]DAMGO binding to μ-opioid receptors was significantly increased in the midbrain and striatum after 7 days of naltrexone administration, and was maintained for at least an additional week after plasma naltrexone levels fell below the levels of quantitation. This may reflect a slow rate of elimination of naltrexone that had accumulated in the brain (Taylor et al, 1980; Verebey, 1980) or the long residency of naltrexone at the μ-opioid receptor (Lee et al, 1988). However, it probably does not reflect a substantial activation of μ-opioid receptor protein expression, as indicated by the relatively small increase in μ-opioid receptor immunoreactivity observed only after two courses of extended-release naltrexone administration. While the mechanisms responsible for the lack of correlation between the increase in density of μ-opioid receptor binding sites and immunoreactivity are not clear, this phenomenon has been previously observed (Unterwald et al, 1995, 1998; Castelli et al, 1997). The cumulative results suggest that the increase in μ-opioid receptor density is not regulated at the transcriptional level, but reflects recruitment of active μ-opioid receptors from a pool of spare, sequestered receptors in response to the presence of antagonists.
Overall, the degree of increase in μ-opioid receptor density is comparable to that previously reported following long-term naltrexone administration (⩾28 D, Giordano et al, 1990), and did not appear to compromise the efficacy of naltrexone in blocking morphine analgesia (Yoburn et al, 1989). This was supported by the lack of decrease in the intensity of suppression of morphine analgesia over the period of maximally increased receptor density (34 days postadministration). While hypersensitivity to morphine analgesia may result from chronic naltrexone administration (Zukin et al, 1982; Yoburn et al, 1995), naltrexone-induced increases in opioid receptor density do not enhance sensitivity to opiate-induced respiratory depression (Cornish et al, 1993) and tolerance to suppression of opiate-induced euphoria does not occur (Kleber et al, 1985).
In summary, the Vivitrex® formulation of extended release naltrexone maintains stable, pharmacologically relevant plasma levels of naltrexone for at least 28 days. Given that both naltrexone (Croop et al, 1997; Lin, 1994) and the PLG polymer matrix in which it is encapsulated (Shive and Anderson, 1997) show little systemic toxicity and are well tolerated locally, Vivitrex® should prove safe and effective in the treatment of both alcohol and opiate dependence by providing a superior means for maintaining elevated plasma levels of naltrexone.
References
Altshuler HL, Phillips PE, Feinhandler DA (1980). Alteration of ethanol self-administration by naltrexone. Life Sci 26: 679–688.
Bardo MT, Bhatnagar RK, Gebhart GF (1982). Differential effects of chronic morphine and naloxone on opiate receptors, monoamines and morphine-induced behaviors in preweanling rats. Brain Res 255: 139–147.
Boyle AE, Stewart RB, Macenski MJ, Spiga R, Johnson BA, Meisch RA (1998). Effects of acute and chronic doses of naltrexone on ethanol self-administration in rhesus monkeys. Alcohol Clin Exp Res 22: 359–366.
Capone T, Brahen L, Condren R, Kordal N, Melchionda R, Peterson M (1986). Retention and outcome in a narcotic antagonist treatment program. J Clin Psychol 42: 825–833.
Castelli MP, Melis M, Mameli M, Fadda P, Diaz G, Gessa GL (1997). Chronic morphine and naltrexone fail to modify mu-opioid receptor mRNA levels in the rat brain. Brain Res Mol Brain Res 45: 149–153.
Chiang CN, Hollister LE, Kishimoto A, Barnett G (1984). Kinetics of a naltrexone sustained-release preparation. Clin Pharmacol Ther 36: 704–708.
Cornish JW, Henson D, Levine S, Volpicelli J, Inturrisi CE, Yoburn BC et al (1993). Naltrexone maintenance: effect on morphine sensitivity in normal volunteers. Am J Addict 2: 34–38.
Croop RS, Faulkner EB, Labriola DF (1997). The safety profile of naltrexone in the treatment of alcoholism. Results from a multicenter usage study. The Naltrexone Usage Study Group. Arch Gen Psychiatry 54: 1130–1135.
Davidson D, Amit Z (1997). Naltrexone blocks acquisition of voluntary ethanol intake in rats. Alcohol Clin Exp Res 21: 677–683.
D'Ippoliti D, Davoli M, Perucci CA, Pasqualini F, Bargagli AM (1998). Retention in treatment of heroin users in Italy: the role of treatment type and of methadone maintenance dosage. Drug Alcohol Depend 52: 167–171.
Food and Drug Administration, New Drug Application (1994). Trexan (Naltrexone Tablets) NDA 18-932/S-010, December 30.
Garbutt JC, West SL, Carey TS, Lohr KN, Crews FT (1999). Pharmacological treatment of alcohol dependence: a review of the evidence. JAMA 281: 1318–1325.
Giordano AL, Nock B, Cicero TJ (1990). Antagonist-induced up-regulation of the putative Epsilon opioid receptor in rat brain: comparison with Kappa, Mu and Delta opioid receptors. J Pharmacol Exp Ther 255: 536–540.
Goldstein A, Naidu A (1989). Multiple opioid receptors: ligand selectivity profiles and binding site signatures. Mol Pharmacol 36: 265–272.
Grant BF (1997). Prevalence and correlates of alcohol use and DSM-IV alcohol dependence in the United States: results of the National Longitudinal Alcohol Epidemiologic Survey. J Stud Alcohol 58: 464–473.
Greenstein RA, Arndt IC, McLellan AT, O'Brien CP, Evans B (1984). Naltrexone: a clinical perspective. J Clin Psychiatry 45: 25–28.
Herz A (1997). Endogenous opioid systems and alcohol addiction. Psychopharmacology (Berl) 129: 99–111.
Johnson OL, Cleland JL, Lee HJ, Charnis M, Duenas E, Jaworowicz W et al (1996). A month-long effect from a single injection of microencapsulated human growth hormone. Nat Med 2: 795–799.
Jones EG, Hendry SH, Liu XB, Hodgins S, Potkin SG, Tourtellotte WW (1992). A method for fixation of previously fresh-frozen human adult and fetal brains that preserves histological quality and immunoreactivity. J Neurosci Methods 44: 133–144.
King AC, Volpicelli JR, Gunduz M, O'Brien CP, Kreek MJ (1997). Naltrexone biotransformation and incidence of subjective side effects: a preliminary study. Alcohol Clin Exp Res 21: 906–909.
Kleber HD, Kosten TR, Gaspari J, Topazian M (1985). Nontolerance to the opioid antagonism of naltrexone. Biol Psychiatry 20: 66–72.
Kranzler HR, Modesto-Lowe V, Nuwayser ES (1998). Sustained-release naltrexone for alcoholism treatment: a preliminary study. Alcohol Clin Exp Res 22: 1074–1079.
Krystal JH, Cramer JA, Krol WF, Kirk GF, Rosenheck RA (2001). Naltrexone in the treatment of alcohol dependence. N Engl J Med 345: 1734–1739.
Lahti RA, Collins RJ (1978). Chronic naloxone results in prolonged increases in opiate binding sites in brain. Eur J Pharmacol 51: 185–186.
Lee MC, Wagner HN, Tanada S, Frost JJ, Bice AN, Dannals RF (1988). Duration of occupancy of opiate receptors by naltrexone. J Nucl Med 29: 1207–1211.
Lewis DH (1990). Controlled release of bioactive agents from lactide/glycolide polymers. In: Chasin M, Langer R (eds) Biodegradable Polymers as Drug Delivery Systems pp 1–41.
Lin G (1994). Reviewer's report, FDA re-evaluation of carcinogenicity studies for naltrexone hydrochloride (Trexan). NDA 18-932.
Litten RZ, Allen JP (1998). Advances in development of medications for alcoholism treatment. Psychopharmacology (Berl) 139: 20–33.
Macgregor TR, Drum MA, Harrigan SE, Wiley JN, Reuning RH (1983). Naltrexone metabolism and sustained release following administration of an insoluble complex to rhesus monkeys and guinea-pigs. J Pharm Pharmacol 35: 38–42.
Martin WR, Jasinski DR, Mansky PA (1973). Naltrexone, an antagonist for the treatment of heroin dependence. Effects in man. Arch Gen Psychiatry 28: 784–791.
Misra AL, Pontani RB (1981). An improved long-acting delivery system for narcotic antagonists. NIDA Res Monogr 28: 254–264.
Morris BJ, Millan MJ, Herz A (1988). Antagonist-induced opioid receptor up-regulation, II. Regionally specific modulation of mu, delta and kappa binding sites in rat brain revealed by quantitative autoradiography. J Pharmacol Exp Ther 247: 729–736.
Morris PL, Hopwood M, Whelan G, Gardiner J, Drummond E (2001). Naltrexone for alcohol dependence: a randomized controlled trial. Addiction 96: 1565–1573.
Naidong W, Bu H, Chen YL, Shou WZ, Jiang X, Halls TD (2002). Simultaneous development of six LC-MS-MS methods for the determination of multiple analytes in human plasma. J Pharm Biomed Anal 28: 1115–1126.
O'Malley SS, Jaffe AJ, Chang G, Rode S, Schottenfeld R, Meyer RE et al (1996). Six-month follow-up of naltrexone and psychotherapy for alcohol dependence. Arch Gen Psychiatry 53: 217–224.
O'Malley SS, Jaffe AJ, Chang G, Schottenfeld RS, Meyer RE, Rounsaville B (1992). Naltrexone and coping skills therapy for alcohol dependence. A controlled study. Arch Gen Psychiatry 49: 881–887.
Overstreet DH, Kampov-Polevoy AB, Rezvani AH, Braun C, Bartus RT, Crews FT (1999). Suppression of alcohol intake by chronic naloxone treatment in P rats: tolerance development and elevation of opiate receptor binding. Alcohol Clin Exp Res 23: 1761–1771.
Parkes JH, Sinclair JD (2000). Reduction of alcohol drinking and upregulation of opioid receptors by oral naltrexone in AA rats. Alcohol 21: 215–221.
Resnick RB, Volavka J, Freedman AM, Thomas M (1974). Studies of EN-1639A (naltrexone): a new narcotic antagonist. Am J Psychiatry 131: 646–650.
Reuning RH, Ashcraft SB, Wiley JN, Morrison BE (1989). Disposition and pharmacokinetics of naltrexone after intravenous and oral administration in rhesus monkeys. Drug Metab Dispos 17: 583–589.
Reuning RH, Liao SH, Staubus AE (1981). Pharmacokinetic quantitation of naltrexone release from several sustained-release delivery systems. NIDA Res Monogr 28: 172–184.
Sanders LM, Kell BA, McRae GI, Whitehead GW (1986). Prolonged controlled-release of nafarelin, a luteinizing hormone-releasing hormone analogue, from biodegradable polymeric implants: influence of composition and molecular weight of polymer. J Pharm Sci 75: 356–360.
Shive MS, Anderson JM (1997). Biodegradation and biocompatibility of PLA and PLGA microspheres. Adv Drug Deliv Rev 28: 5–24.
Spanagel R, Herz A, Shippenberg TS (1992). Opposing tonically active endogenous opioid systems modulate the mesolimbic dopaminergic pathway. Proc Natl Acad Sci USA 89: 2046–2050.
Stromberg MF, Volpicelli JR, O'Brien CP (1998). Effects of naltrexone administered repeatedly across 30 or 60 days on ethanol consumption using a limited access procedure in the rat. Alcohol Clin Exp Res 22: 2186–2191.
Taylor SM, Rodgers RM, Lynn RK, Gerber N (1980). The seminal excretion, plasma elimination, tissue distribution and metabolism of naltrexone in the rabbit. J Pharmacol Exp Ther 213: 289–299.
Unterwald EM, Anton B, To T, Lam H, Evans CJ (1998). Quantitative immunolocalization of mu opioid receptors: regulation by naltrexone. Neuroscience 85: 897–905.
Unterwald EM, Rubenfeld JM, Imai Y, Wang JB, Uhl GR, Kreek MJ (1995). Chronic opioid antagonist administration upregulates mu opioid receptor binding without altering mu opioid receptor mRNA levels. Brain Res Mol Brain Res 33: 351–355.
Verebey K (1980). The clinical pharmacology of naltrexone: pharmacology and pharmacodynamics. NIDA Res Monogr 28: 147–158.
Volpicelli JR, Alterman AI, Hayashida M, O'Brien CP (1992). Naltrexone in the treatment of alcohol dependence. Arch Gen Psychiatry 49: 876–880.
Volpicelli JR, Rhines KC, Rhines JS, Volpicelli LA, Alterman AI, O'Brien CP (1997). Naltrexone and alcohol dependence. Role of subject compliance. Arch Gen Psychiatry 54: 737–742.
Wall ME, Brine DR, Perez-Reyes M (1981). Metabolism and disposition of naltrexone in man after oral and intravenous administration. Drug Metab Dispos 9: 369–375.
Yoburn BC, Sierra V, Lutfy K (1989). Chronic opioid antagonist treatment: assessment of receptor upregulation. Eur J Pharmacol 170: 193–200.
Yoburn BC, Shah S, Chan K, Duttaroy A, Davis T (1995). Supersensitivity to opioid analgesics following chronic opioid antagonist treatment: relationship to receptor selectivity. Pharmacol Biochem Behav 51: 535–539.
Zukin RS, Sugarman JR, Fitz-Syage ML, Gardner EL, Zukin SR, Gintzler AR (1982). Naltrexone-induced opiate receptor supersensitivity. Brain Res 245: 285–292.
Acknowledgements
This work was produced as part of the duties of employees of Alkermes, Inc.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bartus, R., Emerich, D., Hotz, J. et al. Vivitrex®, an Injectable, Extended-Release Formulation of Naltrexone, Provides Pharmacokinetic and Pharmacodynamic Evidence of Efficacy for 1 Month in Rats. Neuropsychopharmacol 28, 1973–1982 (2003). https://doi.org/10.1038/sj.npp.1300274
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.npp.1300274
Keywords
This article is cited by
-
Nanoparticle delivery systems for substance use disorder
Neuropsychopharmacology (2022)
-
Extended-Release Intramuscular Naltrexone (VIVITROL®): A Review of Its Use in the Prevention of Relapse to Opioid Dependence in Detoxified Patients
CNS Drugs (2013)
-
Studies of 3-O-acyl derivatives of naloxone as its potential prodrugs
Chemistry of Heterocyclic Compounds (2009)