Abstract
The physiological relationship between local arterial displacement and blood pressure (BP) plays an integral role in assess- ment of the mechanical properties of arteries. In this study, we used more advanced methods to obtain reliable continuous BP and the displacement of the common carotid artery (CCA) simultaneously. We propose a novel evaluation method for arterial stiffness that relies on determining the physiological relationship between the axial and radial displacements of the CCA wall and beat-to-beat BP. Patients (total of 138) were divided into groups according to the following three criteria: essential hyper- tension (EH) and normotension, male and female, elderly and younger. The Pearson correlation test and canonical correlation analysis showed that the CCA indices were significantly correlated with BP indices (r = 0:787; p < 0:05). The slope of the CCA displacement/pressure curve showed a progressive reduction with increasing age and EH disease occurrence (EH: 0.496 vs. normotension: 0.822; age <= 60:0.585 vs. age > 60:0.783). Our method provides an explicit reference value and relationship for the manner in which the CCA wall responds to changes in BP. Short-term and continuous BP were significantly correlated with CCA displacement and exhibited a close inverse relationship with each subject’s BP and EH, age, and systolic blood pressure.
Similar content being viewed by others
Introduction
Atherosclerosis has been considered the main cause of morbidity and mortality in relation to cardiovascular diseases. As a result, the evaluation of arterial stiffness has become a popular research field, receiving wide attention1. In previous studies, substantial evidence has demonstrated that arterial stiffness undergoes a progressive change with aging, yielding values that are markedly changed in cases of hypertension and a variety of other diseases2,3,4. Such changes are also known to give rise to adverse clinical consequences. Arterial wall displacement refers to the deformation and rate of deformation of an arterial wall in axial, planes, and circumferential planes. Increased stiffness of the large central arteries, as estimated by the common carotid artery (CCA) wall displacement, is a risk factor for atherosclerosis5,6,7. However, blood pressure (BP) is the pressure exerted by the circulating blood on the walls of blood vessels. The displacement of the arterial wall is associated with the development of stresses due to the BP and blood flow, as well as tethering into the surrounding tissues8. Through observing a temporal relationship between the blood velocity wave and anterograde carotid artery longitudinal wall displacement, the relationship between carotid artery movement and left ventricular rotation has been found9. Several researchers have revealed the relationship between blood pressure variability (BPV) and alterations to the artery, identifying the mean level of and variability in the BP as potential risk factors for arterial stiffness10,11. Therefore, the accurate evaluation of the physiological relationship between arterial wall displacement and changes in pulse pressure is important for exploring the mechanism of arterial stiffness, which has an important clinical value.
The displacement of the arterial wall has been under study for many decades. As a physical phenomenon, the radial displacement of the artery is easy to explain based on the combined action of variations in the BP gradient, the elastic properties of the arterial wall, and the periphery of the pressure wave reflection12. The axial expansion of the arterial wall is a relatively new phenomenon. It was first discovered in the 1950s, although it is typically considered to be negligible compared to the radial expansion of these vessels13. Due to medical imaging technical problems with participant observation of the distension of the axial artery wall, the axial displacement of the arterial wall remains a more complex phenomenon that is harder to measure than radial displacement. Recently, improvements in ultrasound resolution have contributed to the speckle tracking image analysis method that has been used to quantify arterial wall movements in two dimensions. Speckle tracking uses a block matching scheme to track the position of speckle patterns in carotid artery tissue through a sequence of b-mode ultrasound images14. At present, many research achievements based on speckle tracking ultrasound imaging to estimate CCA wall mechanics have been obtained15,16,17,18. For instance, the association between the acute double-leg press exercise and similar transient changes in CCA wall mechanics at low and moderate intensities has been demonstrated19. Similarly, the BPV is an important factor in assessments of end-organ damage, independent of the traditional BP level; the target organs of such studies have mainly been the heart, brain, and kidneys20. With a high BPV, CCA wall remodeling is mainly characterized by an increase in the intima media thickness (IMT), which allows the vessel to maintain its circumferential wall stress but changes the stiffness and thickness of the CCA. CCA short-axis ultrasound images have shown that circumferential wall displacement of the CCA wall is significantly related to pulse pressure21. Moreover, increased pulse pressure as well as increased stiffness and thickness of the CCA wall are known to be significant, independent predictors of cardiovascular complications22. Changes in the stiffness and thickness of the CCA are determinative effects for displacing the CCA wall. However, in previous studies, most BPV parameters were captured either from 24-hour ambulatory BP monitoring (ABPM) or following several BP measurements recorded during home visits using clinical BPV23,24,25. As a result, many current methods: (1) focus solely on associations between carotid artery longitudinal displacements and cardiovascular disease risk factors26; and (2) measure continuous BP, which is not accurate and is estimated by complex mathematical assumptions27. (3) Simultaneously obtaining reliable short-term BP measurements and measurements of axial and radial (2-D) displacement of the CCA wall at same time period has not been investigated.
The aim of this study was to determine the relationship between two-dimensional (axial and radial) motions of the CCA wall and beat-to-beat BP to explore the mechanism of arterial stiffness in longitudinal ultrasound images. We aimed to solve the limitations of current methods for assessing carotid artery motion properties in which continuous BP is estimated by complex mathematical assumptions and arterial expansion evaluations are not accurate enough. Our method may have several advantages: (1) an index of arterial dispensability that includes the integrated characteristics and interactive influence of axial and radial displacements are provided, which ensures the influence of each individual indicator; (2) BP is used as a new, continuous physiological parameter and the issue of how 2-D arterial function varies on a beat-to-beat BP basis has never been addressed previously; (3) A more accurate 2-D displacement of the CCA has been obtained by a novel and reliable motion-tracking algorithm; and (4) it simultaneously obtains a reliable short-term BP measurement and measurement of 2-D displacement of the CCA wall at same time.
Materials and Methods
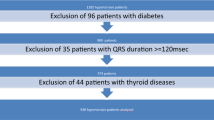
Study Participants
The study protocol was designed according to the principles of the Declaration of Helsinki and was approved by the Ethics Committee of the Second People’s Hospital of Shenzhen in China. The study objectives and design have not been previously published. All participants provided written informed consent. The study population consisted of 138 Chinese participants aged 29 to 81 years (59.6 ± 11.4 years). Among the participants, 85 participants were suffering from essential hypertension and 19 participants were diagnosed with diabetes. Risk factors such as smoking, alcohol, and body mass index were recorded.
Beat-to-beat BP and Carotid Arterial Displacement
In the experiment, both the beat-to-beat BPs and CCA displacements were gathered as continuous data, Hence to complete our analysis, we needed to measure the values at the same time. Beat-to-beat recordings of the systolic BP (mmHg) and diastolic BP (mmHg) were measured using a Finometer system Model-2 (Midi). A cuff was attached to the left upper arm close to the elbow for continuous beat-by-beat measurement of BP. For both the entire group and each of the individuals in this study, one ultrasound physician with more than 10 years of experience measured and evaluated the axial and radial displacements of the left and right carotid artery walls using a high-resolution ultrasound system (iU22, Philips Ultrasound, Bothell, WA, USA) and 7.5 MHz linear array transducer. During collection, all of the measurements were made with patients in a supine position. Scanning was performed on both CCAs in the lateral plane, 2–5 cm proximal to the carotid bifurcation, so that the CCA segment was displayed as a rectilinear structure (Fig. 1). Video clips of six consecutive cardiac cycles were obtained for each participant. All imaging data were saved in both the DICOM format and as CDs for off-line analysis.
Tracking the 2D displacement of the Carotid Artery Wall
The 2D displacement of the carotid artery wall in the ultrasound sequence was tracked using the H∞-based block matching method (HBM). The HBM uses the state-space equation to describe the motion of the target tissue on the carotid artery wall as below28

where Xn is the estimated location of the target tissue, Yn is the observed location of the target tissue acquired by the block matching method, Wn and Vn are noise terms, and n is the time or frame index. Then, the H∞ filter was used to compute the optimal estimate of the target tissue location using a min-max approach. Given the worst possible disturbances from the data, our HBM method can still ensure optimal estimation of carotid artery wall motion29.
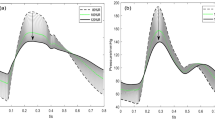
Carotid Artery and Blood Pressure Curves
According to the separate axial and radial displacements of the left and right carotid artery walls and BP signals, 4-type displacement/pressure curves were obtained via software, which was developed with MATLAB. From the recording time, an initial alignment of pressure and 2-D displacement waveforms was obtained. Then, a correction factor of 30–60 milliseconds was applied to the CCA displacement to correct the delay due to the propagation of the carotid artery pressure wave. It was also applied for removal of nonlinear waveforms and dealing with semiautomatic irregular waveforms. Once aligned, the beginning and end of the segments to be analyzed within each waveform were visually identified on a complete cardiac cycle between two late diastole phases (Fig. 2). When CCA displacement/pressure curves were calculated, the curve fitting method was used to estimate the best slope for the curve.
(a) Axial and radial displacement of the left and right carotid artery walls. The red line represents the axial displacement of the left CCA. The blue line represents the radial displacement of the left CCA. The green line represents the axial displacement of the right CCA. The yellow line represents the radial displacement of the right CCA. (b) An initial alignment of the pressure and CCA displacement waveforms.
Carotid Artery and Blood Pressure Assessments
The motion of the CCA wall includes axial motion in the left CCA wall (LAM), radial motion in the left CCA wall (LRM), axial motion in the right CCA wall (RAM), and radial motion in the right CCA wall (RRM). The systolic blood pressure variability (SBPV) and diastolic blood pressure variability (DBPV) were examined using the systolic blood pressure (SBP) and diastolic blood pressure (DBP). The measurements from the beat-to-beat BP and motion of the CCA wall were assessed by the mean level and variability indices in the time and frequency domains. The BP indices in the time domain included the mean value (MEAN), standard deviation (SD), coefficient of variation (CV), successive variation (SV), average real variability (ARV), and residual standard deviation (RSD)24,30,31,32. The CCA indices, as with the BP indices, could be computed to reflect the characteristics of the four types of CCA wall motion. The definitions of these indices are listed in Table 1.
Canonical Correlation Analysis
Canonical correlation analysis is an approach for making sense of cross-covariance matrices. When there are two vectors X = (x1, …, xn) and Y = (y1, …, ym) of random variables, and there are correlations among the variables, canonical correlation analysis will identify linear combinations of Xi and Yi that are maximally correlated with each other33:

where U and V are the first pair of canonical variables. The vectors a and b such that the random variables a′X and b′X maximize the correlation ρ = corr(a′X, b′Y). Canonical correlation analysis is the general procedure for investigating the relationships between two sets of variables34.
Canonic correlation analysis is used to investigate the relationships between two sets of variables and it is preceded by a hypothesis test. In this case, we used Lilliefors test to validate our data satisfying the normal distribution (lillietest, MATLAB). The Pearson’s linear correlation coefficient was used to detect multiple co-linear relationships among the variables. The results showed that there was a correlation between the variables, but not a strong correlation (r = −0.323–0.46, p < 0.05). Meanwhile, multivariate statistics and F approximations demonstrated that our data satisfied the linear correlation between the variables group and canonical correlation coefficients significantly (Wilks’lambada and F value, p value).
Statistical Analysis
Pearson’s linear correlation coefficient test was employed to measure the correlation between the BP and CCA indices. The Benjamini & Hochberg method was used to construct multiple comparison corrected confidence intervals that corresponded to the FDR-adjusted p-values35. Then, the canonical correlation analysis was used to assess the interrelation and interactions of the CCA indices and BP indices. Finally, according to whether participants had essential hypertension and their sex and age, we grouped all of the participants and identified the similarities and differences between each group. The results of this analysis are demonstrated in the carotid artery displacement/blood pressure curves and canonical correlation analysis. We implemented all codes using MATLAB R2012a on a desktop computer with Intel(R) Xeon(R) CPU E5-2650 (2.00 GHz) and 32 GB DDR2 memory. The statistical analysis was implemented with SPSS (Statistical Product and Service Solutions) 23.0 using a statistical software package (IBM, Armonk, NY), and a calculated difference of P < 0.05 was considered statistically significant.
Results
Baseline Characteristics
Participants were a mean (standard deviation) of 59.6 (11.4) years old, and 76 (55.1%) were male. The participants included two diseases: 19 (13.8%) had diabetes, and 76 (55.1%) had essential hypertension. The smoking, alcohol and coffee rates were 23.2%(32), 14.1%(20) and 2.8%(4), respectively. The mean SBP was 140.2 (23.3) mmHg, and the average DBP was 74.5 (13.4) mmHg. The mean LAM was −0.8 (28.6) pixels, and the mean LRM was 3.7 (9.9) pixels. The mean RAM was −3.8 (25.7) pixels, and the mean RRM was 3.6 (9.3) pixels.
Beat-to-beat BP Index Associations with Left CCA Indices
Tables 2 and 3 show the Pearson’s linear correlation coefficients between CCA indices and BP indices after adjustment of p-values by Benjamini & Hochberg method. A total of 288 sets of correlation coefficients were calculated; 51 sets were significantly correlated with each other (r = −0.323–0.462, p < 0.05). In particular, the residual standard deviation of axial displacement in the left CCA wall (LAM_SV) was the strongest positive that was significantly correlated with the coefficient of variation of the systolic blood pressure (SBPV_SD) (r = 0.105, p < 0.05), and LRM_RSD was the strongest positive that was significantly correlated with the SBPV_RSD (r = 0.462, P < 0.05). LRM_SV was the strongest negative that was significantly correlated with the DBPV_MEAN (r = −0.242, p < 0.05), and LAM_ARV was the strongest negative that was significantly correlated with the DBPV_MEAN (r = −0.323, p < 0.05).
Canonical Correlation Analysis
Canonical correlation analysis was used to test the integration relativity between the CCA indices and BPV indices. It was also used to study the positive and negative factors in the correlation.There was a strong canonical correlation between the CCA and BP indices (r = 0.787, p < 0.05). Furthermore, the SBPV_SD, DBPV_SD, DBPV_CV DBPV_SV, LRM_SD, and LRM_ARV were the major positive factor relative contributions to the relationship. Similarly, the SBPV_CV, SBPV_RSD, DBPV_RSD, LRM_RSD, and RRM_ARV were the major negative factor relative contributions to the relationship. Table 4 presents the canonical correlation analysis between beat-to-beat BP indices and CCA indices.
Essential Hypertension Disease Subgroup Analyses
According to whether participants had essential hypertension (EH), all of the subject were subdivided into the EH and NEH groups. As shown in Fig. 3, both in the axial and radial dimensions, the slope of the CCA displacement/pressure curve was lower in EH than in NEH participants (EH:0.496vs.NEH:0.822). Canonical correlation analysis was also used to measure the relativity between the CCA indices and BP indices in both groups, revealing major differences in the contributing factors. There were significant correlations between the CCA and BP indices for both groups (r = 0.907andr = 0.919, respectively; p < 0.05). The major positive influencing factors in the EH group were SBPV_CV, SBPV_SV, DBPV_SD, LRM_SD, and LRM_ARV, and the major negative influencing factors were SBP_SD, SBP_ARV, and LRM_RSD. The major positive influencing factors in the NEH group were SBPV_SD, DBPV_CV, LRM_SD, and LRM_ARV. The major negative influencing factors are SBPV_CV, SBPV_RSD, DBPV_RSD, and LRM_RSD. These findings are summarized in Table 5.
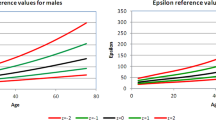
Sex Subgroup Analyses
Figure 4 and Table 6 present the CCA displacement/pressure curve and different correlations between CCA and BP indices as well as the interrelation between each influencing factor in males and females. The average slope of the male curve was similar to that in females (0.861vs.0.808), and there were significant correlations between CCA and BP indices for both groups (r = 0.940andr = 0.919, respectively; p < 0.05). However, the SBPV_CV, SBPV_SV, DBPV_ARV, and DBPV_RSD mostly had positive coefficients and the SBPV_SD, SBPV_ARV, SBPV_RSD, DBPV_SV, and LAM_ARV had significantly negative coefficients for the correlation in the male group. Similar results were recorded in the female group.
Age Subgroup Analyses
Participants in the elderly group (age > 60) had lower slopes compared to the younger group (age <= 60), as shown in Figs 5 and 6 (including EH: 0.585vs.0.783; without EH: 0.572vs.0.667, respectively). Similar to the results described above, Tables 7 and 8, show both groups yielded significant canonical correlations between the CCA and BP indices (including EH: r = 0.870 and 0.926; without EH: r = 0.890 and 0.882, respectively; p < 0.05). DBPV_SD, DBPV_CV, DBPV_CV, DBPV_SV, and RAM_SD were significantly positively correlated in the elderly group. SBPV_CV, SBPV_RSD, DBPV_ARV, DBPV_RSD, and LRM_RSD had a significant positive effect on the correlation. In contrast, SBPV_CV, SBPV_RSD, DBPV_RSD, LAM_SD, LAM_SD, and RRM_SD were major positive correlation factors, and SBPV_SD, SBPV_ARV, DBPV_SD, DBPV_CV, DBPV_SV, LRM_SD, LRM_ARV, and RRM_RSD were major negative correlation factors in the younger group.
Discussion
In this study, we estimated the 2-D displacement of the carotid artery wall and beat-to-beat BP as well as the influence of age, sex, and essential hypertension on the estimations. Our goal was to conduct preliminary trials that validated the interrelation and interaction between the CCA and BP indices as well as to assess the mechanical properties of the artery. In previous studies, a series of effective methods for studying the axial and radial movements of the arterial wall was presented36,37,38,39. Our method was as follows: (1) We used a H∞ filter based standard block matching method (BM) method to estimate the motion of the carotid artery wall from the ultrasound image sequences28. This approach used a newer software version with a free trace feature that did not make any assumptions about the vessel geometry and allowed for more precise measurements of both the axial and radial displacements of the left and right carotid artery walls; (2) Compared with the traditional methods of ABPM or readings from several BP measurements in home visits using clinical BPV, beat-to-beat recordings of BP offered a new, continuous physiological parameter. This approach is recommended as the best means to capture short-term BPV, while intermittent ABPM is less precise24. (3) Precise matching of the changes in artery 2-D displacement was carried out with the actual changes in intravascular pressure occurring at the same time. It helped us make more precise observations of how the CCA wall responded to blood pressure changes; and (4) Canonical correlation analysis was the best way to produce a model equation that related two sets of variables. The analysis relied on slopes to express both the displacement and pressure as continuous data.
The CCA wall invariably undergoes displacement with blood pressure changes because the essence of BP is the pressure exerted by circulating blood on the blood vessel walls. In our experiments, the most important finding was a strong canonical correlation between the beat-to-beat BP and carotid artery wall displacement, indicating that the two-dimensional motion of the carotid artery wall has a strong influence on the beat-to-beat BPV. This result is consistent with the findings presented in a previous publication, namely, that a basic physiological feature, the variability in the BP level, is a significant marker of the risk related to cardiovascular complications32,40,41. BP is a strong determinant of cardiovascular events, and aortic stiffening is highly associated with the progression to high BP in humans. Arterial stiffening plays a pivotal role in the progression of high BP and the development of cardiovascular disease23. Arterial stiffness occurs as a result of arteriosclerosis, which results from long-term cumulative damage in the artery42. Our experimental results provided a precise assessment function, which can allow for the identification, monitoring, and characterization of arteriosclerosis patients in non- or pre-clinical studies. Simultaneously, the impact of both positive and negative influencing factors on the result was clearly explained. We evaluated the relationship between the response of the CCA wall and the changes of the BP within the cardiac cycle in 138 participants as well as in multiple mechanical properties of the elastic artery.
Age, sex, and disease status, and possibly other independent risk factors, were also strongly and inversely associated with carotid displacement or BPV. Svedlund and Gan suggested that differences in age might have confounded the results of prior studies that showed impaired carotid longitudinal displacement in older adults with coronary artery disease and type- 2 diabetes43. Zhang et al. observed that the buffer effect of blood vessels can be enhanced by systemic structural changes in the arteries with age, which leads to increase SBP and, potentially, increased pulse pressure44. Our trial suggests that there is a highly significant correlation between carotid artery wall movement and BPV, whether participants are younger or older, male or female, or diagnosed with essential hypertension or not, which is consistent with our above result. The slope of the CCA displacement/pressure curve showed a progressive reduction with increasing age and EH disease status. It is a well-known phenomenon that arterial stiffness results in arterial displacement changes, the arterial stiffness rate increases with increasing age, and EH is one of the main diseases that affects arterial stiffness. While several clinical investigations have examined the association between menopause and the atherosclerotic cardiovascular risk, estrogen deficiency can protect females and mediate arterial stiffening with aging45,46. However, in our study, the male and female groups had nearly identical slopes of the CCA displacement/pressure curves. We can speculate that this similarity is because the average age of participants was high and most participating females were postmenopausal. Additionally, there were small differences between the axial and radial displacements and the left and right CCA in consecutive cardiac cycles, suggesting that modulation of the arterial mechanical response to continuous changes in intravascular pressure may undergo physiological variations.
ARV is a more appropriate parameter to measure variability, which provides a computationally simple way to estimate variation in a trend. As for ARV, RSD tends to be larger in absolute value and is influenced, to a greater extent, by large discrepancies between successive measurements. In our Pearson’s linear correlation analysis, the ARV and RSD of carotid artery wall displacement were more significantly correlated with BP indices. We also found the ARV and RSD of carotid artery wall movement had the same tendency of changes with the same BP indices in standardized canonical correlation coefficients. It suggested that ARV and RSD are the most appropriate predictors when expressing the relationship between CCA wall displacement and BP.
The common carotid artery is present on the left and right sides of the body. The left common carotid artery can be considered to have two parts, the thoracic (chest) and cervical (neck) regions. The right common carotid originates in or close to the neck, containing only a small thoracic portion47. Only the left common carotid artery has a substantial presence in the thorax. It originates directly from the aortic arch and travels upward through the superior mediastinum to the level of the left sternoclavicular joint. In canonical correlation analysis, the mechanical properties of the common carotid arteries support our findings and suggest that the LRM_SD and LRM_ARV are related to the SBPV_SD, DBPV_SD, DBPV_CV, and DBPV_SV. The data for the left carotid artery were more representative of the influence of the BP on the CCA wall than the data for the right carotid artery. Additionally, we also found the CCA radial displacements were more related to the BP indices than axial displacements, indicating that the changes in BP had more influence on CCA radial than axial displacements. BP plays a crucial role in vascular biology, and may affect IMT through blood vessel remodeling or wall hypertrophy in response to altered circumferential stress48. Meanwhile, IMT is a complex process, leading to changes in the local hemodynamics, shear stress and circumferential tensile stress. Those changes may cause the above mentioned results and thus possibly interferes with the axial displacement of the intima-media.
Fully elucidating the mutual roles of CCA wall displacement and the changes in BP based on our limited research is a difficult task as these elements appear to act in a complex system, impacting each other. However, some practical significance results can be obtained by our canonical correlation coefficients. For example, we found that a smaller SBPV_CV means a smaller LRM_RSD based on overall canonical correlation analysis. This enhanced the study in regard to traumatic effects of intravascular pressure excursions on the vessel wall, thereby favoring atherosclerosis formation mechanism research. Similarly, our 2-D artery and BP curves have also verified the slopes of the 2-D displacement-pressure relationship can be obtained from the carotid arteries during most of the ascending and descending portion of the pulse pressure wave, which may allow study of the mechanisms of this CCA variability and their possible alterations with disease. Additionally, the study of EH can be used to understand more about changing BP and stress levels and short-term changes in endothelial function and how they lead to some degree of variation in the reproducibility results.
There are certain limitations in our study. First, we chose a certain set of characteristics for evaluation and we grouped the participants without considering other known and confounding factors (smoking, alcohol and caffeine status) in the study population. Similarly, cultural factors, ethnic differences, and factors such as socioeconomic disadvantages and psychosocial stress may have contributed to the observed differences between the groups. Second, we focused on determining the relationship between the axial and radial displacements of the CCA wall and BP based on longitudinal ultrasound images. Therefore, more research should consider the influence of the circumferential displacement of the CCA wall to our results in the next stage, which also plays an important role in arterial wall mechanics and measurements based on short-axis ultrasound images. Similarly, simultaneous measurement avoids the error that occurs when measurements are made asynchronously. However, we must acknowledge the limitations that our key parameters were measured in different arteries; the blood pressure was measured in the brachial artery and arteria wall displacement was measured in the carotid artery. This limitation should also be investigated further. Finally, further research is needed on the relative contributions of both positive and negative factors for the CCA and beat-to-beat BP indices to improve our understanding of the relationships.
Conclusions
The two-dimensional motion of the carotid artery wall had a significant correlation with beat-to-beat BP indices, and positive or negative factors that contributed to the relationship were clearly identified. Additionally, we observed that the variation in the carotid artery wall displacement and BPV features could be influenced by multiple risk factors, including the age, sex, and essential hypertension status. Moreover, this new method allows for a precise, in-depth assessment of the carotid artery mechanical properties at rest. However, more research is required to validate these correlations under physiological stress.
Additional Information
How to cite this article: Xu, C. et al. Beat-to-Beat blood pressure and Two-dimensional (axial and radial) motion of the Carotid Artery Wall: physiological evaluation of arterial stiffness. Sci. Rep. 7, 42254; doi: 10.1038/srep42254 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Raitakari, O. T. et al. Endothelial function in healthy 11-year-old children after dietary intervention with onset in infancy: The Special Turku Coronary Risk Factor Intervention Project for children (STRIP). Circulation 112, 3786–3794 (2005).
Smulyan, H., Asmar, R. G., Rudnicki, a., London, G. M. & Safar, M. E. Comparative effects of aging in men and women on the properties of the arterial tree. Journal of the American College of Cardiology 37, 1374–1380 (2001).
Safar, M. E. et al. Metabolic syndrome and age-related progression of aortic stiffness. Journal of the American College of Cardiology 47, 72–75 (2006).
Waldstein, S. R. et al. Pulse pressure and pulse wave velocity are related to cognitive decline in the Baltimore longitudinal study of aging. Hypertension 51, 99–104 (2008).
Blacher, J. et al. Impact of aortic stiffness on survival in end-stage renal disease. Circulation 99, 2434–9 (1999).
Oishi, Y. et al. A novel approach to assess aortic stiffness related to changes in aging using a two-dimensional strain imaging. Echocardiography 25, 941–945 (2008).
Kim, K. H. et al. Usefulness of aortic strain analysis by velocity vector imaging as a new echocardiographic measure of arterial stiffness. Journal of the American Society of Echocardiography 22, 1382–1388 (2009).
Soleimani, E., Dizaji, M. M. & Saberi, H. Carotid artery wall motion estimation from consecutive ultrasonic images: Comparison between block-matching and maximum-gradient algorithms. Journal of Tehran University Heart Center 6, 72–78 (2011).
Au, J. S., Ditor, D. S., MacDonald, M. J. & Stöhr, E. J. Carotid artery longitudinal wall motion is associated with local blood velocity and left ventricular rotational, but not longitudinal, mechanics. Physiological Reports 4, e12872 (2016).
Xiong, H. et al. The relationship between the 24 h blood pressure variability and carotid intima-media thickness: A compared study. Computational and Mathematical Methods in Medicine 2014 (2014).
Stabouli, S. et al. Arterial stiffness and SBP variability in children and adolescents. J Hypertens 33, 88–95 (2015).
Dart, a. M. & Kingwell, B. a. Pulse pressure - A review of mechanisms and clinical relevance. Journal of the American College of Cardiology 37, 975–984 (2001).
Lawton, R. & Greene, L. A method for the in situ study of aortic elasticity in the dog. Authorized Medical Allowance List, US Naval and Air Development Center, Warminister, PA (Rep. No. NADC-MA-5603) (1956).
Beaussier, H. et al. Mechanical and structural characteristics of carotid plaques by combined analysis with echotracking system and MR imaging. JACC. Cardiovascular imaging 4, 468–77 (2011).
Tat, J., Au, J. S., Keir, P. J. & MacDonald, M. J. Reduced common carotid artery longitudinal wall motion and intramural shear strain in individuals with elevated cardiovascular disease risk using speckle tracking. Clinical physiology and functional imaging (2015).
Kouzu, H. et al. Left ventricular hypertrophy causes different changes in longitudinal, radial, and circumferential mechanics in patients with hypertension: a two-dimensional speckle tracking study. Journal of the American Society of Echocardiography 24, 192–199 (2011).
Bjällmark, A. et al. Ultrasonographic strain imaging is superior to conventional non-invasive measures of vascular stiffness in the detection of age-dependent differences in the mechanical properties of the common carotid artery. European Heart Journal-Cardiovascular Imaging jeq033 (2010).
Tsai, W.-C. et al. Association of left atrial strain and strain rate assessed by speckle tracking echocardiography with paroxysmal atrial fibrillation. Echocardiography 26, 1188–1194 (2009).
Black, J. M. et al. The effect of an acute bout of resistance exercise on carotid artery strain and strain rate. Physiological Reports 4, e12959–n/a (2016) E12959.
Miao, C.-Y., Xie, H.-H., Zhan, L.-S. & Su, D.-F. Blood pressure variability is more important than blood pressure level in determination of end-organ damage in rats. Journal of hypertension 24, 1125–1135 (2006).
Yuda, S. et al. Quantitative measurement of circumferential carotid arterial strain by two-dimensional speckle tracking imaging in healthy subjects. Echocardiography 28, 899–906 (2011).
Simons, P. C. et al. Common carotid intima-media thickness and arterial stiffness indicators of cardiovascular risk in high-risk patients the smart study (second manifestations of arterial disease) (1999).
Xu, L. et al. Correlation between beat-to-beat blood pressure variability and arterial stiffness in healthy adults in the cold pressor test. Australasian Physical & Engineering Sciences in Medicine 1–9 (2015).
Dolan, E. & O’Brien, E. Blood pressure variability clarity for clinical practice. Hypertension 56, 179–181 (2010).
Shintani, Y. et al. Ambulatory blood pressure, blood pressure variability and the prevalence of carotid artery alteration: the ohasama study. Journal of hypertension 25, 1704–1710 (2007).
Giannattasio, C. et al. Simultaneous measurement of beat-to-beat carotid diameter and pressure changes to assess arterial mechanical properties. Hypertension 52, 896–902 (2008).
Laurent, S. et al. Expert consensus document on arterial stiffness: methodological issues and clinical applications. European Heart Journal 27, 2588–2605 (2006).
Gao, Z. et al. Motion estimation of common carotid artery wall using a h∞filter based block matching method. 18th International Conference on Medical Image Computing and Computer Assisted Intervention (MICCAI) (2015).
Hassibi, B. & Kailath, T. H∞ adaptive filtering. In Acoustics, Speech, and Signal Processing, 1995. ICASSP-95., 1995 International Conference on, vol. 2, 949–952 (IEEE, 1995).
Parati, G., Ochoa, J. E., Lombardi, C. & Bilo, G. Assessment and management of blood-pressure variability. Nature reviews. Cardiology 10, 143–55 (2013).
Rothwell, P. M. et al. Prognostic significance of visit-to-visit variability, maximum systolic blood pressure, and episodic hypertension. The Lancet 375, 895–905 (2010).
Wei, F. F. et al. Beat-to-beat, reading-to-reading, and day-to-day blood pressure variability in relation to organ damage in untreated chinese. Hypertension 63, 790–796 (2014).
Johnson, R. A., Wichern, D. W. et al. Applied multivariate statistical analysis vol. 5 (Prentice hall Upper Saddle River, NJ, 2002).
Knapp, T. R. Canonical correlation analysis: A general parametric significance-testing system. Psychological Bulletin 85, 410–416 (1978).
Benjamini, Y. & Hochberg, Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. Journal of the Royal Statistical Society B 57, 289–300 (1995).
Cinthio, M. et al. Longitudinal movements and resulting shear strain of the arterial wall. American journal of physiology. Heart and circulatory physiology 291, H394–402 (2006).
Yli-Ollila, H., Laitinen, T., Weckström, M. & Laitinen, T. Axial and radial waveforms in common carotid artery: An advanced method for studying arterial elastic properties in ultrasound imaging. Ultrasound in medicine & biology 39, 1168–1177 (2013).
Corretti, M. C. et al. Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery: A report of the international brachial artery reactivity task force. Journal of the American College of Cardiology 39, 257–265 (2002).
Gemignani, V., Faita, F., Ghiadoni, L., Poggianti, E. & Demi, M. A system for real-time measurement of the brachial artery diameter in B-mode ultrasound images. IEEE Trans. Med. Imag. 26, 393–404 (2007).
Asayama, K. et al. Home blood pressure variability as cardiovascular risk factor in the population of ohasama. Hypertension 61, 61–69 (2013).
Mancia, G. et al. Relation between blood pressure variability and carotid artery damage in hypertension: baseline data from the European Lacidipine Study on Atherosclerosis (ELSA). Journal of hypertension 19, 1981–1989 (2001).
Ngim, C. A., Rahman, A. R. A. & Ibrahim, A. Pulse wave velocity as an index of arterial stiffness: A comparison between newly diagnosed (untreated) hypertensive and normotensive middle-aged Malay men and its relationship with fasting insulin. Acta Cardiologica 54, 277–282 (1999).
Svedlund, S. & Gan, L. M. Longitudinal wall motion of the common carotid artery can be assessed by velocity vector imaging. Clinical Physiology and Functional Imaging 31, 32–38 (2011).
Zhang, M. et al. Factors associated with blood pressure response to the cold pressor test: The GenSalt study. American Journal of Hypertension 26, 1132–1139 (2013).
Trémollières, F. A., Pouilles, J.-M., Cauneille, C. & Ribot, C. Coronary heart disease risk factors and menopause: A study in 1684 French women. Atherosclerosis 142, 415–423 (1999).
Miller, A. M., Wilbur, J., Chandler, P. J. & Sorokin, O. Cardiovascular Disease Risk Factors and Menopausal Status in Midlife Women from the Former Soviet Union. Women & Health 38, 19–36 (2003).
Manbachi, A., Hoi, Y., Wasserman, B. A., Lakatta, E. G. & Steinman, D. A. On the shape of the common carotid artery with implications for blood velocity profiles. Physiological measurement 32, 1885–97 (2011).
Antunes, R. F., Kaski, J. C. & Dumitriu, I. E. The role of costimulatory receptors of the tumour necrosis factor receptor family in atherosclerosis. BioMed Research International 2012 (2011).
Acknowledgements
We gratefully acknowledge the volunteers who participated in our study. This work was supported in part by Shenzhen Innovation Funding (SGLH20150213143207911, JCYJ20151030151431727), Guangdong Image-guided Therapy Innovation Team (2011S013), The national Key research and Development Program of China (2016YFC1300302, 2016YFC1301700) and the National Natural Science Foundation of China (No. 61175046, No. 61203290, and No. 61402006).
Author information
Authors and Affiliations
Contributions
C.X., Z.G., Z.Y., H.Z., X.D. and S.L. conceived and designed the experiments. C.X., W.W., X.L. performed the experiments. C.X., G.L., Z.G. analyzed the data. C.X. and Z.G. contributed reagents/materials/analysis tools. C.X., Z.G., Z.Y. and H.Z. wrote the paper. X.L. and H.X. provided the data. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Xu, C., Xiong, H., Gao, Z. et al. Beat-to-Beat Blood Pressure and Two-dimensional (axial and radial) Motion of the Carotid Artery Wall: Physiological Evaluation of Arterial Stiffness. Sci Rep 7, 42254 (2017). https://doi.org/10.1038/srep42254
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep42254
This article is cited by
-
Simulation of phase contrast angiography for renal arterial models
BioMedical Engineering OnLine (2018)
-
Novel blood pressure and pulse pressure estimation based on pulse transit time and stroke volume approximation
BioMedical Engineering OnLine (2018)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.