Abstract
Over the past 15 years, we have witnessed a resurgence of surgery for prevention of ischemic stroke. Landmark trials including the North American Symptomatic Carotid Endarterectomy Trial and the European Carotid Surgery Trial have explored the role of carotid endarterectomy in this context, comparing the procedure with best medical treatment in patients with high-grade stenosis of the internal carotid artery and transient ischemic attack or minor nondisabling stroke in the same territory. Here, we discuss the lessons learnt from these trials, and review the Asymptomatic Carotid Atherosclerosis Study and the Asymptomatic Carotid Surgery Trial, which attempted to resolve the rather vexing issue of surgical treatment for patients with asymptomatic internal carotid artery stenosis. We also review the best medical treatment for patients undergoing carotid endarterectomy in the perioperative period, and examine the risk of ischemic stroke after CABG surgery, both when this procedure is performed alongside endarterectomy and when CABG surgery and endarterectomy are performed as a two-staged procedure.
Key Points
-
The role of carotid endarterectomy (CEA) in stroke prevention has been greatly clarified in the last 15 years
-
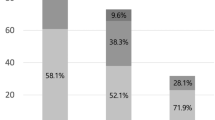
Early CEA is beneficial in patients with symptomatic carotid stenosis greater than 50%, provided the institutional perioperative complication rate is less than 6%
-
CEA is beneficial in patients with symptomatic carotid stenosis even in presence of carotid ulceration, contralateral carotid occlusion and to a lesser extent carotid near occlusion
-
Benefit gained from CEA in asymptomatic carotid stenosis is reduced and should probably be restricted to certain patient subgroups, provided the institutional perioperative complication rate is less than 3%
-
CEA is performed to prevent stroke during CABG surgery, but despite theoretical promise, the combined procedure has not yet been conclusively shown to be safer than the staged approach
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Fields WS et al. (1970) Joint study of extracranial arterial occlusion V—progress report of prognosis following surgery or nonsurgical treatment for transient cerebral ischemic attacks and cervical carotid artery lesions. JAMA 211: 1993–2003
Shaw DA et al. (1984) Carotid endarterectomy in patients with transient cerebral ischaemia. J Neurol Sci 64: 45–53
North American Symptomatic Carotid Endarterectomy Trial Collaborators (1991) Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. N Engl J Med 325: 445–453
European Carotid Surgery Trialists' Collaborative Group (1991) MRC European Carotid Surgery Trial: interim results for symptomatic patients with severe (70–99%) or with mild (0–29%) carotid stenosis. Lancet 337: 1235–1243
Mayberg MR et al. (1991) Carotid endarterectomy and prevention of cerebral ischemia in symptomatic carotid stenosis. Veterans Affairs Cooperative Studies Program 309 Trialist Group. JAMA 266: 3289–3294
Barnett HJM et al. (1998) Benefit of carotid endarterectomy in patients with symptomatic moderate or severe stenosis. N Engl J Med 339: 1415–1425
Rothwell PM et al.; Carotid Endarterectomy Trialists' Collaboration (2003) Analysis of pooled data from the randomised controlled trials of endarterectomy for symptomatic carotid stenosis. Lancet 361: 107–116
Goldstein LB et al. (1995) Comparison and meta-analysis of randomized trials of endarterectomy for symptomatic carotid artery stenosis. Neurology 45: 1965–1970
Alamowitch S et al.; North American Symptomatic Carotid Endarterectomy Trial (NASCET); ASA Trial Group; Carotid Endarterectomy (ACE) Trial Group (2005) The risk and benefit of endarterectomy in women with symptomatic internal carotid artery disease. Stroke 36: 27–31
Rothwell PM et al. (1994) Equivalence of measurements of carotid stenosis: a comparison of three methods on 1001 angiograms. European Carotid Surgery Trialists' Collaborative Group. Stroke 25: 2435–2439
Rothwell PM et al. (2003) Reanalysis of the final results of the European Carotid Surgery Trial. Stroke 34: 514–523
Bernstein M et al. (1984) Cerebral hyperperfusion after carotid endarterectomy: a cause of cerebral hemorrhage. Neurosurgery 15: 50–56
Piepgras DG et al. (1988) Intracerebral hemorrhage after carotid endarterectomy. J Neurosurg 68: 532–536
Ferguson GG et al. (1999) The North American Symptomatic Carotid Endarterectomy Trial: surgical results in 1,415 patients. Stroke 30: 1751–1758
Hafner DH et al. (1987) Massive intracerebral hemorrhage following carotid endarterectomy. Arch Surg 122: 305–307
Lovett JK et al. (2004) Early risk of recurrence by subtype of ischemic stroke in population-based incidence studies. Neurology 62: 569–573
Johnston SC et al. (2000) Short-term prognosis after emergency department diagnosis of TIA. JAMA 284: 2901–2906
Rothwell PM et al.; Carotid Endarterectomy Trialists' Collaboration (2004) Endarterectomy for symptomatic carotid stenosis in relation to clinical subgroups and timing of surgery. Lancet 363: 915–924
Chaturvedi S et al. (2005) Carotid endarterectomy—an evidence-based review: report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology 65: 794–801
Sacco RL et al. (2006) Guidelines for prevention of stroke in patients with ischemic stroke or transient ischemic attack: a statement for healthcare professionals from the American Heart Association/American Stroke Association Council on Stroke: co-sponsored by the Council on Cardiovascular Radiology and Intervention: the American Academy of Neurology affirms the value of this guideline. Stroke 37: 577–617
Bond R et al. (2005) A systematic review of the associations between age and sex and the operative risks of carotid endarterectomy. Cerebrovascular Dis 20: 69–77
Grego F et al. (2005) Is carotid endarterectomy in octogenarians more dangerous than in younger patients? J Cardiovasc Surg (Torino) 46: 477–483
Benavente O et al. (2001) Prognosis after transient monocular blindness associated with carotid-artery stenosis. N Engl J Med 345: 1084–1090
Grego F et al. (2005) Is contralateral carotid artery occlusion a risk factor for carotid endarterectomy? Ann Vasc Surg 19: 882–889
AbuRahma AF et al. (2000) Perioperative and late stroke rates of carotid endarterectomy contralateral to carotid artery occlusion: results from a randomized trial. Stroke 31: 1566–1571
Klijn CJ et al. (2000) Outcome in patients with symptomatic occlusion of the internal carotid artery. Eur J Vasc Endovasc Surg 19: 579–586
Gasecki AP et al. (1995) Long-term prognosis and effect of endarterectomy in patients with symptomatic severe carotid stenosis and contralateral carotid stenosis or occlusion: results from NASCET. North American Symptomatic Carotid Endarterectomy Trial (NASCET) Group. J Neurosurg 83: 778–782
Park AE et al. (1998) Carotid plaque morphology correlates with presenting symptomatology. J Vasc Surg 27: 872–878
Fisher M et al. (2005) Carotid plaque pathology: thrombosis, ulceration, and stroke pathogenesis. Stroke 36: 253–257
Eliasziw M et al. (1994) Significance of plaque ulceration in symptomatic patients with high-grade carotid stenosis. North American Symptomatic Carotid Endarterectomy Trial. Stroke 25: 304–308
Streifler JY et al. (1994) Angiographic detection of carotid plaque ulceration: comparison with surgical observations in a multicenter study. North American Symptomatic Carotid Endarterectomy Trial. Stroke 25: 1130–1132
Morgenstern LB et al. (1997) The risks and benefits of carotid endarterectomy in patients with near occlusion of the carotid artery. North American Symptomatic Carotid Endarterectomy Trial (NASCET) Group. Neurology 48: 911–915
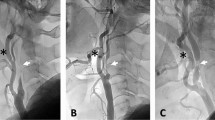
Fox AJ et al. (2005) Identification, prognosis, and management of patients with carotid artery near occlusion. AJNR Am J Neuroradiol 26: 2086–2094
Hobson R et al. (1995) Endarterectomy for asymptomatic carotid artery stenosis. Executive Committee for the Asymptomatic Carotid Atherosclerosis Study. JAMA 273: 1421–1428
Halliday A et al.; MRC Asymptomatic Carotid Surgery Trial (ACST) Collaborative Group (2004) Prevention of disabling and fatal strokes by successful carotid endarterectomy in patients without recent neurological symptoms: randomised controlled trial. Lancet 363: 1491–1502
Chambers BR and Donnan GA . Carotid endarterectomy for asymptomatic carotid stenosis. Cochrane Database Systematic Reviews 2005, Issue 4. Art. No.: CD001923. DOI: 10.1002/14651858.CD001923.pub2
Barnett HJM et al. (2002) The appropriate use of carotid endarterectomy. CMAJ 166: 1169–1179
Goldstein LB et al. (1998) Multicenter review of preoperative risk factors for endarterectomy for asymptomatic carotid artery stenosis. Stroke 29: 750–753
Taylor DW et al. (1999) Low-dose and high-dose acetylsalicylic acid for patients undergoing carotid endarterectomy: a randomised controlled trial. ASA and Carotid Endarterectomy (ACE) Trial Collaborators. Lancet 353: 2179–2184
Engelter S and Lyrer P . Antiplatelet therapy for preventing stroke and other vascular events after carotid endarterectomy. Cochrane Database Systematic Reviews 2003, Issue 3. Art. No.: CD001458. DOI: 10.1002/14651858.CD001458
Poldermans D et al. (2003) Statins are associated with a reduced incidence of perioperative mortality in patients undergoing major noncardiac vascular surgery. Circulation 107: 1848–1851
Devereaux PJ et al. (2005) How strong is the evidence for the use of perioperative beta blockers in non-cardiac surgery? Systematic review and meta-analysis of randomised controlled trials. BMJ 331: 313–321
McGirt MJ et al. (2005) 3-Hydroxy-3-methylglutaryl coenzyme A reductase inhibitors reduce the risk of perioperative stroke and mortality after carotid endarterectomy. J Vasc Surg 42: 829–836
Faggioli GL et al. (1990) The role of carotid screening before coronary artery bypass. J Vasc Surg 12: 724–729
Cirillo F et al. (2001) Associated vascular lesions in patients undergoing coronary artery bypass grafting. Acta Cardiol 56: 91–96
Hogue CW Jr et al. (1999) Risk factors for early or delayed stroke after cardiac surgery. Circulation 100: 642–647
Roach GW et al. for The Multicenter Study of Perioperative Ischemia Research Group and the Ischemia Research and Education Foundation Investigators (1996) Adverse cerebral outcomes after coronary bypass surgery. N Engl J Med 335: 1857–1863
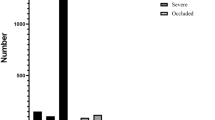
Chiappini B et al. (2005) Simultaneous carotid and coronary arteries disease: staged or combined surgical approach? J Card Surg 20: 234–240
Naylor AR et al. (2003) A systematic review of outcomes following staged and synchronous carotid endarterectomy and coronary artery bypass. Eur J Vasc Endovasc Surg 25: 380–389
Ricotta JJ et al. (2005) The influence of concurrent carotid endarterectomy on coronary bypass: a case-controlled study. J Vasc Surg 41: 397–401
Hill MD et al. (2005) Simultaneous carotid endarterectomy and coronary artery bypass surgery in Canada. Neurology 64: 1435–1437
Findlay JM and Marchak BE (2002) Reoperation for acute hemispheric stroke after carotid endarterectomy: is there any value? Neurosurgery 50: 486–492
Rothwell PM et al. (1997) Clinical and angiographic predictors of stroke and death from carotid endarterectomy: systematic review. BMJ 315: 1571–1577
AbuRahma AF et al. (2001) Redo carotid endarterectomy versus primary carotid endarterectomy. Stroke 32: 2787–2792
Acknowledgements
Charles P Vega, University of California, Irvine, CA, is the author of and is solely responsible for the content of the learning objectives, questions and answers of the Medscape-accredited continuing medical education activity associated with this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Rajamani, K., Chaturvedi, S. Surgery Insight: carotid endarterectomy—which patients to treat and when?. Nat Rev Cardiol 4, 621–629 (2007). https://doi.org/10.1038/ncpcardio1008
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1038/ncpcardio1008
This article is cited by
-
Transient ischemic attack and minor stroke as “surgeons affairs”: a narrative review
Neurological Sciences (2023)