Abstract
Study design:
Retrospective case review.
Objectives:
In the present study, the neurological outcome, retirement and prognostic factors of patients with spinal cord injury without radiographic abnormality (SCIWORA) were evaluated.
Setting:
Swiss national work accident insurance database.
Methods:
The medical histories of 32 patients who were insured by the Swiss Accident Insurance Fund (SUVA) and had SCIWORA between 1995 and 2004 were evaluated thoroughly. Moreover, all available magnetic resonance imaging (MRI) scans were evaluated.
Results:
At the last follow-up, none of the patients had complete spinal cord injury, only 4 patients had severe deficits and 12 patients had normal motor and sensory function in the neurological examination. However, only 7 out of 32 patients had returned to full-time work and 10 out of 32 patients were fully retired. Both the presence of spinal cord change (ρ=0.51) and higher maximum spinal cord compression (ρ=0.57) in MRI scan correlated with the likelihood for retirement; older age (ρ=0.38) and physical load of work (ρ=0.4) correlated with retirement to a lesser extent.
Conclusion:
Although the neurological outcome of SCIWORA is mostly good, the retirement rate is high. Presence of spinal cord change and severity of cord compression are the best predictors for the degree of retirement.
Similar content being viewed by others
Introduction
A spinal cord injury without radiographic abnormality (SCIWORA) was first described as a self-contained syndrome in children in 1982.1 Thereafter, it has also been reported in adult populations.2, 3, 4, 5, 6, 7, 8
The development of magnetic resonance imaging (MRI) has increased the diagnostic accuracy in the assessment of spinal cord injuries, but it has also lead to a controversy regarding the definition of SCIWORA by visualisation of soft tissue injuries.9, 10 Moreover, using MRI scan, adult patients with SCIWORA have been found to present disc herniations, ossification of the posterior longitudinal ligament, spinal canal stenosis and cervical spondylosis as predisposing factors for spinal cord injury.2, 3, 4, 5, 6, 7, 8
The outcome of patients with SCIWORA has considerable variation according to the severity of the injury. The spinal cord signal changes have been reported to be prognostic for the recovery from injury.5 The outcome is worst in patients with cord disruption, poor in patients with haemorrhage and good in patients with oedema or normal cord.7, 8, 10 Koyanagi et al.2 reported smaller sagittal diameters of the central spinal canal in computerised tomography scans of patients with SCIWORA when compared with patients who had a trauma without a spinal cord injury. Moreover, the severe spinal cord compression in MRI scans has been shown to be associated with severe paralysis and poor recovery.5 The outcome of SCIWORA has been described in several studies, but to our knowledge the working capacity after SCIWORA in patients at working age has not been previously reported.
Fehlings et al.11 proposed a MRI-scan-based method for the quantitative assessment of maximum canal compromise (MCC) and maximum spinal cord compression (MSCC) in patients with cervical spinal cord injury. In their study, the MCC and MSCC were both associated to some degree with the severity of neurological deficit in patients with acute cervical spinal cord injury. Thereafter, the reliability of the method by using mid-sagittal MRI images was validated.12
In the present study, we evaluated the neurological outcome, working capacity and prognostic factors of 32 adult patients with spinal cord injury without radiographic evidence of spinal fracture or dislocation.
Patients and methods
In Switzerland, people who work more than 8 h per week need an obligatory accident insurance that covers all work-related accidents and diseases as well as other accidents. About 50% of the working population is insured by SUVA (Swiss Accident Insurance Fund) and the rest have insurance in other, smaller companies. SUVA has access rights to all hospital and health care files of its clients.
The medical history, available radiographs, computerised tomography and MRI scans of all patients who were insured by SUVA and had SCIWORA between 1995 and 2004 were reviewed by a SUVA expert panel. The SCIWORA was defined as a spinal cord injury without fracture or dislocation in plain radiographs. One patient was excluded from the study because his follow-up time was only 2 months. The final number of SCIWORA patients was 32. Altogether, 29 patients had MRI scans taken but the initial MRI scans of only 16 patients were found.
Using medical histories, the Frankel classification of neurological injury was determined by the SUVA expert panel.13 The presence of spinal canal stenosis, disc protrusion or herniation and changes in spinal cord were recorded based on the initial radiologists' assessments. In addition, MCC and MSCC were measured from available MRI scans in 16 patients. The physical load of work of each case was classified as light, moderate or heavy, based on the job titles that were recorded in the SUVA files.
Measurements
The mid-sagittal T1- and T2-weighted MRI images were used to assess the MCC and MSCC, respectively. The anteroposterior diameter of the spinal canal and anteroposterior cord diameter at the level of the MCC or at the level of intramedullary cord signal changes were compared with respective diameters at normal levels above and below the injury. Normal diameters were measured at the adjacent midvertebral body levels. The MCC and MSCC were calculated using the following formula:11

Di, anteroposterior canal or cord diameter at the level of injury; Da, anteroposterior canal or cord diameter at nearest normal level above the level of injury; Db, anteroposterior canal or cord diameter at the nearest normal level below the level of injury.
The demographic factors, MRI findings and measurements and physical load of work were correlated to the neurological outcome and work status of the patients.
Statistics
Non-parametric methods, namely Spearman's rank correlation coefficient, were used for the assessment of group correlations. The level of significance was set to 0.05. The statistical analyses were conducted using SAS 9.2 (SAS Institute Inc., Cary, NC, USA).
Results
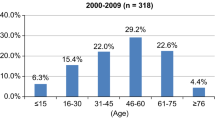
The mean age (range) of the 32 SCIWORA patients was 46.9 (18–64) years, and 29 of the patients were men. The injuries of 11, 10 and 7 patients were caused by traffic-, sports- and work-related accidents, respectively. The injuries of the other four patients were caused by accidents at leisure time. In all, 40.6% of cases had a physically less demanding work, 25% a moderate one and 34.3% were involved in physically heavy work. The level of injury was at the cervical spine in 27 and at the thoracic spine in 5 patients. A surgical intervention was performed in 14 patients (9 anterior decompressions and fusions, 3 laminectomies and 2 combined anterior and posterior interventions). According to the initial radiographic assessment, 24 patients presented a spinal canal stenosis and 16 of them also had a disc protrusion or herniation. Furthermore, 17 patients had spinal cord changes.
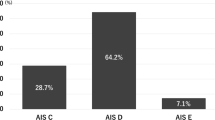
The mean (range) follow-up time was 3 years 7 months (1–11 years). The initial clinical presentation of spinal cord injury according to the Frankel classification was A, B, C and D in 7, 5, 5 and 15 patients, respectively. All patients with complete tetraplegia at the beginning, improved within a few hours time. Moreover, during the follow-up, the Frankel grade did not deteriorate in any of the patients, remained the same in nine patients and improved in all others. Therefore, at the end of the follow-up, none of the patients had complete tetra- or paraplegia (Frankel grade A), only 4 patients had severe deficits (Frankel grade C) and 12 patients had normal motor and sensory function in neurological examination (Frankel grade E). The Frankel grade at the beginning and at the end of the follow-up is described in Table 1.
Before injury, all patients were employed. However, at the end of the follow-up, only 7 out of 32 patients had returned to full-time work and 10 patients were fully retired (Table 2). The rest of the patients were partially retired (from 25 to 80%). Two patients were still under consideration for retirement.
Older age was moderately correlated with the degree of retirement (Spearman's ρ=0.38, P-value=0.04), and the presence of spinal cord change (based on the initial radiologists' assessments) was moderately correlated with worse final Frankel grade (ρ=0.39, P-value=0.02) but better correlated with the degree of retirement (ρ=0.51, P-value=0.002; Table 3). In 16 patients with available MRI scans, more severe MSCC correlated well with worse Frankel grade (ρ=0.57, P-value=0.02) and similarly well with the degree of retirement (ρ=0.57. P-value=0.04). The physical load of work was moderately correlated with the degree of retirement (ρ=0.4, P=0.008).
Discussion
SCIWORA was originally described before common use of MRI scan in diagnosing spinal cord injuries.1 The development of MRI has increased the diagnostic accuracy of neuroimaging by visualising the soft tissue injuries and also pathologies causing the spinal cord compression, which has lead to a controversy in the definition of SCIWORA.9, 10 The term of spinal cord injury without radiographic evidence of trauma (SCIWORET), which occurs in combination with cervical spondylosis, spinal stenosis, disc herniation and so on, and real SCIWORA, which excludes all neuroimaging abnormalities, have also been established.3, 9 As there is no common consensus for a new terminology, we still use the term SCIWORA in description of the syndrome of spinal cord injury without fracture or dislocation in plain radiographs, although patients presented spinal stenosis, disc herniations and so on, in MRI scans.
The severity of neurological injuries caused by SCIWORA varies from complete cord transsection with permanent tetra- or paraplegia to mild transient neurological deficit.10 In our study, seven patients had initially complete tetra- or paraplegia (Frankel grade A). However, four of them fully recovered in a few hours of time, which indicates that they rather presented spinal cord neuropraxia or concussion than real spinal cord injury.14, 15 Moreover, the other three patients with complete tetra- or paraplegia recovered partially. At the end of the follow-up, none of the patients presented Frankel grade A or B neurological deficit and only 4 out of 32 (13%) patients had severe (grade C) deficit. Furthermore, 12 patients had normal motor and sensory function at the final neurological examination. In the study of Tewari et al.8, the outcome was apparently worse (Frankel grade A–C in 18 out of 40 (45%) patients), but in their study the follow-up was only until discharge and the initial neurological injury was worse (severe Frankel grade A–C in 36 out of 40 patients). The more severe injury grades were probably explained by the different trauma mechanisms, which were high-energy road traffic accidents or falls from heights, in 90% of the patients. The outcome of the study of Saruhashi et al.,3 in which the Frankel grade at an average of 31 months follow-up was A–C only in 3 out of 33 (9%) patients, is in accordance with our results.
Although the neurological outcome in our study was generally good, the retirement rate was high. At the end of the follow-up, only 7 out of 32 (22%) of the patients were back at full-time work, 10 out of 32 (31%) patients were fully retired and 2 patients were still under consideration for retirement. The other 13 patients were partially retired. The fact that SUVA is a common insurance in industrial companies, indicating physically heavier stresses at work, may have some influence on the retirement rate. However, only about a quarter of cases were involved in physically more demanding types of work (for example, construction, lumbering), and the correlation between the degree of retirement and physical load of work was only moderate. Of the seven patients who were fully reintegrated at work, the neurological outcome was Frankel grade E in four and D in three cases. In contrast, the final Frankel grade was E in only one of the fully retired patients. The degree of retirement was, hence, better correlated with spinal cord change and spinal cord compression, and to a lesser extent with older age and physical load of work.
Developmental and degenerative narrowing of the cervical canal has been shown to be a causative factor for cervical cord neurapraxia.14 Moreover, the spinal canal narrowing caused by degenerative changes like spondylosis has been found to be a pre-existing factor in patients with acute cervical cord injury without bone injuries.2, 6 In these patients, the spinal cord compression caused by degenerative changes has also been used for the indication of surgery.3 Fehlings et al. described11 and validated12 a quantitative method for assessing spinal canal compromise and spinal cord compression in patients with cervical spinal cord injury. They also found some association between the canal or spinal cord compressions and the neurological deficit. In the present study, the severity of spinal cord compression correlated well with the outcome regarding neurological deficit and the degree of retirement.
Conclusions
In patients with spinal cord injury without evidence of fracture or dislocation of spinal structures, the neurological outcome was mostly good. However, only 22% of patients returned back to full-time work. Presence of spinal cord change and severity of spinal cord compression were the best predictors for a higher degree of retirement, older age and physical load of work were moderately correlated with it.
References
Pang D, Wilberger Jr JE . Spinal cord injury without radiographic abnormalities in children. J Neurosurg 1982; 57: 114–129.
Koyanagi I, Iwasaki Y, Hida K, Akino M, Imamura H, Abe H . Acute cervical cord injury without fracture or dislocation of the spinal column. J Neurosurg 2000; 93: 15–20.
Saruhashi Y, Hukuda S, Katsuura A, Asajima S, Omura K . Clinical outcomes of cervical spinal cord injuries without radiographic evidence of trauma. Spinal Cord 1998; 36: 567–573.
Hendey GW, Wolfson AB, Mower WR, Hoffman JR . Spinal cord injury without radiographic abnormality: results of the National Emergency X-Radiography Utilization Study in blunt cervical trauma. J Trauma 2002; 53: 1–4.
Hayashi K, Yone K, Ito H, Yanase M, Sakou T . MRI findings in patients with a cervical spinal cord injury who do not show radiographic evidence of a fracture or dislocation. Paraplegia 1995; 33: 212–215.
Regenbogen VS, Rogers LF, Atlas SW, Kim KS . Cervical spinal cord injuries in patients with cervical spondylosis. Am J Roentgenol 1986; 146: 277–284.
Gupta SK, Rajeev K, Khosla VK, Sharma BS, Paramjit, Mathuriya SN et al. Spinal cord injury without radiographic abnormality in adults. Spinal Cord 1999; 37: 726–729.
Tewari MK, Gifti DS, Singh P, Khosla VK, Mathuriya SN, Gupta SK et al. Diagnosis and prognostication of adult spinal cord injury without radiographic abnormality using magnetic resonance imaging: analysis of 40 patients. Surg Neurol 2005; 63: 204–209.
Yucesoy K, Yuksel KZ . SCIWORA in MRI era. Clin Neurol Neurosurg 2008; 110: 429–433.
Pang D . Spinal cord injury without radiographic abnormality in children, 2 decades later. Neurosurgery 2004; 55: 1325–1343.
Fehlings MG, Rao SC, Tator CH, Skaf G, Arnold P, Benzel E et al. The optimal radiologic method for assessing spinal canal compromise and cord compression in patients with cervical spinal cord injury. Part II: Results of a multicenter study. Spine 1999; 24: 605–613.
Fehlings MG, Furlan JC, Massicotte EM, Arnold P, Aarabi B, Harrop J et al. Interobserver and intraobserver reliability of maximum canal compromise and spinal cord compression for evaluation of acute traumatic cervical spinal cord injury. Spine 2006; 31: 1719–1725.
Frankel HL, Hancock DO, Hyslop G, Melzak J, Michaelis LS, Ungar GH et al. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. Paraplegia 1969; 7: 179–192.
Torg JS, Corcoran TA, Thibault LE, Pavlov H, Sennett BJ, Naranja Jr RJ et al. Cervical cord neurapraxia: classification, pathomechanics, morbidity, and management guidelines. J Neurosurg 1997; 87: 843–850.
Haller H, Leblhuber F, Trenkler J, Kröpfl A . Trauma-induced spinal palsy without fracture or instability of the vertebral skeleton. Eur J Trauma 2002; 1: 106–110.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Neva, M., Roeder, C., Felder, U. et al. Neurological outcome, working capacity and prognostic factors of patients with SCIWORA. Spinal Cord 50, 78–80 (2012). https://doi.org/10.1038/sc.2011.100
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2011.100
Keywords
This article is cited by
-
Surfer’s myelopathy: an atypical case presentation
Spinal Cord Series and Cases (2020)
-
A geriatric patient with spinal cord injury without radiographic abnormality: outcomes and causes
Spinal Cord Series and Cases (2018)
-
Spinal cord injury without radiographic abnormality (SCIWORA) in adults: MRI type predicts early neurologic outcome
Spinal Cord (2016)