Abstract
Objectives:
Despite many years of research, there is currently no treatment available that results in major neurological or functional recovery after traumatic spinal cord injury (tSCI). In particular, no conclusive data related to the role of the timing of decompressive surgery, and the impact of injury severity on its benefit, have been published to date. This paper presents a protocol that was designed to examine the hypothesized association between the timing of surgical decompression and the extent of neurological recovery in tSCI patients.
Study design:
The SCI-POEM study is a Prospective, Observational European Multicenter comparative cohort study. This study compares acute (<12 h) versus non-acute (>12 h, <2 weeks) decompressive surgery in patients with a traumatic spinal column injury and concomitant spinal cord injury. The sample size calculation was based on a representative European patient cohort of 492 tSCI patients. During a 4-year period, 300 patients will need to be enrolled from 10 trauma centers across Europe. The primary endpoint is lower-extremity motor score as assessed according to the ‘International standards for neurological classification of SCI’ at 12 months after injury. Secondary endpoints include motor, sensory, imaging and functional outcomes at 3, 6 and 12 months after injury.
Conclusion:
In order to minimize bias and reduce the impact of confounders, special attention is paid to key methodological principles in this study protocol. A significant difference in safety and/or efficacy endpoints will provide meaningful information to clinicians, as this would confirm the hypothesis that rapid referral to and treatment in specialized centers result in important improvements in tSCI patients.
Similar content being viewed by others
Introduction
In his seminal paper on the treatment of spinal injuries published in 1905, Dr Burrell postulated two important assumptions related to the role of surgical decompression in traumatic spinal cord injury (tSCI).1 Related to the ‘window of opportunity’ for surgical decompression, his first assumption was ‘that if pressure on the cord is allowed to remain for many hours, irreparable damage to the cord may take place’. In his second assumption Burrell refers to the ‘window of severity’ for surgical decompression: ‘that unless it is perfectly clear that the cord is irremediably damaged an open operation to establish the condition of the cord and to relieve pressure is imperative as soon as surgical shock has been recovered from’. Nowadays, more than 100 years after Burrell’s findings, the role of surgical treatment in tSCI is well recognized.2, 3 However, no conclusive data related to the role of the timing of decompressive surgery, and the impact of injury severity on its benefit, have been published to date.
The contemporary debate on the optimal timing of decompression in tSCI is based on a more recent concept that distinguishes primary from secondary mechanisms of injury.4 The primary mechanism refers to the initial cord lesion resulted from the physical trauma to the tissue caused by a displacement of the surrounding spinal column. The primary mechanism in turn initiates a cascade of secondary injury mechanisms including ischemia, edema, increased excitatory amino acids and lipid peroxidation.4 Pre-clinical data support the theory that persistent compression of spinal cord represents a cause of secondary injury and thus may be potentially reversible.5, 6 The National Acute Spinal Cord Injury Studies were the first large clinical studies supporting the concept of secondary mechanism of injury.7, 8, 9 The accumulation of both experimental and clinical study results increasingly supported the potential therapeutic role of acute surgical decompression in tSCI.10
Dr Furlan et al.3 recently published a review of clinical studies on the efficacy of surgical decompression in tSCI patients. Although the included studies showed some conflicting findings, a modified Delphi process led the authors to the conclusion and recommendation that surgical decompression of the injured spinal cord should be performed within 24 h after injury when medically feasible.3 It was noted that this recommendation was based on 20 ‘level-4 evidence’ studies and 2 ‘level-2b evidence’ studies.11 But what could be the explanation for the lack of robust evidence on such a burning issue in the management of spinal trauma patients?
With a reported incidence rate ranging from 10.4 to 83 cases per million population worldwide,12 tSCI is not only relatively uncommon, but is also markedly heterogeneous in terms of anatomic level and severity.13 Another aspect limiting the feasibility of conducting a surgical randomized controlled trial on the acute management of tSCI is the difficulty to recruit potentially eligible subjects in the early hours after the injury. The foremost explanation for this is the required transfer time to specialized trauma centers.14 Given these and other practical and ethical limitations,15, 16 a well-powered prospective, comparative cohort study would be the second best study design of choice.
The aim of this article is to describe a protocol that was designed to examine the hypothesized association between the timing of surgical decompression and the extent of neurological recovery in tSCI patients. The purpose of this observational study is to determine the safety, effectiveness and feasibility of early surgical treatment for tSCI among patients with a traumatic spinal column injury. The primary aim of this study is to determine whether acute (<12 h) surgical treatment results in better neurological recovery 12 months after injury when compared with non-acute (>12 h, <2 weeks) surgical treatment in tSCI patients.
Materials and methods
Study design
A Prospective, Observational European Multicenter comparative cohort study, which has the acronym ‘SCI-POEM’, will be undertaken.
Setting and patient recruitment
Setting and investigational sites
Patients will be identified and recruited in European level I and II trauma centers. To diminish the putative confounding effect of differences in perioperative care and acute rehabilitation, the number of tSCI patients treated at participating investigational sites needs to be at least 10 per year during the past 3 years. Furthermore, to aim for high-quality outcome research, participating investigational sites have to ensure that physicians obtain a complete neurological examination before surgical intervention and that designated personnel are willing to attend outcome measurement instructional courses. As there is (1) conflicting evidence on the therapeutic efficacy of methylprednisolone administration in tSCI patients and (2) increasing evidence on complications associated with its administration,17, 18, 19 it was decided to exclude those trauma centers that administer methylprednisolone to acute tSCI patients per protocol.
Patient recruitment, eligibility criteria and informed consent
All adult patients admitted with a traumatic spinal column injury to one of the participating hospitals will be assessed for eligibility. Upon admission to hospital, all trauma patients undergo clearance protocols of the cervical20 and thoracolumbar21 spine. In line with common practice, a mandatory computed tomography (CT) scan is performed in all patients where the spinal column cannot be cleared. Additional magnetic resonance imaging (MRI) of the spine is not mandatory and left to the preference of the treating physician. Patients with a detected, significant spinal column injury undergo a detailed neurological examination. All patients with a significant traumatic spinal column injury and concomitant spinal cord injury are considered eligible for inclusion in the SCI-POEM study. A detailed list of eligibility criteria is presented in Table 1.
The treating spinal surgeon assesses the eligibility for inclusion in this study. Eligible patients are approached by a local study coordinator who is not involved in the treatment-decision making and inquires about their interest of participating in this study. Because of the observational nature of this study, written consent—or verbal assent—may also be obtained days after the, often hectic, early phase after the injury. On the basis of previous experience, the recruitment, or allocation, ratio for acutely and non-acutely decompressed patients is estimated to be 1:2.
Treatment protocol and follow-up
General treatment regimen
During both the acute phase and early rehabilitation, all tSCI patients will be treated at each institution per standard of care.22 All patients are managed according to advanced trauma life support principles. During the first 2 weeks after injury, hemodynamic and respiratory functions are monitored and supported to reach appropriate levels of cord perfusion and oxygenation.23 Special attention is given to the prevention of respiratory adverse events, thromboembolic events, urogenital adverse events, bowel obstruction, pressure sores, muscle contractures and periarticular ossifications.24, 25 Dependent on the level and severity of injury, individually tailored rehabilitation programmes will vary in focus and intensity.
Treatment protocol: Surgical treatment regimen
Depending on the preference of the spinal surgeon, the following surgical approaches are performed consistent with the standard of care provided by each of the participating hospitals:
-
Closed: Closed reduction and external fixation
-
Open: Posterior approach
-
Open: Anterior approach
-
Open: Circumferential approach (one or two stage)
If an open approach follows a closed approach, details of both approaches are recorded. If applicable, additional details of closed and open surgeries (for example, duration of traction, performance of a laminectomy) are also collected. The type and duration of postoperative spinal immobilization and perioperative pharmaceutical interventions are also recorded.
The following information related to the principle exposure under study, the timing of surgical decompression, will be documented:
-
Date, time and location of injury
-
Date and time of arrival of patient in participating hospital
-
Date, time and method of surgical decompression
The timing of decompression is defined as the date and time of the applied intervention leading to a successful decompression as confirmed with MRI. A successful decompression is defined as either when the transverse spinal area (TSA)26 of the injured level is at least 90% of the average TSA of the rostral and caudal levels, or as presence/restoration of hyperintense cerebrospinal fluid signal around the spinal cord on transverse T2 MR images. To gain additional information on the feasibility of acute surgical decompression for tSCI, details on delays in patient transfer, diagnostic work-up and treatment will be documented.
Follow-up and data collection
Follow-up assessments will take place at routine visits 3, 6 and 12 months after injury. Source data collection will be performed by a local research coordinator at each participating hospital using paper case-record forms. After the initial data collection, the source data will be transferred from case-record forms onto the electronic data capturesystem in a de-identified manner and latest within 14 calendar days of study enrollment and follow-up measurements. De-identified DICOM images will be transferred to the clinical research organization (CRO) and stored on secure operating servers.
Study endpoints and adverse events (AEs)
Primary endpoint
The primary outcome is the:
-
Lower-extremity motor score (LEMS) as assessed according to the ‘International standards’ for neurological and functional classification of SCI at 12 months after injury
All neurological outcomes will be assessed according to the ‘International standards’ for neurological and functional classification of SCI developed by the American Spinal Injury Association (ASIA) committee.27 The International standards provide a standardized quantitative description of the neurological level of injury and sensorimotor function above and below this level.
Motor function testing according to International standards encompasses 10 bilateral myotomes, more specifically C5–T1 and L2–S1, corresponding to the five key muscle groups in each of the four limbs. The total motor score can be divided into two subscales, an upper-extremity motor score (UEMS) and a LEMS, each consisting of a total of 10 key muscles.28 Motor score testing of the key muscles is graded on a five-point scale adapted from the Medical Research Council scale. In a recent review, Furlan et al.29 demonstrated a high reproducibility and a good responsiveness to change of the International standards as a whole.
Secondary endpoints
The secondary outcomes are the:
-
LEMS as assessed according to the ‘International standards’ at 3 and 6 months after injury
-
UEMS in tetraplegic patients as assessed according to the ‘International standards’ at 3, 6 and 12 months after injury
The LEMS and UEMS will be assessed and scored as described above.
-
Aggregated sensory score as assessed according to the ‘International standards’ at 3, 6 and 12 months after injury
Sensory examination comprises testing of what are known as key points in each of the 28 dermatomes on both the left and right sides of the body. The key points correspond with a defined area of skin in each dermatome where overlapping innervation to adjacent dermatomes is at a minimum, thereby making these areas most suitable for testing the function of each specific dermatome. The dermatomes extend from level C2 to S5, where S4 and S5 are considered as one dermatome. Each key point, including the perianal region, is tested for light touch (with a cotton tip applicator or similar object) and pain (using a pin or similar object). Sensory function is graded as follows: normal=2; impaired/distorted=1; absent=0; not testable=NT. The latter may be due to a local injury, amputation or a cast covering the area.27
-
The ASIA/International Spinal Cord Society neurological standard scale (ASIA Impairment Scale, AIS) at 3, 6 and 12 months after injury
On the basis of the sensorimotor scores as assessed according to the ‘International standards’, the level and the severity of the SCI can be determined. The scale most commonly used to classify the severity of the injury is the ASIA/ISCoS neurological standard scale AIS. Using the AIS the severity of the injury can be categorized into five grades (A–E, see Table 2).27 As previous studies indicated that the AIS may not be responsive enough to detect small neurological improvements,30 this commonly applied outcome measure was not applied as a primary outcome measure in the current study.
-
The Spinal Cord Independency Measure III (SCIM-III) at 3, 6 and 12 months after injury
The SCIM is a disability scale that specifically addresses patients with spinal cord lesions describing their ability to accomplish activities of daily living. It has undergone two revisions,31, 32 the most recent one resulting in the SCIM-III.32 The SCIM-III consists of 19 subitems and cover the following three main categories (1) self-care, (2) respiration and sphincter management, and (3) mobility. Main areas and subitems are weighted according to their assumed clinical relevance in relation to the overall activity of the SCI population. The maximal total score of the SCIM-III amounts to 100 points. Previous studies demonstrated excellent reliability and construct validity of the SCIM-III.32, 33, 34
-
Fracture consolidation at 6 months after injury
To improve the understanding of the effect of post-traumatic spinal column characteristics on neurological and functional outcomes, several routine spinal column outcome measures will be recorded. A fracture is defined as healed if there is complete or almost complete resolution of the fracture line or if there are visible bony trabeculations crossing the fracture line.35 Non-union, or pseudoarthrosis, is defined as failure of fracture consolidation 6 or more months after injury. As no definitive method that defines fracture healing has been published to date, there is currently no consensus as to which is the best imaging study to use to affirm the presence of union or pseudarthrosis. Despite absence of a gold standard, presence of bony trabeculations as discerned on conventional or CT imaging is considered the next best approach.
-
Sagital alignment at 3, 6 and 12 months after injury
The sagital alignment of the spinal column will be assessed according to the Cobb angle method. The Cobb angle is the angle between the superior endplate of the vertebral body one level above the injured vertebral body to the inferior endplate of the vertebral body one level below.36 Kuklo et al.36 demonstrated a good reproducibility and responsiveness to change of the Cobb angle method.
-
Vertebral height at 3, 6 and 12 months after injury
The anterior vertebral height is the distance between the anterosuperior and anteroinferior corner of the vertebral body as described by Isomi et al.37 The vertebral height ratio can be calculated by dividing the anterior vertebral height by the posterior vertebral height, which is defined as the distance between the posterosuperior and posteroinferior corners of the vertebral body. No data regarding the validity, reproducibility or responsiveness of these measures have been published to date.
-
Spinal canal compromise at 3, 6 and 12 months after injury
The extent of spinal canal encroachment will be determined by measuring the TSA as described by Rasmussen et al.26 The TSA, or total canal cross-sectional area, is defined as the total area of the canal bordered anteriorly by the posterior border of the vertebral body, posteriorly by the convergence of the superior border of the laminae at the midline of the spinous process, and laterally by the medial border of the pedicles.38 The maximum encroachment at the affected level can be expressed as a percentage by dividing the TSA by the average TSA of the unaffected levels rostral and caudal to the level of injury (% Canal encroachment=100—(2TSAInjured/(TSARostral+TSACaudal) × 100)). Although construct validity has been proven,26 no data regarding the reproducibility or responsiveness of the TSA measure have been published to date.
Outcome assessors
Although blinding to important prognostic factors and treatment modalities is theoretically possible, blinding of neurological and functional outcome assessors is not regarded as a feasible option in this study. The number of trained and qualified assessors per investigational site is expected to be low and the bias-prone effect of knowledge of prognostic factors on outcomes is considered to be minimal. Radiologists, however, will be blinded to specific clinical information (severity and level of neurological deficit and timing of surgery) and will examine de-identified medical images independently of treating surgeons.
AEs and safety
AEs are defined as any unfavorable and unintended sign, symptom, disease or clinical event occurring to a subject during the study, whether or not considered related to the intervention under study. The research coordinator of each participating hospital records all AEs on a study worksheet. The worksheet will capture the date of onset, severity, duration, outcome and relationship to the treatment or protocol.
Serious AEs (SAEs) are defined as events that led to a death or led to a serious deterioration in the health of a subject. In case an SAE occurs, the research coordinator is required to notify the principal investigator and to contact the CRO as soon as possible. The research coordinator will report any and all SAE to the institutional review board (IRB) as required.
Anticipated AEs are those that might reasonably be expected, or have previously been reported, to occur in the spinal column injury and spinal cord injury population. These can include, but are not necessarily limited to those outlined and defined in Table 3.
Statistical analyses
Sample size
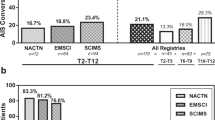
For the sample size calculation we used a representative European patient cohort of 492 tSCI patients (see Table 4), for whom clinical characteristics have been documented in detail in a recent study.39 Given the heterogeneity of recovery patterns in the tSCI population,40 it was decided to stratify the study population into the four AIS categories and to conduct a separate sample size calculation for each AIS grade. Furthermore, given that the primary outcome recovery profile for tetra- and paraplegic patients was remarkably similar in all of the AIS grade groups (data not presented; available upon request), it was decided not to stratify by the ‘level of injury’. The following equation was used to calculate the sample size for each AIS grade group:41

All sample size calculations are based on at least 80% power and 95% certainty. The anticipated therapeutic effects of acute decompression are 7 LEMS points for AIS grade A, 10 LEMS points for AIS grade C and D and 3 LEMS points for AIS grade D. The estimated allocation and drop-out ratios are 1:2 (acute:non-acute) and 1:10, respectively. On the basis of these conditions and estimations the sample sizes were set at 114 AIS grade A patients, 63 AIS grade B patients, 60 AIS grade C patients and 63 AIS grade D patients. This means that the total required study sample is 300 patients.
Analysis
Frequencies and percentages or means and SD will be calculated where appropriate, to describe patient characteristics for the entire cohort and for the two study groups. Patient characteristics will be compared between the two study groups using two-sample t tests for continuous variables and χ2-tests for categorical variables. Within-group changes from baseline to the 3-, 6- and 12-month follow-up assessments will be examined by a paired samples t-test.
Confounding by indication is an inherent limitation of non-randomized comparative studies. Covariate, or patient characteristic, imbalances between the two study groups resulting from selection bias may lead to incorrect estimations of the attributable effect of the timing of surgical decompression on neurological recovery. Analysis of covariance, with adjustment for the propensity score, will be used to adjust for covariates including age, gender, (concomitant) injury characteristics (for example, ISS, fracture classification) and co-morbidities.42, 43, 44, 45 A propensity score is the likelihood of exposure to a treatment, given a subject’s observed covariates, and is estimated by using a logistic regression model of observed covariates with treatment exposure as the outcome variable. The propensity score can be used to balance the covariates in the two groups, and thus reduce the magnitude of selection bias.46 Multiple imputation techniques will be used to replace missing data rather than discarding incomplete records.47
Interim analysis
As both acute and non-acute decompression are current spinal injury management practices, it is expected that the IRBs will advise that repeated interim analyses for safety outcomes are not required. However, a superiority interim analysis will be performed once 50% of participants have reached the primary endpoint.
Study organization
Protocol implementation
The study protocol will be instructed by the CRO study monitor to all designated physicians and paramedical staff through site visits, telephone/audio–video conferences and study progress meetings. Each investigational site will need to nominate at least two physicians and medic staff members for an ‘outcome assessment’ course. Only those assessors who successfully completed the instructional course will be allowed to examine included patients for the current study. All outcome assessors will be provided explanatory documentation and standardized recording forms.
Follow-up compliance
Patients will be followed from the day of inclusion to the study endpoint 12 months after the injury. This will include time while hospitalized, routine standard of care visits (or consultations while in rehabilitation center), unplanned visits and planned routine visits at 3, 6 and 12 months after injury. Patients will receive reminders by (electronic) mail for upcoming study visits. In case a patient does not show up for a follow-up visit, designated local staff will contact the subject to schedule a new visit and to update any changes in residence and contact details.
Monitoring
The CRO will regularly check the study database to identify missing data or unrealistic values. Inconsistencies will be resolved by contacting the participating hospital and asking for clarification or by asking the local research coordinator to contact the subject, subject’s physicians, or querying the subject’s source documents or medical record. In addition, the CRO study monitor will visit each participating hospital to examine recruitment procedures, ensure data quality and monitor compliance with the study protocol.
Data integrity and management
All case-record forms are kept in locked file cabinets in secure areas. De-identified data transfer to the electronic data capture system will be encrypted. The electronic data capture system is located at a secure premise, has restricted access and maintains a continuous advanced mirroring back-up system on secure operating servers.
Ethical aspects and informed consent
Consent will be specifically sought for follow-up participation and the use and storage of de-identified data for the current research project. A local study coordinator will approach eligible subjects and will explain (1) the purpose of the study, (2) the procedures, (3) the risk/benefits, (4) alternatives to participation, (5) and their confidentiality. The study monitor will emphasize that the current non-experimental study does not influence the type or quality of treatment or provided healthcare by any means. Each subject choosing to participate will sign (or will approve a relative to sign) and date an informed consent form. Either in writing or verbally and at all times enrolled patients will have the right to withdraw their consent. A register will be kept of all spinal column injury patients with spinal cord injury who are ineligible, not consenting to participate or withdraw from the study. The reason for ineligibility, not consenting and consent withdrawal will be documented along with the following core patient characteristics: age, gender and level and severity of spinal cord injury.
Given the lack of standard operating procedures for the assessment of non-experimental clinical studies by ethics committees across European countries,48 the need for approval of the current study protocol and consent forms will be checked for each participating investigational site separately.49
Discussion
The conduct of a surgical randomized controlled trial on the acute management of tSCI is a very challenging, if not infeasible, undertaking. For this reason we designed a prospective, comparative cohort study protocol. One of the major limitations of non-randomized comparative studies is the susceptibility to confounding by indication. With use of advanced statistical approaches, including the use of a propensity score, we try to correct and even reduce the magnitude of selection bias.
The diagnostic and prognostic role of MRI in the management of tSCI patients remains a heavily debated topic. Although some specialists perform MRI in all alert patients presenting with signs of spinal cord injury,50 others rely on neurological examination and CT only and order MRI in those cases where neurological findings do not correspond with the injury pattern as discerned on CT images.14 Given this variety in diagnostic work-up, and also the fact that MRI does not provide information relevant for the primary study endpoint under study, pre-decompression MRI is not considered as a mandatory investigation in the current study. This approach will also enable us to compare the time between hospital admission and treatment between institutions with a ‘routine MRI protocol’ and institutions without such a protocol.
To our knowledge, we are the first authors defining the successfulness of a decompression of the traumatic spinal cord in such detail. As opposed to the pre-surgical work-up, MRI is mandatory after the intervention to confirm the successfulness of the decompression. As not all tSCI patients with spinal column injury present with a (continued) compression of the neurological structures, this may be interpreted as an inconsistency in the diagnostic work-up and a limitation of the study design. However, the intention of this study is not to demonstrate to what extent a certain compression of the cord has been decompressed by comparing two MRI series, but rather to demonstrate the effect of the timing of a confirmed decompressed, or non-compressed, spinal cord after the intervention and relate this to neurological outcomes. Nonetheless, an ancillary analysis will be performed in those patients with available pre-surgical MRI to assess the relation between the extent of pre-surgical spinal cord compression and neurological outcomes. Finally, the impact of metal-induced susceptibility artifacts on the accuracy of TSA measurements—due to encoding difficulties in MRI and to beam hardening in CT—warrants careful consideration and optimization of imaging processing.51, 52
It is planned to commence patient recruitment at the first investigational sites autumn 2012. Aiming for a total of 10 participating investigational sites and considering the tSCI incidence rate for each AIS grade specifically, it is expected that the study will take approximately 5 years to complete. At the time of submission of this paper not all participating centers have yet been identified, and funding is still being sought from local and international sources. As reported throughout this study protocol, this prospective, comparative cohort study will adhere to key methodological principles for minimizing bias and reducing the impact of confounders. The findings of this study will be reported according to the STROBE statement.53 A significant difference in safety and/or efficacy endpoints will provide meaningful information to clinicians, as this would confirm the hypothesis that rapid referral and treatment in specialized centers result in important improvements in tSCI patients.
Data archiving
There were no data to deposit.
References
Burrell HL . Fracture of the spine. A summary of all the cases (244) which were treated at the Boston City Hospital from 1864 to 1905. Ann Surg 1905; 42: 481–506.
Fehlings MG, Perrin RG . The timing of surgical intervention in the treatment of spinal cord injury: a systematic review of recent clinical evidence. Spine 2006; 3111 (suppl): S28–S35; discussion S6.
Furlan JC, Noonan V, Cadotte DW, Fehlings MG . Timing of Decompressive Surgery of Spinal Cord after Traumatic Spinal Cord Injury: an Evidence-Based Examination of Pre-Clinical and Clinical Studies. J Neurotrauma 2011; 28: 1371–1399.
Carlson SL, Parrish ME, Springer JE, Doty K, Dossett L . Acute inflammatory response in spinal cord following impact injury. Exp Neurol 1998; 151: 77–88.
Dimar JR, Glassman SD, Raque GH, Zhang YP, Shields CB . The influence of spinal canal narrowing and timing of decompression on neurologic recovery after spinal cord contusion in a rat model. Spine 1999; 24: 1623–1633.
Rabinowitz RS, Eck JC, Harper CM, Larson DR, Jimenez MA, Parisi JE et al. Urgent surgical decompression compared to methylprednisolone for the treatment of acute spinal cord injury: a randomized prospective study in beagle dogs. Spine 2008; 33: 2260–2268.
Bracken MB, Collins WF, Freeman DF, Shepard MJ, Wagner FW, Silten RM et al. Efficacy of methylprednisolone in acute spinal cord injury. JAMA 1984; 251: 45–52.
Bracken MB, Shepard MJ, Collins WF, Holford TR, Young W, Baskin DS et al. A randomized, controlled trial of methylprednisolone or naloxone in the treatment of acute spinal-cord injury. Results of the Second National Acute Spinal Cord Injury Study. N Engl J Med 1990; 322: 1405–1411.
Bracken MB, Shepard MJ, Holford TR, Leo-Summers L, Aldrich EF, Fazl M et al. Methylprednisolone or tirilazad mesylate administration after acute spinal cord injury: 1-year follow up. Results of the third National Acute Spinal Cord Injury randomized controlled trial. J Neurosurg 1998; 89: 699–706.
La Rosa G, Conti A, Cardali S, Cacciola F, Tomasello F . Does early decompression improve neurological outcome of spinal cord injured patients? Appraisal of the literature using a meta-analytical approach. Spinal Cord 2004; 42: 503–512.
Sackett DL, Strauss SE, Richardson WS, Rosenberg W, Haynes RB . Evidence-Based Medicine: How to Practice and Teach EBM. Churchill-Livingstone: Philadelphia, PA, 2000.
Wyndaele M, Wyndaele JJ . Incidence, prevalence and epidemiology of spinal cord injury: what learns a worldwide literature survey? Spinal Cord 2006; 44: 523–529.
Tuszynski MH, Steeves JD, Fawcett JW, Lammertse D, Kalichman M, Rask C et al. Guidelines for the conduct of clinical trials for spinal cord injury as developed by the ICCP Panel: clinical trial inclusion/exclusion criteria and ethics. Spinal Cord 2007; 45: 222–231.
Tator CH, Fehlings MG, Thorpe K, Taylor W . Current use and timing of spinal surgery for management of acute spinal surgery for management of acute spinal cord injury in North America: results of a retrospective multicenter study. J Neurosurg 1999; 911 (suppl): 12–18.
Garcia J, Elbourne D . Snowdon C. Equipoise: a case study of the views of clinicians involved in two neonatal trials. Clin Trials 2004; 1: 170–178.
Carr AJ . Evidence-based orthopaedic surgery: what type of research will best improve clinical practice? J Bone Joint Surg Br 2005; 87: 1593–1594.
Ito Y, Sugimoto Y, Tomioka M, Kai N, Tanaka M . Does high dose methylprednisolone sodium succinate really improve neurological status in patient with acute cervical cord injury?: a prospective study about neurological recovery and early complications. Spine 2009; 34: 2121–2124.
Lee HC, Cho DY, Lee WY, Chuang HC . Pitfalls in treatment of acute cervical spinal cord injury using high-dose methylprednisolone: a retrospect audit of 111 patients. Surg Neurol 2007; 68(Suppl 1): S37–S41 discussion S-2..
Suberviola B, Gonzalez-Castro A, Llorca J, Ortiz-Melon F, Minambres E . Early complications of high-dose methylprednisolone in acute spinal cord injury patients. Injury 2008; 39: 748–752.
Como JJ, Diaz JJ, Dunham CM, Chiu WC, Duane TM, Capella JM et al. Practice management guidelines for identification of cervical spine injuries following trauma: update from the eastern association for the surgery of trauma practice management guidelines committee. J Trauma 2009; 67: 651–659.
Inaba K, DuBose JJ, Barmparas G, Barbarino R, Reddy S, Talving P et al. Clinical examination is insufficient to rule out thoracolumbar spine injuries. J Trauma 2011; 70: 174–179.
Stevens RD, Bhardwaj A, Kirsch JR, Mirski MA . Critical care and perioperative management in traumatic spinal cord injury. J Neurosurg Anesthesiol 2003; 15: 215–229.
Bernhard M, Gries A, Kremer P, Bottiger BW . Spinal cord injury (SCI)--prehospital management. Resuscitation 2005; 66: 127–139.
Kirshblum SC, Priebe MM, Ho CH, Scelza WM, Chiodo AE, Wuermser LA . Spinal cord injury medicine. 3. Rehabilitation phase after acute spinal cord injury. Arch Phys Med Rehabil 2007; 88(3 Suppl 1): S62–S70.
Jia X, Kowalski RG, Sciubba DM, Geocadin RG . Critical Care of Traumatic Spinal Cord Injury. J Intensive Care Med, (e-pub ahead of print 11 April 2011).
Rasmussen PA, Rabin MH, Mann DC, Perl JR, Lorenz MA, Vrbos LA . Reduced transverse spinal area secondary to burst fractures: is there a relationship to neurologic injury? J Neurotrauma 1994; 11: 711–720.
American Spinal Injury Association. International standards for neurological classification of spinal cord injury (revised 2000). American Spinal Injury Association: Chicago, IL, 2002.
Marino RJ, Graves DE . Metric properties of the ASIA motor score: subscales improve correlation with functional activities. Arch Phys Med Rehabil 2004; 85: 1804–1810.
Furlan JC, Noonan V, Singh A, Fehlings MG . Assessment of impairment in patients with acute traumatic spinal cord injury: a systematic review of the literature. J Neurotrauma 2011; 28: 1445–1477.
Spiess MR, Muller RM, Rupp R, Schuld C, van Hedel HJ . Conversion in ASIA impairment scale during the first year after traumatic spinal cord injury. J Neurotrauma 2009; 26: 2027–2036.
Catz A, Itzkovich M, Steinberg F, Philo O, Ring H, Ronen J et al. The Catz-Itzkovich SCIM: a revised version of the Spinal Cord Independence Measure. Disabil Rehabil 2001; 23: 263–268.
Catz A, Itzkovich M, Tesio L, Biering-Sorensen F, Weeks C, Laramee MT et al. A multicenter international study on the Spinal Cord Independence Measure, version III: Rasch psychometric validation. Spinal Cord 2007; 45: 275–291.
Anderson KD, Acuff ME, Arp BG, Backus D, Chun S, Fisher K et al. United States (US) multi-center study to assess the validity and reliability of the Spinal Cord Independence Measure (SCIM III). Spinal Cord 2011; 49: 880–885.
Lam T, Noonan VK, Eng JJ . A systematic review of functional ambulation outcome measures in spinal cord injury. Spinal Cord 2008; 46: 246–254.
Kaiser MG, Mummaneni PV, Matz PG, Anderson PA, Groff MW, Heary RF et al. Radiographic assessment of cervical subaxial fusion. J Neurosurg Spine 2009; 11: 221–227.
Kuklo TR, Polly DW, Owens BD, Zeidman SM, Chang AS, Klemme WR . Measurement of thoracic and lumbar fracture kyphosis: evaluation of intraobserver, interobserver, and technique variability. Spine 2001; 26: 61–65 discussion 6.
Isomi T, Panjabi MM, Kato Y, Wang JL . Radiographic parameters for evaluating the neurological spaces in experimental thoracolumbar burst fractures. J Spinal Disord 2000; 13: 404–411.
Keynan O, Fisher CG, Vaccaro A, Fehlings MG, Oner FC, Dietz J et al. Radiographic measurement parameters in thoracolumbar fractures: a systematic review and consensus statement of the spine trauma study group. Spine 2006; 31: E156–E165.
van Middendorp JJ, Hosman AJ, Donders AR, Pouw MH, Ditunno JF, Curt A et al. A clinical prediction rule for ambulation outcomes after traumatic spinal cord injury: a longitudinal cohort study. Lancet 2011; 377: 1004–1010.
van Middendorp JJ, Hosman AJ, Pouw MH, Van de Meent H . ASIA impairment scale conversion in traumatic SCI: is it related with the ability to walk? A descriptive comparison with functional ambulation outcome measures in 273 patients. Spinal Cord 2009; 47: 555–560.
Chapter 9: Trial size. In: Machin D, Fayers PM eds ). Randomized Clinical Trials: Design, Practice and Reporting. Wiley-Blackwell: Chichester, UK, 2010.
Baker SP, O'Neill B, Haddon W, Long WB . The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma 1974; 14: 187–196.
van Middendorp JJ, Albert TJ, Veth RP, Hosman AJ . Methodological systematic review: mortality in elderly patients with cervical spine injury: a critical appraisal of the reporting of baseline characteristics, follow-up, cause of death, and analysis of risk factors. Spine 2010; 35: 1079–1087.
Rosenbaum PR, Rubin DB . Reducing Bias in Observational Studies Using Subclassification on the Propensity Score. J Am Stat Assoc 1984; 79(387): 516–524.
D'Agostino RB, D'Agostino RB . Estimating treatment effects using observational data. JAMA 2007; 297: 314–316.
D'Agostino RB . Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med 1998; 17: 2265–2281.
Janssen KJ, Donders AR, Harrell FE, Vergouwe Y, Chen Q, Grobbee DE et al. Missing covariate data in medical research: to impute is better than to ignore. J Clin Epidemiol 2010; 63: 721–727.
Rikkert MG, Lauque S, Frolich L, Vellas B, Dekkers W . The practice of obtaining approval from medical research ethics committees: a comparison within 12 European countries for a descriptive study on acetylcholinesterase inhibitors in Alzheimer's dementia. Eur J Neurol 2005; 12: 212–217.
European Commission. European Textbook on Ethics in Research. Publications Office of the European Union: Luxembourg, 2010. http://www.ec.europa.eu/research/science-society/document_library/pdf_06/textbook-on-ethics-report_en.pdf.
Bozzo A, Marcoux J, Radhakrishna M, Pelletier J, Goulet B . The role of magnetic resonance imaging in the management of acute spinal cord injury. J Neurotrauma 2011; 28: 1401–1411.
Stradiotti P, Curti A, Castellazzi G, Zerbi A . Metal-related artifacts in instrumented spine. Techniques for reducing artifacts in CT and MRI: state of the art. Eur Spine J 2009; 18(Suppl 1): 102–108.
Koch KM, Hargreaves BA, Pauly KB, Chen W, Gold GE, King KF . Magnetic resonance imaging near metal implants. J Magn Reson Imaging 2010; 32: 773–787.
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP . Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 2007; 335: 806–808.
Teasdale G, Jennett B . Assessment of coma and impaired consciousness. A practical scale. Lancet 1974; 2: 81–84.
Dripps RD, Lamont A, Eckenhoff JE . The role of anesthesia in surgical mortality. JAMA 1961; 178: 261–266.
Sinnreich M, Taylor BV, Dyck PJ . Diabetic neuropathies. Classification, clinical features, and pathophysiological basis. Neurologist 2005; 11: 63–79.
Garg J, Woo K, Hirsch J, Bruffey JD, Dilley RB . Vascular complications of exposure for anterior lumbar interbody fusion. J Vasc Surg 2010; 51: 946–950 discussion 50.
Lobo SM, Lobo FR, Polachini CA, Patini DS, Yamamoto AE, de Oliveira NE et al. Prospective, randomized trial comparing fluids and dobutamine optimization of oxygen delivery in high-risk surgical patients [ISRCTN42445141]. Crit Care 2006; 10: R72.
Bosacco SJ, Gardner MJ, Guille JT . Evaluation and treatment of dural tears in lumbar spine surgery: a review. Clin Orthop Relat Res 2001; 389: 238–247.
Sin AH, Caldito G, Smith D, Rashidi M, Willis B, Nanda A . Predictive factors for dural tear and cerebrospinal fluid leakage in patients undergoing lumbar surgery. J Neurosurg Spine 2006; 5: 224–227.
Amato V, Giannachi L, Irace C, Corona C . Accuracy of pedicle screw placement in the lumbosacral spine using conventional technique: computed tomography postoperative assessment in 102 consecutive patients. J Neurosurg Spine 2010; 12: 306–313.
Kast E, Mohr K, Richter HP, Borm W . Complications of transpedicular screw fixation in the cervical spine. Eur Spine J 2006; 15: 327–334.
Ito Y, Sugimoto Y, Tomioka M, Hasegawa Y, Nakago K, Yagata Y . Clinical accuracy of 3D fluoroscopy-assisted cervical pedicle screw insertion. J Neurosurg Spine 2008; 9: 450–453.
Okuyama K, Abe E, Suzuki T, Tamura Y, Chiba M, Sato K . Can insertional torque predict screw loosening and related failures? An in vivo study of pedicle screw fixation augmenting posterior lumbar interbody fusion. Spine 2000; 25: 858–864.
Pull ter Gunne AF, Mohamed AS, Skolasky RL, van Laarhoven CJ, Cohen DB . The presentation, incidence, etiology, and treatment of surgical site infections after spinal surgery. Spine 2010; 35: 1323–1328.
Horan TC, Gaynes RP, Martone WJ, Jarvis WR, Emori TG . CDC definitions of nosocomial surgical site infections, 1992: a modification of CDC definitions of surgical wound infections. Am J Infect Control 1992, 271–274.
Kraemer P, Lee MB, Englehardt H, Chapman JR, Bransford RJ . Infectious pin complication rates in halo vest fixators using ceramic versus metallic pins. J Spinal Disord Tech 2010; 23: e59–e62.
Ebraheim NA, Liu J, Patil V, Hiltner L, Shapiro A, Zamary KR et al. An evaluation of halo pin insertion torque on outer table penetration in elderly patients. J Spinal Disord Tech 2009; 22: 177–181.
van Middendorp JJ, Slooff WB, Nellestein WR, Oner FC . Incidence of and risk factors for complications associated with halo-vest immobilization: a prospective, descriptive cohort study of 239 patients. J Bone Joint Surg Am 2009; 91: 71–79.
Winslow CP, Winslow TJ, Wax MK . Dysphonia and dysphagia following the anterior approach to the cervical spine. Arch Otolaryngol Head Neck Surg 2001; 127: 51–55.
Skoretz SA, Flowers HL, Martino R . The incidence of dysphagia following endotracheal intubation: a systematic review. Chest 2010; 137: 665–673.
Beeckman D, Schoonhoven L, Fletcher J, Furtado K, Gunningberg L, Heyman H et al. EPUAP classification system for pressure ulcers: European reliability study. J Adv Nurs 2007; 60: 682–691.
Roghi A, Palmieri B, Crivellaro W, Sara R, Puttini M, Faletra F . Preoperative assessment of cardiac risk in noncardiac major vascular surgery. Am J Cardiol 1999; 83: 169–174.
Frietsch T, Karger R, Scholer M, Huber D, Bruckner T, Kretschmer V et al. Leukodepletion of autologous whole blood has no impact on perioperative infection rate and length of hospital stay. Transfusion 2008; 48: 2133–2142.
Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L et al. Report of the American-European Consensus conference on acute respiratory distress syndrome: definitions, mechanisms, relevant outcomes, and clinical trial coordination. Consensus Committee. J Crit Care 1994; 9: 72–81.
Duggan M, Kavanagh BP . Pulmonary atelectasis: a pathogenic perioperative entity. Anesthesiology 2005; 102: 838–854.
Kollef MH, Shapiro SD, Clinkscale D, Cracchiolo L, Clayton D, Wilner R et al. The effect of respiratory therapist-initiated treatment protocols on patient outcomes and resource utilization. Chest 2000; 117: 467–475.
Erkan D, Harrison MJ, Levy R, Peterson M, Petri M, Sammaritano L et al. Aspirin for primary thrombosis prevention in the antiphospholipid syndrome: a randomized, double-blind, placebo-controlled trial in asymptomatic antiphospholipid antibody-positive individuals. Arthritis Rheum 2007; 56: 2382–2391.
Carrier M, Rodger MA, Wells PS, Righini M, LEG G . Residual vein obstruction to predict the risk of recurrent venous thromboembolism in patients with deep vein thrombosis: a systematic review and meta-analysis. J Thromb Haemost 2011; 9: 1119–1125.
Nys S, van Merode T, Bartelds AI, Stobberingh EE . Urinary tract infections in general practice patients: diagnostic tests versus bacteriological culture. J Antimicrob Chemother 2006; 57: 955–958.
Evans A, Perez I, Harraf F, Melbourn A, Steadman J, Donaldson N et al. Can differences in management processes explain different outcomes between stroke unit and stroke-team care? Lancet 2001; 358: 1586–1592.
Ozturk E, Kiran RP, Remzi F, Fazio VW . Early readmission after ileoanal pouch surgery. Dis Colon Rectum 2009; 52: 1848–1853.
Mor IJ, Vogel JD, da Luz Moreira A, Shen B, Hammel J, Remzi FH . Infliximab in ulcerative colitis is associated with an increased risk of postoperative complications after restorative proctocolectomy. Dis Colon Rectum 2008; 51: 1202–1207; discussion 7-10.
Acknowledgements
We are indebted to Dr H Van de Meent for his invaluable assistance with the preparations of the manuscript. We would also like to thank Dr H Saraste, Dr L Benneker, Dr A Lazary, Dr C Kilincer, Dr M Fehlings and Dr O Moraes-Heton Defino who provided feedback and indirectly contributed to the final study protocol. We are grateful to the support of the European Multicenter Study of Human Spinal Cord Injury (EM-SCI) network for providing data for the sample size calculation. We acknowledge Dr M Rovers for her expertise and time spent on the statistical part of this study protocol.
JJvM drafted the study protocol and manuscript. AH contributed to the design of the study protocol. GB and MS provided feedback during the development of the study protocol. AH, GB and MS co-authored the writing of the manuscript. All the authors read and approved the final manuscript. For the primary report of the clinical results, the authorship will be determined according to the recommendations of the International Committee of Medical Journal Editors where special attention will be paid to collaborators’ intellectual and operational contribution (including the number of patients with complete follow-up in each center).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
van Middendorp, J., Barbagallo, G., Schuetz, M. et al. Design and rationale of a Prospective, Observational European Multicenter study on the efficacy of acute surgical decompression after traumatic Spinal Cord Injury: the SCI-POEM study. Spinal Cord 50, 686–694 (2012). https://doi.org/10.1038/sc.2012.34
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2012.34
Keywords
This article is cited by
-
Pharmacologic and Acute Management of Spinal Cord Injury in Adults and Children
Current Treatment Options in Neurology (2022)
-
Prophylactic enlargement of the thecal sac volume by spinal expansion duroplasty in patients with unresectable malignant intramedullary tumors and metastases prior to radiotherapy
Neurosurgical Review (2020)
-
Effects of antidepressant and treadmill gait training on recovery from spinal cord injury in rats
Spinal Cord (2013)