Abstract
Therapygenetics, the study of genetic determinants of response to psychological therapies, is in its infancy. Here, we investigate whether single-nucleotide polymorphisms in nerve growth factor (NGF) (rs6330) and brain-derived neutrotrophic factor (BDNF) (rs6265) genes predict the response to cognitive behaviour therapy (CBT). Neurotrophic genes represent plausible candidate genes: they are implicated in synaptic plasticity, response to stress, and are widely expressed in brain areas involved in mood and cognition. Allelic variation at both loci has shown associations with anxiety-related phenotypes. A sample of 374 anxiety-disordered children with white European ancestry was recruited from clinics in Reading, UK, and in Sydney, Australia. Participants received manualised CBT treatment and DNA was collected from buccal cells using cheek swabs. Treatment response was assessed at post-treatment and follow-up time points. We report first evidence that children with one or more copies of the T allele of NGF rs6330 were significantly more likely to be free of their primary anxiety diagnosis at follow-up (OR=0.60 (0.42–0.85), P=0.005). These effects remained even when other clinically relevant covariates were accounted for (OR=0.62 (0.41–0.92), P=0.019). No significant associations were observed between BDNF rs6265 and response to psychological therapy. These findings demonstrate that knowledge of genetic markers has the potential to inform clinical treatment decisions for psychotherapeutic interventions.
Similar content being viewed by others
Introduction
Anxiety disorders frequently onset in childhood1 are highly prevalent2 and often persist into adolescence and adulthood.3 They are associated with a wide range of impairments4, 5, 6 and are a major risk factor for future psychological7 and physical health problems.8 Given the considerable suffering, dysfunction and poor prognosis associated with child anxiety, ensuring that treatments are maximally efficacious is of critical importance.
Remission rates in the most established first-line treatment for child anxiety, cognitive behavior therapy (CBT), are approximately 55% immediately post treatment, rising to around 65% by 6–12-month follow-up.9 This means that 35–45% of children retain significant impairments following treatment. Only limited work has investigated the predictors of children's treatment response to CBT, despite the potential of such an approach to guide treatment and improve outcome. The most convincing predictors are increased symptom severity,10 parental psychopathology11, 12 and comorbid mood disorders.13
While the field of pharmacogenetics is well established,14 therapygenetics, the study of genetic markers that predict response to psychological therapy, is a novel research area. In the most comprehensive study to date,15 we showed that anxiety-disordered children (N=270) with the 5-HTTLPR SS genotype were 20% more likely to be free of their primary anxiety diagnosis following CBT than those with SL/LL genotypes. 5-HTTLPR SS genotype predicted better treatment response even after controlling for other significant clinical covariates. However, this effect was seen only at follow-up (assessed at 3, 6 or 12 months) and not immediately post treatment. Similarly, the SS genotype (and S/Lg and Lg/Lg) predicted increased sensitivity to an experimental attention bias modification intervention designed to manipulate attentional biases either toward threat or toward positive stimuli.16 However, another study with adult bulimia patients found that the 5-HTTLPR S allele predicted a poorer treatment response, irrespective of whether it was CBT, medication or combined therapy.17 The contradictory results between Eley et al.15 and Steiger et al.17 most likely reflect small samples, varying phenotypes and the use of medication. Finally, an association was observed between COMT val158met and CBT response in adult panic disorder;18 however, many patients also received medication. A recent review argues strongly for incorporating genetic variation into psychological treatment research given its potential to shed light on psychopathology, enhance the ability to tailor personalised treatments on the basis of genetic profile and improve treatment efficacy.19
Building on the very modest therapygenetics literature so far, this study examines associations between polymorphisms in nerve growth factor (NGF rs6330, also referred to as 104C>T) and brain-derived neutrotrophic factor (BDNF rs6265, also referred to as Val66Met) and response to CBT in a sample of anxiety-disordered children. In brief, both NGF and BDNF are neurotrophic genes that regulate growth factors involved in the development, differentiation and survival of neurons. Neurotrophic markers are plausible candidates for involvement in response to psychological therapy. They have a key role in synaptic plasticity and long-term potentiation, are implicated in the orchestration of HPA axis response to stress and are widely expressed in limbic areas of the central nervous system (for example, hippocampus, insula, anterior cingulate cortex) involved in mood and cognition.20 Reduced neurotrophic signalling and neurotrophin-mediated neuronal plasticity may be implicated in the pathophysiology of a range of psychiatric disorders and their therapy.21, 22, 23
A non-synonymous single-nucleotide polymorphism in the NGF gene, rs6330, produces an alanine to valine substitution at amino acid position 35, and is thought to affect intracellular processing and secretion of NGF.24 Studies in rodent and non-human primates have shown that NGF (and BDNF) levels are sensitive to environmental influences, such as maternal separation, deprivation and changes to the rearing environment.25, 26, 27 NGF blood levels also increase in response to anxiety and acute arousal states in humans.28, 29 NGF serum levels also rise in response to positive environments, namely, after successful but not unsuccessful CBT treatment for generalised anxiety disorder.30 Allelic variations at the rs6330 locus have previously shown associations with anxiety-related traits and affective disorders. NGF genotype interacted with gender to predict trait-anxiety scores, with higher anxiety seen in females with the CC genotype compared with CT and TT genotype carriers, but with the opposite effect observed in males.31 In contrast, the T allele of rs6330 has been associated with affective disorders in females.32
BDNF secretion is activity dependent, with decreases associated with stress and mood disorders, whereas antidepressant treatment increases BDNF secretion.22, 33, 34, 35 In the functional rs6265 (Val66Met) polymorphism, the more common G allele encodes for valine (Val), whereas the A allele encodes for methionine (Met). The Met allele is associated with diminished activity-dependent secretion of BDNF,36, 37 structural brain abnormalities in limbic regions of the central nervous system,38, 39, 40 impaired hippocampal activity,41 impaired associative fear learning,42 and, in knock-in mice, defective BDNF secretion and increased anxiety-related behaviour.37
Association studies in humans have yielded heterogenous findings with regard to determining the risk allele for anxiety-related traits. Some studies have reported an association between the Val66 allele and higher neuroticism scores;43, 44 a meta-analysis concluded that the Met variant, despite its unfavourable biological effects, was associated with lower neuroticism.45 Others have reported no significant association between either allele and neuroticism scores.46, 47, 48 However, others report significant associations between Met carriers and increased introversion,49 harm avoidance50 and significant gene–gene (for example, with 5-HTTLPR) and gene–environment interactions for anxiety and depression-related (endo)phenotypes.49, 51, 52, 53, 54 A better antidepressant treatment response is also observed for the Met variant.55
To date, no studies have investigated whether neurotrophic gene polymorphisms predict response to purely psychological therapy, despite NGF and BDNF being associated with anxiety responses in humans and neural plasticity and BDNF appearing to mediate antidepressant treatment response. Furthermore, given our recent finding that 5-HTTLPR genotype predicts treatment response to CBT, evidence of genetic epistasis between 5-HTTLPR and neurotrophic markers (particularly BDNF Val66Met) and a role for BDNF in mediating serotonergic antidepressant response, it is also of interest to explore whether neurotrophic gene polymorphisms interact with 5-HTTLPR to predict treatment response. Here, we test these novel hypotheses in a sample of anxiety-disordered children aged 6–13 years receiving CBT.
Materials and methods
Participants
Six hundred and thirteen children aged 6–13 years and meeting the DSM-IV56 criteria for a primary anxiety-disorder diagnosis were recruited (participation rate=73%). Exclusion criteria were significant physical/intellectual impairment and psychoses. Genotyping data were available for 593 children for NGF rs6330 and 604 children for BDNF rs6265. Parental DNA was obtained from 525 mothers and 457 fathers for rs6330, and from 583 mothers and 458 fathers for rs6265, with 414 and 424 complete trios for rs6330 and rs6265, respectively.
Recruitment was done at two clinical sites: Sydney, Australia and Reading, UK. The Australian sample was recruited from referrals to randomised CBT-based treatment trials undertaken by the Centre for Emotional Health at Macquarie University (N=429). The UK sample was recruited from two CBT-based clinical trials at the Berkshire Child Anxiety Clinic, University of Reading (N=156) and a feasibility study of CBT-based guided self-help within the Oxfordshire Primary Child and Adolescent Mental Health Service (N=24). Treatment was based on the Cool Kids Program.57
Children's ethnicity was assessed using the ancestry of their grandparents. Those with four grandparents of white European ancestry were included in the ‘white’ subgroup (N=374) and data from this subset are analysed here. Sample descriptives for this sample are reported in Table 1. This sample overlaps to a significant extent with the sample reported in our earlier paper on the associations between treatment response and the 5-HTTLPR.15 Fifteen extra cases are included in this paper for whom genotype data were available for rs6330 and/or rs6265 but who were not included in our earlier paper because of not having 5-HTTLPR genotype data. The numbers of subjects from other ethnic subgroups were too small for a separate analysis (African or Caribbean, N=2; Asian, N=14; Arab and Middle Eastern, N=9; Mixed, N=41; ancestry unknown and missing data, N=173).
Controls consisted of 459 white Europeans (61% female, mean age±s.d., 31.95±12.62) recruited for the Bipolar Affected Case–Control study.58 Participants were excluded if they, or a first-degree relative, ever fulfilled the criteria or received treatment for any psychiatric disorder.
Measures
Child diagnoses were made using the Anxiety Disorders Interview Schedule for DSM-IV, Parent and Child Versions (ADIS-IV-C/P59), and based on composite parent/child report and clinician severity rating (CSR; 0–8). Diagnostic criteria were applied by graduate or clinical psychologists, with diagnosis assigned when the child met the diagnostic criteria and received a CSR of 4 or more. Inter-rater reliability across diagnostic subtypes was excellent at both sites (>0.80 for anxiety disorders, >0.65 for mood disorders).60, 61 The percentages of children with specific disorders as their (a) primary diagnosis or (b) anywhere in their profile were as follows: separation anxiety disorder (18.7%, 48.5%); social phobia (20.9%, 62.5%); generalised anxiety disorder (44.7%, 79.9%); specific phobia (9.4%, 56.7%); panic/agoraphobia (0.8%, 3.0%); obsessive compulsive disorder (3.5%, 10.5%); post-traumatic stress disorder (0.3%, 0.8%) and anxiety disorders not otherwise specified (1.9%, 2.1%). Mood disorders were present in 10.2% of the children (depression: 3.5%; dysthymia: 6.7%), with attention deficit hyperactivity disorder present in 11.5% and oppositional defiant disorders in 12.1% of the children.
Maternal and paternal depression, anxiety and stress over the past week at the pretreatment time point were assessed using the self-report Depression, Anxiety and Stress Scale (DASS-21) (ref. 62). Three subscales consisting of 7 items each were calculated: stress, anxiety and depression, with scores for each subscale ranging from a possible 0 to 42 (subscale totals are multiplied by 2). Internal consistency for each scale was 0.85, 0.77 and 0.89, respectively. For the purpose of the analyses reported here, a single mean score across the three subscales was computed.
Genotyping
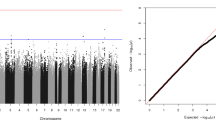
Genomic DNA was extracted from buccal swabs (for cases) and blood samples (for controls) using established procedures.63, 64 Genotyping was performed using the Sequenom MassARRAY iPLEX Gold technology (Sequenom, San Diego, CA, USA). Primers for PCR amplification and extension probes were purchased from Metabion (Martinsried, Germany). PCR and extension reactions were performed according to the iPLEX Gold protocol, with 10 ng of genomic template per sample. Extension products were analysed on a compact MALDI-TOF Mass Spectrometer (Sequenom). Genotypes were assigned automatically using the MassARRAY SpectroTyper 4.0 software (Sequenom) and then individually inspected in order to remove erroneous calls. Quality control measures included eight negative controls per 384-well plate and 4% of samples genotyped in duplicate to confirm inter-plate reproducibility. The genotyping success rate was 98.1% for rs6330 and 99% for rs6265. Genotype distribution conformed to the Hardy–Weinberg equilibrium for rs6330 (χ21=0.56, P=0.453) and rs6265 (χ21=0.05, P=0.823).
Procedure
Ethical approval was granted at each site by Human Ethics and Biosafety Committees (National Research Ethics Service: Berkshire Research Ethics Committee and Macquarie University Ethics Review Committee (Human Research)). Informed consent was sought from parents and verbal assent from children. Buccal swabs were collected either at the clinic or through the post. Diagnostic data were available before and after treatment (N=336 children; 89.8%) and at one follow-up point (N=278; 74.3%). The timing of the follow-up differed across trials (3, 6 and 12 months) and for these the N (percentage) values were as follows: 41 (11.0%), 217 (58.0%) and 20 (5.3%) available at the 3-, 6- and 12-month follow-up points, respectively Those without follow-up data differed from those with follow-up data by being significantly more likely to have a comorbid mood disorder (χ21=10.44, P=0.001, 18.8% vs 7.2%), being significantly older (t(372)=2.94, P=0.003, 9.93 vs 9.30 years) and having a less severe primary anxiety disorder before treatment (t(372)=−2.41, P=0.016, 5.96 vs 6.23).
Statistical analyses
The primary outcome was treatment response for primary anxiety diagnosis at follow-up using an additive genotype model. We note whether any effects survive multiple testing correction using a Bonferroni adjusted P value of 0.017 correcting for the analysis of three independent markers, investigated in this and our previous paper.15 Only when the additive model retained significance after applying multiple testing corrections do we report recessive and dominant genetic models. No further correction is applied, because these are not independent tests. We also report treatment response data at post treatment and for all anxiety diagnoses, for subsets of the data (for example, only those with follow-up data at 6 months) and interactions with 5-HTTLPR. We do not apply further multiple testing corrections, because these are supplementary analyses that test the same core hypothesis and are not fully independent tests. Finally, we present secondary analyses investigating case–control and family-based associations. We do not apply multiple testing corrections for these secondary analyses. Stringently correcting for all primary and secondary analyses presented on the three markers described here and in our previous paper with the 5-HTTLPR would require a Bonferroni adjusted P value of 0.002. None of the analyses reported here would survive this correction. However, we consider this to be very conservative given that the vast majority of analyses performed for each marker do not represent independent tests.
Results
Treatment response analyses
Treatment response was classified as (1) primary anxiety response: the absence of the primary anxiety disorder and (2) all anxiety response: the absence of any anxiety diagnosis. Treatment response was assessed immediately post treatment and at follow-up (collapsed across the time point, although usually 6 months after the end of treatment, with a proportion assessed at 3 and 12 months post treatment). We used logistic regression analyses with robust standard errors and maximum likelihood estimation to test for differences in treatment response using the additive genetic model. No significant effects of genotype were observed immediately post treatment for either polymorphism (see Table 2).
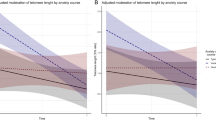
For NGF genotypes, a significant difference in treatment response was observed for primary anxiety response at follow-up (Table 2). This effect was significant for the additive model and supported by inspection of frequency data, with each extra T allele conferring a more positive treatment response (OR=0.60 (95% CI: 0.42–0.85), P=0.005), with this effect surviving multiple testing corrections. As shown in Figure 1, 53.2% of those with the CC genotype were free of their primary anxiety diagnosis and 63.5% of those with the CT genotype showed a positive treatment response, while 76.7% of those with the TT genotype were free of their primary anxiety diagnosis at follow-up. As the additive model survived multiple testing corrections, analyses were performed for recessive and dominant genetic models. A significant effect of NGF genotype was also observed in both models (recessive: OR=0.45 (0.23–0.87), P=0.018; dominant: OR=0.55 (0.32–0.93), P=0.026). For all anxiety response, the additive model indicated a non-significant statistical trend (OR=0.73 (0.52–1.02), P=0.067), with the percentage of treatment responders for each genotype as follows: CC: 40.5%; CT: 45.3%; TT: 56.7% (see Figure 1). No significant effects of the BDNF polymorphism on treatment response were observed (see Table 2).
Next we determined whether the significant effect of NGF genotype remained even after controlling for other possible covariates. As a first stage, genotype (CC coded as −1, CT coded as 0, TT coded as 1), time (linear and quadratic terms to account for the use of three different follow-up time points), age, gender and treatment site (Sydney or Reading) were entered into the model. For primary anxiety response only NGF genotype was a significant predictor (OR 0.58 (0.40–0.84), P=0.004, see Table 3, model 1), indicating that with each additional T allele children were significantly less likely to have their primary anxiety disorder at follow-up. This effect survived multiple testing corrections. This pattern of findings was also similar when analyses were performed on (a) the entire sample (that is, white subset+other ethnicities) (OR=0.72 (0.54–0.96), P=0.024); (b) those with 6-month follow-up only (OR=0.64 (0.42–0.97), P=0.037) and (c) those who received an eight session in-person CBT programme (OR=0.61 (0.41–0.92), P=0.018). In a subsequent model (Table 3, model 2), we included other variables that were significant predictors of treatment response (comorbid mood disorders, pretreatment symptom severity and maternal psychopathology were significant predictors, paternal psychopathology was not a significant predictor) in their own right. Importantly, NGF genotype remained a significant predictor of treatment response for primary anxiety response when controlling for these other factors (OR =0.62 (0.41–0.92), P=0.019); see Table 3. However, this effect marginally exceeded the Bonferroni-corrected P-value. For the more stringent test of all anxiety response, the effect size was similar but non-significant (OR=0.71 (0.50–1.00), P=0.051, see Table 3).
Interaction with 5-HTTLPR
Using multiple logistic regression analyses with robust standard errors and maximum likelihood estimation, we investigated the interaction between (i) BDNF genotype (AA/AG coded as 1, GG coded as 0 as the dominant model was most strongly indicated by frequency data) and 5-HTTLPR genotype (SS coded as 1, SL/LL coded as 0) and (ii) NGF genotype (CC coded as −1, CT coded as 0, TT coded as 1) and 5-HTTLPR genotype as predictors of primary anxiety response at follow-up. The basic model included genotypes, time (linear and quadratic terms), age, gender and treatment site (see Table 4, model 1).
For rs6265 there was no significant main effect (OR=0.99 (0.56–1.78), P=0.983) or interaction with 5-HTTLPR (OR=2.43 (0.48–12.33), P=0.285). The inclusion of rs6265 in the model did not diminish the predictive power of 5-HTTLPR (OR=0.31 (0.12–0.75), P=0.010), with this effect surviving multiple testing corrections.
As main effects (that is, no interaction term in the model), both NGF genotype and 5-HTTLPR significantly predicted treatment response (NGF: OR=0.58 (0.40–0.84), P=0.004; 5-HTTLPR: OR=0.38 (0.18–0.80), P=0.011, see Table 4, model 1), with both effects surviving multiple testing corrections. Adding an interaction term did not reduce the predictive power of either NGF (OR=0.57 (0.38–0.85), P=0.006) or 5-HTTLPR (OR=0.39 (0.18–0.85), P=0.017, see Table 4, model 2). The interaction term was non-significant (OR=1.12 (0.40–3.12), P=0.823) and was therefore omitted from model 3. In model 3, the significant effect of both markers was retained even after controlling for other significant clinical covariates (NGF: OR=0.59 (0.39–0.89), P=0.013; 5-HTTLPR: OR=0.36 (0.16–0.82), P=0.015).
Case–control and family-based analyses
Genotypic frequencies were compared between cases (N=374) and never-psychiatrically-ill controls (N=459). There were no significant differences using the additive model and no other genetic models were indicated for either rs6265 ((GG, GA, AA); cases: 67.5%, 29.5%, 3.0% and controls: 64.3%, 32.7%, 3.1%, P=0.388) or rs6330 ((CC, CT, TT); cases: 29.5%, 47.8%, 22.7% and controls: 30.3%, 50.8% 19.0%, P=0.363). Within-family analyses using transmission-disequilibrium tests (TDT) on the trios from the case sample only (child, mother and father; N=273 (rs6330) and N=278 (rs6265)) were also non-significant (rs6330: χ22=0.09, P=0.763; rs6265: χ22=0.62, P=0.429).
Discussion
Children with a primary anxiety disorder with one or more copies of the NGF rs6330 T allele were significantly more likely to be free of their primary anxiety diagnosis at follow-up. We observed an additive effect, with each extra T allele conferring a more positive treatment response: children with the TT genotype were 23.5% more likely to be free of their primary anxiety diagnosis at follow-up than those children with the CC genotype, whereas those with the CT genotype were 10.3% more likely to show remission compared with CC-genotype children. The association between genotype and treatment response remained significant even when other clinically relevant covariates were included in the model. No significant association between BDNF rs6265 genotype and response to psychological therapy was observed, in contrast to previous work reporting associations with antidepressant treatment response.55 Both NGF and 5-HTTLPR were independent predictors of anxious children's response to psychological therapy. However, there was no evidence for an interaction between these markers, which is consistent with past work.65 There were no case–control or within-family transmission differences for either polymorphism. This is counter to previous work reporting associations between both BDNF and NGF polymorphisms and anxiety-related phenotypes.
The effects of NGF genotype on psychological treatment response were observed only at follow-up, with no significant effects evident immediately post treatment. This mirrors the pattern of findings we reported with 5-HTTLPR genotype.15 The period between post-treatment and follow-up is often characterised by continued improvement, as the child continues to apply the skills learnt during therapy; thus, it is possible that, as with the 5-HTTLPR SS genotype, having one or more NGF T alleles influences the capacity for continued benefit from the intervention. Further studies are necessary to determine the precise functionality of this single nucleotide polymorphism (or linked SNPs) and the mechanism by which it may affect response to CBT. This is particularly pertinent given the heterogeneity in the existing literature regarding which allele confers the risk for anxiety and depressive disorders.31, 32 However, NGF is a plausible candidate gene for involvement in psychological treatment response for anxiety. It is expressed in limbic areas important for mood and cognition and there is evidence of effects on synaptic plasticity and neurogenesis and regulation of endocrine responses to stress. In particular, NGF is known to act on neurite outgrowth, making it especially well placed to determine structural changes in neural circuitry. A rise in serum NGF is also an indicator of positive treatment response in generalised anxiety disorder patients following CBT.30 One possibility is that children with the T allele may show subtle differences in neurotrophic signalling that influence the extent to which environmental influences bring about neuroplastic modifications, which in turn modulate the mood.
Neuroplasticity represents a plausible biological mechanism through which psychological interventions may exert some of their therapeutic effects.66 CBT is a learning-based intervention in which patients actively recall, reappraise and reconstruct their experiences. The aim is to improve problem-solving capacities, modify self-representations and regulate distressing affective states. Significant learning experiences of the kind undertaken during CBT may very well be underpinned by neuroplastic modifications in brain activity and function.66 Neuroimaging studies of psychological interventions lend weight to this hypothesis.67 Several studies have shown that psychological interventions alter brain function (measured by brain blood flow and oxygen/glucose metabolism) in individuals with unipolar mood disorders68, 69 and a range of anxiety disorders (OCD,70, 71, 72 panic disorder,73 social anxiety disorder,74 specific phobia75, 76 and PTSD77), with these changes consistent with the reduction in symptoms observed following treatment. Preliminary evidence also suggests that CBT may stimulate structural brain alterations reflective of neuroplasticity. After 16 sessions of CBT, women with chronic fatigue syndrome showed small increases in grey matter of the lateral prefrontal cortex.78 However, the study of changes in brain structure and function across psychological interventions is relatively new and many findings require replication and methodological improvements before definitive conclusions can be made regarding the neural effects of these interventions.67 In particular, it remains to be determined whether CBT has a causal influence on brain structure and function.
The present findings may have important clinical implications. These and our previous data,15 if replicated, suggest that knowledge of genetic markers could be used to inform clinical treatment decisions for psychotherapeutic as well as pharmacological interventions. However, to do so, genetic markers will need to yield sufficiently large effects to make a clinically meaningful contribution to psychological treatment response prediction. Recent work has shown using simulation data that for a genetic marker with a minor allele frequency (MAF) of 30% (that approximates the MAF for rs6330), a per-allele difference of 2.4 points on the Hamilton Rating Scale for Depression would be required to explain 6.3% of the variance in outcome in an antidepressant trial.79 Only then would the genetic marker be considered a clinically meaningful predictor of treatment outcome. The simulations are also extended to categorical outcomes (for example, remission status) and suggest that pseudo r2 values can be approximately translated to the clinically meaningful effect size measure of number needed to assess (NNA). For the clinical significance criterion of 6.3%, this corresponds to a NNA of 3: meaning that for every three patients assessed for a genetic marker, one significantly more accurate prediction of outcome can be made. In the present data, a model containing only NGF rs6330 genotype yielded a pseudo r2 estimate of 0.023 and an area under the curve (AUC) of 0.5938. Converting AUC to NNA using the methods outlined79 (see also Kraemer and Kupfer80) produces an NNA of 5.33. This suggests that for every five patients assessed for rs6330, one significantly more accurate prediction of outcome could be made. However, our summary statistic of choice is the percentage difference in treatment response between genotype groups: compared with individuals with no copies of the T allele, 23.5% more children with the TT genotype had a positive treatment response. We consider this to be indicative of a clinically meaningful effect. However, we also concur with the views of others79 that clinically significant prediction by genetic markers is likely to be best achieved by combining multiple genetic markers (perhaps in combination with clinical predictors) into predictive indices or algorithms.
This study has several limitations worthy of consideration. First, there is no independent replication, so these results should be considered preliminary. Although the main findings were consistent in direction in both the white subset and the entire sample, giving us confidence in the veracity of the results, some of the findings reported do not survive multiple testing corrections. Following conservative correction for all primary and secondary analyses performed in this and our previous paper, none of the analyses reported survived multiple testing correction. In our lab, we are in the process of working towards obtaining a replication sample. We intend to explore a limited number of additional plausible candidate markers in this original data set. This manuscript outlines the analyses we have performed to date and we will continue to take this approach going forwards. Second, the sample size, although large for a child anxiety treatment trial, is relatively small for a genetic association study. This may have reduced power to detect significant effects in some of our analyses. Third, the functional relevance of the NGF SNP (rs6330) remains underspecified, particularly with regard to the mechanisms by which the T allele may confer a benefit in terms of treatment response. We also limited our investigations to just two SNPs, each previously associated with anxiety phenotypes. However, it remains plausible that other NGF and BDNF variants may contribute both to susceptibility to anxiety disorders and to psychological therapy response. Fourth, our main analyses were performed on a subset who self-reported having four white European ancestry grandparents. However, without the benefit of ancestrally informative markers, it is not possible to eliminate the potential risk of hidden population substructures.
In summary, allelic variation in NGF rs6330 significantly predicted response to CBT in children with a primary anxiety diagnosis. These findings show that interactions between genetic variation and environmental experiences (here, psychological therapy) can influence not only the development but also the remission of psychiatric outcomes. Genetic predictors of treatment response may prove to be particularly informative given that they can be measured with little error and remain stable over time. Knowing an anxious child's genetic makeup with regard to NGF rs6330 and 5-HTTLPR genotype has predictive power for treatment prognosis, above and beyond ‘traditional’ clinical predictors such as disorder severity, comorbid mood disorders and parental psychopathology. This information could be beneficial in helping to decide whether a child is likely to benefit from standard CBT alone or whether an enhanced treatment is required in order to maximise the chance of them improving.
References
Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE . Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry 2005; 62: 593–602.
Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui L et al. Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication--Adolescent Supplement (NCS-A). J Am Acad Child Adolesc Psychiatry 2010; 49: 980–989.
Weems CF . Developmental trajectories of childhood anxiety: identifying continuity and change in anxious emotion. Dev Rev 2008; 28: 488–502.
Asendorpf JB, Denissen JJA, van Aken MAG . Inhibited and aggressive preschool children at 23 years of age: Personality and social transitions into adulthood. Dev Psychol 2008; 44: 997–1011.
Erath S, Flanagan K, Bierman K . Social anxiety and peer relations in early adolescence: behavioral and cognitive factors. J Abnorm Child Psychol 2007; 35: 405–416.
Owens M, Stevenson J, Norgate R, Hadwin J . Processing efficiency theory in children: working memory as a mediator between trait anxiety and academic performance. Anxiety Stress Copin 2008; 21: 417–430.
Kim-Cohen J, Caspi A, Moffitt TE, Harrington H, Milne BJ, Poulton R . Prior juvenile diagnoses in adults with mental disorder: developmental follow-back of a prospective-longitudinal cohort. Arch Gen Psychiatry 2003; 60: 709–717.
Beesdo K, Hoyer, Jacobi F, Low NCP, Ĥfler M, Wittchen H-U . Association between generalized anxiety levels and pain in a community sample: Evidence for diagnostic specificity. J Anxiety Disord 2009; 23: 684–693.
James A, Soler A, Weatherall R . Cognitive behavioural therapy for anxiety disorders in children and adolescents. Cochrane Database of Systematic Reviews 2005.
Hudson JL . Efficacy of cognitive-behavioural therapy for children and adolescents with anxiety disorders. Behav Change 2005; 22: 55–70.
Bodden DH, Bogels SM, Nauta MH, De Haan E, Ringrose J, Appelboom C et al. Child versus family cognitive-behavioral therapy in clinically anxious youth: an efficacy and partial effectiveness study. J Am Acad Child Adolesc Psychiatry 2008; 47: 1384–1394.
Rapee RM, Schniering CA, Hudson JL . Anxiety disorders during childhood and adolescence: origins and treatment. Ann Rev Clin Psychol 2009; 5: 311–341.
Ollendick TH, Jarrett MA, Grills-Taquechel AE, Hovey LD, Wolff JC . Comorbidity as a predictor and moderator of treatment outcome in youth with anxiety, affective, attention deficit/hyperactivity disorder, and oppositional/conduct disorders. Clin Psychol Rev 2008; 28: 1447–1471.
Keers R, Aitchison KJ . Pharmacogenetics of antidepressant response. Expert Rev Neurother 2011; 11: 101–125.
Eley TC, Hudson JL, Creswell C, Tropeano M, Lester KJ, Cooper P et al. Therapygenetics: The 5HTTLPR and response to psychological therapy. Mol Psychiatry 2012; 17: 236–237.
Fox E, Zougkou K, Ridgewell A, Garner K . The serotonin transporter gene alters sensitivity to attention bias modification: evidence for a plasticity gene. Biol Psychiatry 2011; 70: 1049–1054.
Steiger H, Joober R, Gauvin L, Bruce KR, Richardson J, Israel M et al. Serotonin-system polymorphisms (5-HTTLPR and -1438G/A) and responses of patients with bulimic syndromes to multimodal treatments. J Clin Psychiatry 2008; 69: 1565–1571.
Lonsdorf TB, Ruck C, Bergstrom J, Andersson G, Ohman A, Lindefors N et al. The COMTval158met polymorphism is associated with symptom relief during exposure-based cognitive-behavioral treatment in panic disorder. BMC Psychiatry 2010; 10: 99.
Beevers CG, McGeary JE . Therapygenetics: moving towards personalized psychotherapy treatment. Trends Cogn Sci 2012; 16: 11–12.
Cirulli F, Alleva E . The NGF saga: from animal models of psychosocial stress to stress-related psychopathology. Front Neuroendocrinol 2009; 30: 379–395.
Castren E, Voikar V, Rantamaki T . Role of neurotrophic factors in depression. Curr Opin Pharm 2007; 7: 18–21.
Sen S, Duman R, Sanacora G . Serum brain-derived neurotrophic factor, depression, and antidepressant medications: meta-analyses and implications. Biol Psychiatry 2008; 64: 527–532.
Duman RS, Monteggia LM . A neurotrophic model for stress-related mood disorders. Biol Psychiatry 2006; 59: 1116–1127.
Syed Z, Dudbridge F, Kent L . An investigation of the neurotrophic factor genes GDNF, NGF, and NT3 in susceptibility to ADHD. Am J Med Genet B 2007; 144B: 375–378.
Branchi I, D'Andrea I, Fiore M, Di Fausto V, Aloe L, Alleva E . Early social enrichment shapes social behavior and nerve growth factor and brain-derived neurotrophic factor levels in the adult mouse brain. Biol Psychiatry 2006; 60: 690–696.
Cirulli F, Alleva E, Antonelli A, Aloe L . NGF expression in the developing rat brain: effects of maternal separation. Brain Res Dev Brain Res 2000; 123: 129–134.
Cirulli F, Francia N, Branchi I, Antonucci MT, Aloe L, Suomi SJ et al. Changes in plasma levels of BDNF and NGF reveal a gender-selective vulnerability to early adversity in rhesus macaques. Psychoneuroendocrinology 2009; 34: 172–180.
Alleva E, Santucci D . Psychosocial vs ‘physical’ stress situations in rodents and humans: role of neurotrophins. Physiol Behav 2001; 73: 313–320.
Aloe L, Bracci-Laudiero L, Alleva E, Lambiase A, Micera A, Tirassa P . Emotional stress induced by parachute jumping enhances blood nerve growth factor levels and the distribution of nerve growth factor receptors in lymphocytes. Proc Natl Acad Sci USA 1994; 91: 10440–10444.
Jockers-Scherubl MC, Zubraegel D, Baer T, Linden M, Danker-Hopfe H, Schulte-Herbruggen O et al. Nerve growth factor serum concentrations rise after successful cognitive-behavioural therapy of generalized anxiety disorder. Prog NeuroPsychopharmacol Biol Psychiatry 2007; 31: 200–204.
Lang UE, Hellweg R, Bajbouj M, Gaus V, Sander T, Gallinat J . Gender-dependent association of a functional NGF polymorphism with anxiety-related personality traits. Pharmacopsychiatry 2008; 41: 196–199.
Cui D, Zhang H, Yang BZ, Listman JB, Li D, Price LH et al. Variation in NGFB is associated with primary affective disorders in women. Am J Med Genet B Neuropsychiatr Genet 2011; 156B: 401–412.
Mattson MP, Maudsley S, Martin B . BDNF and 5-HT: a dynamic duo in age-related neuronal plasticity and neurodegenerative disorders. Trends Neurosci 2004; 27: 589–594.
Martinowich K, Lu B . Interaction between BDNF and serotonin: role in mood disorders. Neuropsychopharmacology 2008; 33: 73–83.
Chen B, Dowlatshahi D, MacQueen GM, Wang J-F, Young LT . Increased hippocampal bdnf immunoreactivity in subjects treated with antidepressant medication. Biol Psychiatry 2001; 50: 260–265.
Egan MF, Kojima M, Callicott JH, Goldberg TE, Kolachana BS, Bertolino A et al. The BDNF val66met polymorphism affects activity-dependent secretion of BDNF and human memory and hippocampal function. Cell 2003; 112: 257–269.
Chen ZY, Jing D, Bath KG, Ieraci A, Khan T, Siao CJ et al. Genetic variant BDNF (Val66Met) polymorphism alters anxiety-related behavior. Science 2006; 314: 140–143.
Bueller JA, Aftab M, Sen S, Gomez-Hassan D, Burmeister M, Zubieta JK . BDNF Val66Met allele is associated with reduced hippocampal volume in healthy subjects. Biol Psychiatry 2006; 59: 812–815.
Frodl T, Schule C, Schmitt G, Born C, Baghai T, Zill P et al. Association of the brain-derived neurotrophic factor Val66Met polymorphism with reduced hippocampal volumes in major depression. Arch Gen Psychiatry 2007; 64: 410–416.
Gallinat J, Schubert F, Bruhl R, Hellweg R, Klar AA, Kehrer C et al. Met carriers of BDNF Val66Met genotype show increased N-acetylaspartate concentration in the anterior cingulate cortex. Neuroimage 2010; 49: 767–771.
Hariri AR, Goldberg TE, Mattay VS, Kolachana BS, Callicott JH, Egan MF et al. Brain-derived neurotrophic factor val66met polymorphism affects human memory-related hippocampal activity and predicts memory performance. J Neurosci 2003; 23: 6690–6694.
Hajcak G, Castille C, Olvet DM, Dunning JP, Roohi J, Hatchwell E . Genetic variation in brain-derived neurotrophic factor and human fear conditioning. Genes Brain Behav 2009; 8: 80–85.
Lang UE, Hellweg R, Kalus P, Bajbouj M, Lenzen KP, Sander T et al. Association of a functional BDNF polymorphism and anxiety-related personality traits. Psychopharmacology (Berl) 2005; 180: 95–99.
Sen S, Nesse RM, Stoltenberg SF, Li S, Gleiberman L, Chakravarti A et al. A BDNF coding variant is associated with the neo personality inventory domain neuroticism, a risk factor for depression. Neuropsychopharmacology 2003; 28: 397–401.
Frustaci A, Pozzi G, Gianfagna F, Manzoli L, Boccia S . Meta-analysis of the brain-derived neurotrophic factor gene (BDNF) Val66Met polymorphism in anxiety disorders and anxiety-related personality traits. Neuropsychobiology 2008; 58: 163–170.
Willis-Owen SA, Fullerton J, Surtees PG, Wainwright NW, Miller S, Flint J . The Val66Met coding variant of the brain-derived neurotrophic factor (BDNF) gene does not contribute toward variation in the personality trait neuroticism. Biol Psychiatry 2005; 58: 738–742.
Terracciano A, Sanna S, Uda M, Deiana B, Usala G, Busonero F et al. Genome-wide association scan for five major dimensions of personality. Mol Psychiatry 2010; 15: 647–656.
van den Oord EJCG, Kuo P-H, Hartmann AM, Webb BT, Moller H-J, Hettema JM et al. Genomewide association analysis followed by a replication study implicates a novel candidate gene for neuroticism. Arch Gen Psychiatry 2008; 65: 1062–1071.
Terracciano A, Tanaka T, Sutin AR, Deiana B, Balaci L, Sanna S et al. BDNF Val66Met is associated with introversion and interacts with 5-HTTLPR to influence neuroticism. Neuropsychopharmacology 2010; 35: 1083–1089.
Montag C, Basten U, Stelzel C, Fiebach CJ, Reuter M . The BDNF Val66Met polymorphism and anxiety: Support for animal knock-in studies from a genetic association study in humans. Psychiatry Res 2010; 179: 86–90.
Gatt JM, Nemeroff CB, Dobson-Stone C, Paul RH, Bryant RA, Schofield PR et al. Interactions between BDNF Val66Met polymorphism and early life stress predict brain and arousal pathways to syndromal depression and anxiety. Mol Psychiatry 2009; 14: 681–695.
Dougherty LR, Klein DN, Congdon E, Canli T, Hayden EP . Interaction between 5-HTTLPR and BDNF Val66Met polymorphisms on HPA axis reactivity in preschoolers. Biol Psychol 2010; 83: 93–100.
Pezawas L, Meyer-Lindenberg A, Goldman AL, Verchinski BA, Chen G, Kolachana BS et al. Evidence of biologic epistasis between BDNF and SLC6A4 and implications for depression. Mol Psychiatry 2008; 13: 709–716.
Hunnerkopf R, Strobel A, Gutknecht L, Brocke B, Lesch KP . Interaction between BDNF Val66Met and dopamine transporter gene variation influences anxiety-related traits. Neuropsychopharmacology 2007; 32: 2552–2560.
Kato M, Serretti A . Review and meta-analysis of antidepressant pharmacogenetic findings in major depressive disorder. Mol Psychiatry 2010; 15: 473–500.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. American Psychiatric Association: Washington, DC, 1994.
Lyneham HJ, Schniering CA, Hudson JL, Rapee RM . The Cool Kids Program - Adolescent Version. Macquarie University Anxiety Research Unit: Sydney, 2005.
Schosser A, Gaysina D, Cohen-Woods S, Chow PC, Martucci L, Craddock N et al. Association of DISC1 and TSNAX genes and affective disorders in the depression case-control (DeCC) and bipolar affective case-control (BACCS) studies. Mol Psychiatry 2010; 15: 844–849.
Silverman WK, Albano AM . The Anxiety Disorders Interview Schedule for Children-IV (Child and Parent Versions). Oxford University Press: New York, 1996.
Hudson JL, Rapee RM, Deveney C, Schniering CA, Lyneham HJ, Bovopoulos N . Cognitive-behavioral treatment versus an active control for children and adolescents with anxiety disorders: a randomized trial. J Am Acad Child Adolesc Psychiatry 2009; 48: 533–544.
Lyneham HJ, Abbott MJ, Rapee RM . Interrater reliability of the anxiety disorders interview schedule for dsm-iv: child and parent version. J Am Acad Child Adolesc Psychiatry 2007; 46: 731–736.
Lovibond PF, Lovibond SH . The structure of negative emotional states: comparison of the depression anxiety stress scales (dass) with the beck depression and anxiety inventories. Behav Res Ther 1995; 33: 335–343.
Freeman B, Powell J, Ball D, Hill L, Craig I, Plomin R . DNA by mail: an inexpensive and noninvasive method for collecting DNA samples from widely dispersed populations. Behav Genet 1997; 27: 251–257.
Freeman B, Smith N, Curtis C, Huckett L, Mill J, Craig IW . DNA from buccal swabs recruited by mail: evaluation of storage effects on long-term stability and suitability for multiplex polymerase chain reaction genotyping. Behav Genet 2003; 33: 67–72.
Mossner R, Daniel S, Albert D, Heils A, Okladnova O, Schmitt A et al. Serotonin transporter function is modulated by brain-derived neurotrophic factor (BDNF) but not nerve growth factor (NGF). Neurochem Int 2000; 36: 197–202.
Garland EL, Howard MO . Neuroplasticity, psychosocial genomics, and the biopsychosocial paradigm in the 21st century. Health Soc Work 2009; 34: 191–199.
Frewen PA, Dozois DJ, Lanius RA . Neuroimaging studies of psychological interventions for mood and anxiety disorders: empirical and methodological review. Clin Psychol Rev 2008; 28: 228–246.
Goldapple K, Segal Z, Garson C, Lau M, Bieling P, Kennedy S et al. Modulation of cortical-limbic pathways in major depression: treatment-specific effects of cognitive behavior therapy. Arch Gen Psychiatry 2004; 61: 34–41.
Martin SD, Martin E, Rai SS, Richardson MA, Royall R . Brain blood flow changes in depressed patients treated with interpersonal psychotherapy or venlafaxine hydrochloride: preliminary findings. Arch Gen Psychiatry 2001; 58: 641–648.
Baxter Jr LR, Schwartz JM, Bergman KS, Szuba MP, Guze BH, Mazziotta JC et al. Caudate glucose metabolic rate changes with both drug and behavior therapy for obsessive-compulsive disorder. Arch Gen Psychiatry 1992; 49: 681–689.
Nakatani E, Nakgawa A, Ohara Y, Goto S, Uozumi N, Iwakiri M et al. Effects of behavior therapy on regional cerebral blood flow in obsessive-compulsive disorder. Psychiatry Res 2003; 124: 113–120.
Schwartz JM, Stoessel PW, Baxter Jr LR, Martin KM, Phelps ME . Systematic changes in cerebral glucose metabolic rate after successful behavior modification treatment of obsessive-compulsive disorder. Arch Gen Psychiatry 1996; 53: 109–113.
Prasko J, Horacek J, Zalesky R, Kopecek M, Novak T, Paskova B et al. The change of regional brain metabolism (18FDG PET) in panic disorder during the treatment with cognitive behavioral therapy or antidepressants. Neuro Endocrinol Letters 2004; 25: 340–348.
Furmark T, Tillfors M, Marteinsdottir I, Fischer H, Pissiota A, Langstrom B et al. Common changes in cerebral blood flow in patients with social phobia treated with citalopram or cognitive-behavioral therapy. Arch Gen Psychiatry 2002; 59: 425–433.
Paquette V, Levesque J, Mensour B, Leroux JM, Beaudoin G, Bourgouin P et al. ‘Change the mind and you change the brain’: effects of cognitive-behavioral therapy on the neural correlates of spider phobia. Neuroimage 2003; 18: 401–409.
Straube T, Glauer M, Dilger S, Mentzel HJ, Miltner WH . Effects of cognitive-behavioral therapy on brain activation in specific phobia. Neuroimage 2006; 29: 125–135.
Felmingham K, Kemp A, Williams L, Das P, Hughes G, Peduto A et al. Changes in anterior cingulate and amygdala after cognitive behavior therapy of posttraumatic stress disorder. Psychol Sci 2007; 18: 127–129.
de Lange FP, Koers A, Kalkman JS, Bleijenberg G, Hagoort P, van der Meer JW et al. Increase in prefrontal cortical volume following cognitive behavioural therapy in patients with chronic fatigue syndrome. Brain 2008; 131 (Pt 8): 2172–2180.
Uher R, Tansey KE, Malki K, Perlis RH . Biomarkers predicting treatment outcome in depression: what is clinically significant? Pharmacogenomics 2012; 13: 233–240.
Kraemer HC, Kupfer DJ . Size of treatment effects and their importance to clinical research and practice. Biol Psychiatry 2006; 59: 990–996.
Acknowledgements
This study was supported by the Australian Research Council (DP0666048), Australian National Health and Medical Research Council (PG382008 and PG488505), UK Medical Research Council (MRC; GU601020, G0802326 and G0901874) and the UK National Institute for Health Research (PBPG019712042). Creswell is supported by MRC Fellowship G0601874. The Bipolar-Affected Case Control Study was supported by GlaxoSmithKline, Research and Development.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-No Derivative Works 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Lester, K., Hudson, J., Tropeano, M. et al. Neurotrophic gene polymorphisms and response to psychological therapy. Transl Psychiatry 2, e108 (2012). https://doi.org/10.1038/tp.2012.33
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/tp.2012.33
Keywords
This article is cited by
-
Effectiveness of Mindfulness-Based Cognitive Therapy for Positive Clinical Outcome in Panic Disorder: a 5-year Longitudinal Study
Mindfulness (2021)
-
NGF (−198C > T, Ala35Val) and p75NTR (Ser205Leu) gene mutations are associated with liver function in different histopathological profiles of the patients with chronic viral hepatitis in the Brazilian Amazon
Molecular Medicine (2020)
-
Genetics in child and adolescent psychiatry: methodological advances and conceptual issues
European Child & Adolescent Psychiatry (2015)
-
Therapygenetics: Using genetic markers to predict response to psychological treatment for mood and anxiety disorders
Biology of Mood & Anxiety Disorders (2013)