Abstract
Study design:
This study was designed as a comparative cross-sectional cross-over trial on children performing clean intermittent catheterization (CIC) with reused catheters for 1 or 3 weeks.
Objectives:
To determine the incidence of symptomatic urinary tract infection (UTI) and bacteriuria (defined as colony count of ⩾105 colony forming units per ml of a single strain of organism) in these two different frequencies of catheter change.
Setting:
Multidisciplinary children’s neurogenic bladder clinics at two tertiary care hospitals in Kuala Lumpur Malaysia.
Methods:
Forty children aged between 2 and 16 years performing CIC for at last 3 years were recruited. Medical and social data were obtained from case files. Baseline urine cultures were taken. All children changed CIC catheters once in 3 week for the first 9 weeks followed by once a week for the next 9 weeks. Three-weekly urine cultures were obtained throughout the study. Standardization of specimen collection, retrieval and culture was ensured between the two centers.
Results:
At baseline, 65% of children had bacteriuria. This prevalence rose to 74% during the 3-weekly catheter change and dropped to 34% during the weekly catheter change (Z-score 6.218; P<0.001). Persistence of bacteriuria (all three specimens in each 9-week period) changed significantly from 60 to 12.5%, respectively (P<0.005). There was no episode of UTI during the 18-week study period.
Conclusion:
Reuse of CIC catheters for up to 3 weeks in children with neurogenic bladders appears to increase the prevalence of bacteriuria but does not increase the incidence of symptomatic UTI.
Similar content being viewed by others
Introduction
Children with neurogenic bladders comprise mainly those born with congenital defects such as spina bifida and sacral agenesis, and a few with spinal cord injury or disease. The majority of these newborns have normal upper urinary tracts. However, studies have shown that in those with neurogenic bladders without therapeutic intervention, 50–60% will develop progressive renal impairment mainly because of the recurrent urinary tract infections (UTI) and high bladder pressures.1, 2 Drawing from the experience of adult patients with spinal cord injury, the introduction of clean intermittent catheterization (CIC) by Lapides et al.3 in 1972, has revolutionized the management of neurogenic bladders in children and has led to the preservation of renal function as well as improved quality of life by achieving urinary dryness by school age.4
Intermittent catheterization is the method of choice for emptying the bladder in cases of neurogenic bladder dysfunction. To date, there is no consensus on the ideal technique or type of catheter for intermittent catheterization. The basic principles are as follows: the catheter should be introduced in a non-infecting and atraumatic way;5 it should be removed when the entire collection of urine has been emptied from the bladder; and it should be performed at regular intervals several times a day. In the majority of cases a clean technique is all that is required. When resources are limited, catheters have been known to be reused and this has been the case in many developing countries.6 Our literature review indicates that to date, there has been no study, trial or guideline suggesting how often a reused catheter needs to be replaced.
In Malaysia there are two well-established multidisciplinary clinics, Institute Paediatrics Hospital Kuala Lumpur and Universiti Kebangsaan Malaysia Medical Centre; which provide services to children with neurogenic bladders from all over the country. Initially catheters were reused for up to 1–2 weeks in both centers, but over the years the Institute Paediatrics Hospital Kuala Lumpur patients have reduced the frequency of their catheter changes to 3-weekly. When reused, there is potential for increase in the prevalence of bacteriuria and symptomatic UTI (sUTI). However, Van Hala et al.7 in his study on adults showed that reused catheters compared with single use catheters did not increase the likelihood of UTIs. With this in mind, we set out to determine the frequency of UTI in our population of children with neurogenic bladder who reused catheters for up to 3 weeks and compare it with the frequency of UTI in those reusing catheters for 1 week.
Materials and methods
Study population
This is a comparative cross-sectional cross-over trial on children with neurogenic bladders attending these two multidisciplinary clinics in Kuala Lumpur. The study was conducted between November 2012 and May 2013. Children aged between 1 and 18 years with a diagnosis of neurogenic bladder because of spina bifida, sacral agenesis, spinal cord injury or stable spinal cord disease who were performing CIC per urethra at least three times a day for at least 6 months prior to the recruitment and who consented to the study were elgible for inclusion. Children with neurogenic bladders due to other causes (for example, malignant disease or progressive spinal cord disease) and those performing CIC through a Mitrofanoff channel or practising overnight drainage were excluded. Children living beyond a 30-mile radius were also excluded as it was not possible to obtain urine specimens from these patients and deliver to the laboratory within the expected time frame. All healthcare needs of the patients were funded by the government and the cost of extra catheters was borne by the study grant.
Study design
Patients were recruited as their own controls, all starting with a frequency of 3-weekly catheter change for 9 weeks followed by weekly catheter change for another 9 weeks. Patients were required to provide urine specimens once every 3 weeks for urine culture and microscopy, obtained during early morning CIC on the day of their catheter change (that is, with a new catheter). The specimen was deemed unsuitable for culture if kept at room temperature and delivered to the hospital laboratory beyond 2 h of the time of collection. The preferred method was to store the sample in an ice pack and hence it could still be cultured within 24 h from the time of collection. For the purpose of this study, transport of the urine sample was facilitated by providing patients with an ice pack and a styrofoam box in which the urine specimen bottle was placed. A courier service was arranged to facilitate transport to hospital and culture of urine within 24 h of obtaining the urine by CIC. In both of our laboratories, the standard practice followed was inoculation and incubation of the urine on CLED (Starplex Scientific INC, Etobicoke, ON, Canada) blood agar plate.
Prior to commencement of the study, a baseline urine specimen was obtained and those with sUTI were treated and urine re-cultured. Enrolment was done only when the UTI was cleared or the patient remained asymptomatic (Figure 1).
Sample size
Getliffe et al.8 in their review of current evidence for the relationship of reused catheters and the incidence of UTIs reported two studies with 37 and 53% sUTI, defined as >105 colony forming units per ml of a single organism, in patients using clean reused catheters, thus giving an average of ~46%. There have been no studies on the frequency of UTIs in our patient cohort, and hence we used an estimated rate of 30% as reported figures were deemed to be too high. To achieve a power of 80% and a statistical significance of 5% the sample size required was 38 patients.
Definitions and terminology
Asymptomatic bacteriuria (ABU) was defined as the presence of significant bacteriuria in a patient without signs or symptoms referable to the urinary tract. Several different definitions of bacteriuria are found in the literature.9, 10, 11 For the purpose of this study, the definition of bacteriuria is taken as a colony count of ⩾105 colony forming units per ml of a single strain of organism in the absence or presence of pyuria. This is in keeping with the clinical practice guidelines of the Infectious Diseases Society of America12 and the standard operating procedure of the microbiology laboratories of both participating hospitals.
The Infectious Diseases Society of America guidelines define sUTI as a positive urine culture of ⩾105 colony forming units per ml of a single type of ‘usual pathogen’ with pyuria of ⩾10 leukocytes per high-power field and with any of the following symptoms: fever (⩾38 °C), general malaise, increased spasticity and/or autonomic dysreflexia characterized by flushing, sweating and an increase in blood pressure. ‘Usual pathogens’ were defined as Escherichia coli, Enterobacteriaceae, Enterococcus species, coagulase negative Staphylococcus and group B Streptococcus.
Statistical analysis
Statistical analysis was performed using SPSS for Windows, version 20 (SPSS Inc, Chicago, IL, USA). The X2-test and Fischer’s exact test were used to determine the statistical significance of the incidence of sUTI and ABU between the two different frequencies of catheter change. Multiple logistic regression was performed using the ‘enter’ method to determine factors contributing to the persistence of ABU. A P-value <0.05 was considered statistically significant.
Ethics
Ethics approval was obtained from the Medical Research and Ethics committee of the Universiti Kebangsaan Malaysia Medical Centre and from the National Medical Research Registry of the Ministry of Health (for the Institute Paediatrics Hospital Kuala Lumpur). A research grant was allocated from the Universiti Kebangsaan Malaysia Medical Centre (FF-059-2011) for the cost of extra catheters and for the courier service.
Results
A total of 40 children with neurogenic bladder, aged between 2 and 16 years, were recruited from the two centers.
All recruited patients completed the 18-week study. Table 1 shows the socio-demographic and medical characteristics of the children. The majority of patients (90%) had spina bifida. The one patient with acute demyelinating encephalomyelitis had no progression of disease over the previous 3 years. The most common anatomical sites for the spina bifida lesions were the lumbo-sacral and sacral regions.
The majority of children had performed CIC for at least 3 years with 55% doing it for more than 5 years. Only 11 children were performing self-catheterization, whereas 42.5% were still totally dependent on a parent or caretaker and another 30% performed it with assistance. Nine of the children performing self-CIC were aged between 12 and 16 years; one was aged 11 years and one was aged 8 years. Thirty-five of the 40 children followed the recommended frequency of five catheterisations per day; however, only 30% were reliably dry between CICs.
Only 12.5% of children had reflux disease and notably, none had Grade IV or V reflux which carries a higher incidence of UTI. Among them, only nine patients had any evidence of bladder trabeculation.
At the time of recruitment, baseline urine cultures showed that 26 out of 40 children (65%) had positive cultures but all patients were asymptomatic (ABU). Despite this, there was no episode of sUTI in any of the patients throughout the 18-week study period, either during 3-weekly catheter change or during weekly catheter change.
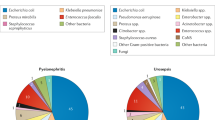
The prevalence of ABU rose to 74.2% (89/120 specimens) during the 3-weekly catheter change and dropped to 34.2% (41/120 specimens) during the weekly catheter change (Table 2), indicating a significant change in the prevalence rates on the Z-test (Z-score of 6.218; P<0.001). During the 3-weekly catheter change, 60% of patients had a persistence of ABU (defined as positive cultures in all three of the urine specimens collected over nine weeks) compared with only 12.5% of patients during the weekly catheter change. This difference was statistically significant on X2-analysis (P<0.005). Multiple logistic regression was then used to analyse factors contributing to the persistence of ABU during the 3-weekly catheter change period. Factors entered were age, gender, duration of CIC, person who performs the CIC, CIC performed during school hours, number of CICs per day, use of diapers, use of prophylactic antibiotics, use of anticholinergics, presence of bladder trabeculation and presence of reflux, soiling and constipation. It was noted that presence of bladder trabeculation increased the persistence of ABU, whereas the use of prophylactic antibiotics decreased the persistence of ABU (Table 3).
Discussion
Bacteriuria is common among patients with neurogenic bladders who are performing CIC. When resources are limited, catheters are often reused. However, it is not clear how frequently a catheter can be reused without leading to the development of an sUTI.
Schlager et al.,11 in their weekly urinary surveillance of 14 children over 6 months, detected five with sUTI. In another study in 2001, the same researchers found no difference between the incidence of sUTI whether using a single sterile catheter or using a clean catheter reused for up to five times.13 However the sample consisted of only 10 patients. In our hospital practice of reusing catheters for 1, 2 or even 3 weeks, the risk for sUTI is potentially increased. However, in this 18-week follow-up study, none of our 40 patients developed an sUTI. It is possible that patient’s adherence to the ‘clean technique’ during this time was stricter as they and their caregivers knew that they were being surveyed.
Literature reports on the prevalence of ABU in spina bifida children performing CIC vary from 40 to 61%.14, 15 In keeping with these reports our prevalence rate was 65% at baseline. However, when catheters were reused for up to 3 weeks, this prevalence rose and it dropped during the more frequent weekly changes, suggesting that the frequency of catheter changes does influence the rate of ABU. Furthermore, our patients also showed a persistence of ABU during the 3-weekly catheter change, which was significantly affected by the presence of bladder trabeculation. However, the statistical significance of this finding is questionable as indicated by the wide confidence intervals and can perhaps be explained by the fact that the sample size was calculated for the incidence of UTIs and not for the prevalence of ABU.
However, despite the persistence of ABU in the 3-weekly catheter change, it is clinically important to note that none of these children developed sUTI. This finding further supports the recent proposal that bacterial colonization of the urinary tract may in fact be advantageous and may protect against invasion by other more virulent bacteria.16
In summary, we conclude that our practice of reusing of CIC catheters can be continued for up to at least 3 weeks without causing sUTIs. Second, 3-weekly catheter change appears to lead to the persistence of ABU and this may be providing some protection against sUTI. This evidence is particularly important for medical professionals managing patients with neurogenic bladder in communities and healthcare systems with limited resources.
DATA ARCHIVING
There were no data to deposit.
References
Bauer SB, Hallett M, Khoshbin S, Lebowitz RL, Winston KR, Gibson S et al. Predictive value of urodynamic evaluation in newborns with myelodysplasia. JAMA 1984; 252: 650–652.
Zegers Bas SHJ, Winkler-Seinstra PLH, Uiterwaal CSPM, de Jong Tom VPM, Kimpen Jan LL, de Jong-de Vos van Steenwijk Catharine CE . Urinary tract infections in children with spina bifida. Pediatr Nephrol 2009; 24: p783.
Lapides J, Diokno AC, Silber SM, Loner BS . Clean intermittent self-catheterization in the treatment of urinary tract disease. J Urol 1972; 107: 458–461.
Verpoorten C, Buyse GM . The neurogenic bladder: medical treatment. Pediatr Nephrol 2008; 23: 717–725.
Wyndaele JJ . Intermittent cathetrization: which is the optimal technique? Spinal Cord 2002; 40: 432–437.
Abeygunasekera AM . Clean intermittent catheterisation. Ceylon Med J 2004; 49: 107–109.
Van Hala S, Nelson VS, Hurvitz EA, Panzi A, Bloom DA, Ward MJ . Bladder management in patients with pediatric onset neurogenic bladders. J Spinal Cord Med 1997; 20: 410–415.
Getliffe K, Fader M, Allen C, Pinar K, Moore KN . Current evidence on intermittent catheterization. Sterile single-use catheters or clean reused catheters and the incidence of UTI. J Wound Ostomy Continence Nurs 2007; 34: 289–296.
National Institute of Disability and Rehabilitation Research. The prevention and management of urinary tract infections among people with spinal cord injuries. National Institute of Disability and Rehabilitation Research Consesnsus Statement. 1992. J Am Paraplegia Soc 1992; 15: 194–204.
Urinary Tract Infection in Children-Diagnosis, Treatment and Long-Term Managment. National Institute for Health and Clinical Excellence (NICE) Clinical Practice Guidelines 2007.
Schlager TA, Dilks S, Trudell J, Whittam TS, owen Hendley J . Bacteriuria in children with neurogenic bladder treated with intermittent catheterization: natural history. J Pediatr 1995; 126: 490–496.
Hooton TM, Bradley SF, Cardenas DD, Colgan R, Geerlings SE, Rice JC et al. Diagnosis, prevention, and treatment of catheter-associated urinary tract infection in adults: 2009 International Clinical Practice Guidelines from the Infectious Diseases Society of America. Clin Infect Dis 2010; 50: 625–663.
Sclagger TA, Clark MT, Anderson S . Effect of a single-use sterile catheter for each void on the frequency of bacteriuria in children with neurogenic bladder on intermittent catheterization for bladder emptying. Pediatrics 2001; 108: 1–4.
Zegers Bas SHJ, Uiterwaal CSPM, Verpoorten CC, Christaens MMH, Kimpen JLL, deJong-de Vos van Steenwijk CCE et al. Home screening for bacteriuria in children with spina bifida and clean intermittent catheterization. BMC Infect Dis 2012; 12: 264–268.
Schlager TA, Hendley JO, Wilson RA, Simon V, Whittam TS . Correlation of periurethral bacterial flora with bacteriuria and urnary tract infection in children with neurogenic bladder receiving intermittent catheterization. Clin Infect Dis 1999; 28: 346–350.
Darouiche RO, Green BG, Donovan WH, Chen D, Schwartz M, Merritt J et al. Multi-center randomized controlled trial of bacterial interference for prevention of urinary tract infection in patients with neurogenic bladder. Urology 2011; 78: 341–347.
Acknowledgements
The authors acknowledge the following collaborators: Dr Ramliza Ramli and Assoc Prof SW Wong of the Universiti Kebangsaan Malaysia Medical Centre; Drs YN Lim, YC Yap and Susan Woo of the Institute Paediatrics Hospital Kuala Lumpur for their assistance in this study; and Prof LC Ong for her advice and guidance during the development of the study protocol. The study was sponsored by Universiti approved research study grant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Kanaheswari, Y., Kavitha, R. & Rizal, A. Urinary tract infection and bacteriuria in children performing clean intermittent catheterization with reused catheters. Spinal Cord 53, 209–212 (2015). https://doi.org/10.1038/sc.2014.210
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2014.210
This article is cited by
-
Disability and sustainability: reusable versus single-use catheters for persons with neurogenic bladder due to spinal cord injury
Spinal Cord Series and Cases (2020)
-
Neurogenic Bladder: Recurrent Urinary Tract Infections—Beyond Antibiotics
Current Bladder Dysfunction Reports (2018)