Key Points
-
Major complications occur in one-third of patients during the month after transcatheter aortic valve replacement (TAVR)
-
Adequate patient screening and selection, using a 'heart team' approach and multimodality imaging, is important for the prevention of TAVR-related complications
-
Complications should be anticipated during a multidisciplinary evaluation before TAVR, to enable prompt recognition and management should such events occur during the procedure
-
The TAVR team should always be ready to perform immediate percutaneous or surgical rescue interventions in the event of serious TAVR-related complications
-
Growing operator experience and upcoming technological refinements will reduce the incidence of TAVR-related complications in the future
Abstract
Patients with severe aortic stenosis who are at high surgical risk or not considered to be suitable candidates for surgical aortic valve replacement are increasingly being treated with transcatheter aortic valve replacement (TAVR). Although this novel treatment modality has been proven to be effective in this patient population, serious complications oc cur in approximately one-third of patients during the month after the procedure. Such events include myocardial infarction, cerebrovascular events, vascular complications, bleeding, acute kidney injury, valve regurgitation, valve malpositioning, coronary obstruction, and conduction disturbances and arrhythmias, which can all lead to death. Prevention of these complications should be based on patient screening and selection by a dedicated 'heart team' and the use of multimodality imaging. Anticipation and early recognition of these complications, followed by prompt management using a wide range of percutaneous or surgical rescue interventions, is vital to patient outcome. Continuous patient assessment and reporting of complications according to standardized definitions, in addition to growing operator experience and upcoming technological refinements, will hopefully reduce the future rate of complications related to this procedure.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
Change history
06 November 2013
In the version of this article originally published online, the sentence “The Claret CE Pro™ system (Claret Medical, Inc., Santa Rosa, CA, USA; Figure 2a) consists of...” should have read “The Claret Montage™ Dual Filter System (Claret Medical, Inc., Santa Rosa, CA, USA; Figure 2a) consists of...”. The error has been corrected in the HTML and PDF versions of the article.
References
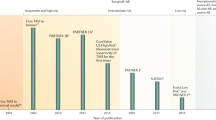
Cribier, A. et al. Percutaneous transcatheter implantation of an aortic valve prosthesis for calcific aortic stenosis: first human case description. Circulation 106, 3006–3008 (2002).
Leon, M. B. et al. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N. Engl. J. Med. 363, 1597–1607 (2010).
Smith, C. R. et al. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N. Engl. J. Med. 364, 2187–2198 (2011).
Vahanian, A. et al. Guidelines on the management of valvular heart disease (version 2012). Eur. Heart J. 33, 2451–2496 (2012).
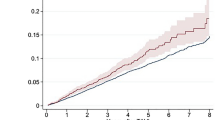
Généreux, P. et al. Clinical outcomes after transcatheter aortic valve replacement using valve academic research consortium definitions: a weighted meta-analysis of 3,519 patients from 16 studies. J. Am. Coll. Cardiol. 59, 2317–2326 (2012).
Leon, M. B. et al. Standardized endpoint definitions for transcatheter aortic valve implantation clinical trials: a consensus report from the Valve Academic Research Consortium. Eur. Heart J. 32, 205–217 (2011).
Kappetein, A. P. et al. Updated standardized endpoint definitions for transcatheter aortic valve implantation: the Valve Academic Research Consortium-2 consensus document. Eur. Heart J. 33, 2403–2418 (2012).
van der Boon, R. M. et al. New conduction abnormalities after TAVI—frequency and causes. Nat. Rev. Cardiol. 9, 454–463 (2012).
Himbert, D. et al. Tools & techniques: transcatheter aortic valve implantation: transfemoral approach. EuroIntervention 6, 784–785 (2011).
Eggebrecht, H. et al. Emergent cardiac surgery during transcatheter aortic valve implantation (TAVI): a weighted meta-analysis of 9,251 patients from 46 studies. EuroIntervention 8, 1072–1080 (2013).
Khatri, P. J. et al. Adverse effects associated with transcatheter aortic valve implantation: a meta-analysis of contemporary studies. Ann. Intern. Med. 158, 35–46 (2013).
Gilard, M. et al. Registry of transcatheter aortic-valve implantation in high-risk patients. N. Engl. J. Med. 366, 1705–1715 (2012).
Van Mieghem, N. M. et al. Cause of death after transcatheter aortic valve implantation. Catheter. Cardiovasc. Interv. http://dx.doi.org/10.1002/ccd.24597.
Rodés-Cabau, J. et al. Incidence, predictive factors, and prognostic value of myocardial injury following uncomplicated transcatheter aortic valve implantation. J. Am. Coll. Cardiol. 57, 1988–1999 (2011).
Yong, Z. Y. et al. Predictors and prognostic value of myocardial injury during transcatheter aortic valve implantation. Circ. Cardiovasc. Interv. 5, 415–423 (2012).
Barbash, I. M. et al. Prevalence and effect of myocardial injury after transcatheter aortic valve replacement. Am. J. Cardiol. 111, 1337–1343 (2013).
Dewey, T. M. et al. Effect of concomitant coronary artery disease on procedural and late outcomes of transcatheter aortic valve implantation. Ann. Thorac. Surg. 89, 758–767 (2010).
Gasparetto, V. et al. Safety and effectiveness of a selective strategy for coronary artery revascularization before transcatheter aortic valve implantation. Catheter. Cardiovasc. Interv. 81, 376–383 (2013).
Gautier, M. et al. Impact of coronary artery disease on indications for transcatheter aortic valve implantation and on procedural outcomes. EuroIntervention 7, 549–555 (2011).
Wenaweser, P. et al. Impact of coronary artery disease and percutaneous coronary intervention on outcomes in patients with severe aortic stenosis undergoing transcatheter aortic valve implantation. EuroIntervention 7, 541–548 (2011).
van Swieten, J. C., Koudstaal, P. J., Visser, M. C., Schouten, H. J. & van Gijn, J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke 19, 604–607 (1988).
Miller, D. C. et al. Transcatheter (TAVR) versus surgical (AVR) aortic valve replacement: occurrence, hazard, risk factors, and consequences of neurologic events in the PARTNER trial. J. Thorac. Cardiovasc. Surg. 143, 832–843.e13 (2012).
Nombela-Franco, L. et al. Timing, predictive factors, and prognostic value of cerebrovascular events in a large cohort of patients undergoing transcatheter aortic valve implantation. Circulation 126, 3041–3053 (2012).
Stortecky, S. et al. Cerebrovascular accidents complicating transcatheter aortic valve implantation: frequency, timing and impact on outcomes. EuroIntervention 8, 62–70 (2012).
Eggebrecht, H. et al. Risk of stroke after transcatheter aortic valve implantation (TAVI): a meta-analysis of 10,037 published patients. EuroIntervention 8, 129–138 (2012).
Amat-Santos, I. J. et al. Incidence, predictive factors, and prognostic value of new-onset atrial fibrillation following transcatheter aortic valve implantation. J. Am. Coll. Cardiol. 59, 178–188 (2012).
Omran, H. et al. Silent and apparent cerebral embolism after retrograde catheterisation of the aortic valve in valvular stenosis: a prospective, randomised study. Lancet 361, 1241–1246 (2003).
Ghanem, A. et al. Prognostic value of cerebral injury following transfemoral aortic valve implantation. EuroIntervention 8, 1296–1306 (2013).
Fairbairn, T. A. et al. Diffusion-weighted MRI determined cerebral embolic infarction following transcatheter aortic valve implantation: assessment of predictive risk factors and the relationship to subsequent health status. Heart 98, 18–23 (2012).
Kahlert, P. et al. Silent and apparent cerebral ischemia after percutaneous transfemoral aortic valve implantation: a diffusion-weighted magnetic resonance imaging study. Circulation 121, 870–878 (2010).
Astarci, P. et al. Cerebral embolization during percutaneous valve implantation does not occur during balloon inflation valvuloplasty: prospective diffusion-weighted brain MRI study. J. Heart Valve Dis. 22, 79–84 (2013).
Ghanem, A. et al. Risk and fate of cerebral embolism after transfemoral aortic valve implantation: a prospective pilot study with diffusion-weighted magnetic resonance imaging. J. Am. Coll. Cardiol. 55, 1427–1432 (2010).
Rodés-Cabau, J. et al. Cerebral embolism following transcatheter aortic valve implantation: comparison of transfemoral and transapical approaches. J. Am. Coll. Cardiol. 57, 18–28 (2011).
Kahlert, P. et al. Cerebral embolization during transcatheter aortic valve implantation: a transcranial Doppler study. Circulation 126, 1245–1255 (2012).
Van Mieghem, N. M. et al. Histopathology of embolic debris captured during transcatheter aortic valve replacement. Circulation 127, 2194–2201 (2013).
Grube, E. et al. Feasibility of transcatheter aortic valve implantation without balloon pre-dilation: a pilot study. JACC Cardiovasc. Interv. 4, 751–757 (2011).
Bagur, R. et al. Transcatheter aortic valve implantation with “no touch” of the aortic arch for the treatment of severe aortic stenosis associated with complex aortic atherosclerosis. J. Card. Surg. 25, 501–503 (2010).
Nietlispach, F. et al. An embolic deflection device for aortic valve interventions. JACC Cardiovasc. Interv. 3, 1133–1138 (2010).
Bourantas, C. V. et al. Transcatheter aortic valve implantation: new developments and upcoming clinical trials. EuroIntervention 8, 617–627 (2012).
Naber, C. K. et al. First-in-man use of a novel embolic protection device for patients undergoing transcatheter aortic valve implantation. EuroIntervention 8, 43–50 (2012).
Webb, J. G. & Barbanti, M. Cerebral embolization during transcatheter aortic valve implantation. Circulation 126, 1567–1569 (2012).
Van Mieghem, N. M. et al. Transcatheter aortic valve replacement and vascular complications definitions. EuroIntervention [online].
Mussardo, M. et al. Periprocedural and short-term outcomes of transfemoral transcatheter aortic valve implantation with the Sapien XT as compared with the Edwards Sapien valve. JACC Cardiovasc. Interv. 4, 743–750 (2011).
Généreux, P. et al. Vascular complications after transcatheter aortic valve replacement: insights from the PARTNER (Placement of AoRTic TraNscathetER Valve) trial. J. Am. Coll. Cardiol. 60, 1043–1052 (2012).
Hayashida, K. et al. Transfemoral aortic valve implantation new criteria to predict vascular complications. JACC Cardiovasc. Interv. 4, 851–858 (2011).
Van Mieghem, N. M. et al. Trends in outcome after transfemoral transcatheter aortic valve implantation. Am. Heart J. 165, 183–192 (2013).
Ducrocq, G. et al. Vascular complications of transfemoral aortic valve implantation with the Edwards SAPIEN prosthesis: incidence and impact on outcome. EuroIntervention 6, 666–672 (2010).
Hayashida, K. et al. True percutaneous approach for transfemoral aortic valve implantation using the Prostar XL device: impact of learning curve on vascular complications. JACC Cardiovasc. Interv. 5, 207–214 (2012).
Pasic, M. et al. Rupture of the device landing zone during transcatheter aortic valve implantation: a life-threatening but treatable complication. Circ. Cardiovasc. Interv. 5, 424–432 (2012).
Barbanti, M. et al. Anatomical and procedural features associated with aortic root rupture during balloon-expandable transcatheter aortic valve replacement. Circulation 128, 244–253 (2013).
Martinez, M. I., Garcia, H. G. & Calvar, J. A. Interventricular septum rupture after transcatheter aortic valve implantation. Eur. Heart J. 33, 190 (2012).
Blanke, P. et al. Prosthesis oversizing in balloon-expandable transcatheter aortic valve implantation is associated with contained rupture of the aortic root. Circ. Cardiovasc. Interv. 5, 540–548 (2012).
Borz, B. et al. Incidence, predictors and impact of bleeding after transcatheter aortic valve implantation using the balloon-expandable Edwards prosthesis. Heart 99, 860–865 (2013).
Pilgrim, T., Stortecky, S., Luterbacher, F., Windecker, S. & Wenaweser, P. Transcatheter aortic valve implantation and bleeding: incidence, predictors and prognosis. J. Thromb. Thrombolysis 35, 456–462 (2013).
Amabile, N. et al. Incidence, predictors and prognostic value of serious hemorrhagic complications following transcatheter aortic valve implantation. Int. J. Cardiol. 168, 151–156 (2013). .
Tchetche, D. et al. Adverse impact of bleeding and transfusion on the outcome post-transcatheter aortic valve implantation: insights from the Pooled-RotterdAm-Milano-Toulouse In Collaboration Plus (PRAGMATIC Plus) initiative. Am. Heart J. 164, 402–409 (2012).
Rezq, A. et al. Incidence, management, and outcomes of cardiac tamponade during transcatheter aortic valve implantation: a single-center study. JACC Cardiovasc. Interv. 5, 1264–1272 (2012).
Takagi, H., Niwa, M., Mizuno, Y., Goto, S. N. & Umemoto, T. Incidence, predictors, and prognosis of acute kidney injury after transcatheter aortic valve implantation: a summary of contemporary studies using Valve Academic Research Consortium definitions. Int. J. Cardiol. http://dx.doi.org/10.1016/j.ijcard.2013.01.273.
Khawaja, M. Z. et al. The effects of VARC-defined acute kidney injury after transcatheter aortic valve implantation (TAVI) using the Edwards bioprosthesis. EuroIntervention 8, 563–570 (2012).
Nuis, R. J. et al. Blood transfusion and the risk of acute kidney injury after transcatheter aortic valve implantation. Circ. Cardiovasc. Interv. 5, 680–688 (2012).
Bagur, R. et al. Acute kidney injury following transcatheter aortic valve implantation: predictive factors, prognostic value, and comparison with surgical aortic valve replacement. Eur. Heart J. 31, 865–874 (2010).
Jabbour, A. et al. Multimodality imaging in transcatheter aortic valve implantation and post-procedural aortic regurgitation: comparison among cardiovascular magnetic resonance, cardiac computed tomography, and echocardiography. J. Am. Coll. Cardiol. 58, 2165–2173 (2011).
Zamorano, J. L. et al. EAE/ASE recommendations for the use of echocardiography in new transcatheter interventions for valvular heart disease. Eur. J. Echocardiogr. 12, 557–584 (2011).
Zoghbi, W. A. et al. Recommendations for evaluation of prosthetic valves with echocardiography and Doppler ultrasound: a report From the American Society of Echocardiography's Guidelines and Standards Committee and the Task Force on Prosthetic Valves, developed in conjunction with the American College of Cardiology Cardiovascular Imaging Committee, Cardiac Imaging Committee of the American Heart Association, the European Association of Echocardiography, a registered branch of the European Society of Cardiology, the Japanese Society of Echocardiography and the Canadian Society of Echocardiography, endorsed by the American College of Cardiology Foundation, American Heart Association, European Association of Echocardiography, a registered branch of the European Society of Cardiology, the Japanese Society of Echocardiography, and Canadian Society of Echocardiography. J. Am. Soc. Echocardiogr. 22, 975–1014 (2009).
Lerakis, S., Hayek, S. S. & Douglas, P. S. Paravalvular aortic leak after transcatheter aortic valve replacement: current knowledge. Circulation 127, 397–407 (2013).
Michel, P. L., Vahanian, A., Besnainou, F. & Acar, J. Value of qualitative angiographic grading in aortic regurgitation. Eur. Heart J. 8 (Suppl. C), 11–14 (1987).
Sinning, J. M. et al. Aortic regurgitation index defines severity of peri-prosthetic regurgitation and predicts outcome in patients after transcatheter aortic valve implantation. J. Am. Coll. Cardiol. 59, 1134–1141 (2012).
Athappan, G. et al. Incidence, predictors, and outcomes of aortic regurgitation after transcatheter aortic valve replacement: meta-analysis and systematic review of literature. J. Am. Coll. Cardiol. 61, 1585–1595 (2013).
Généreux, P. et al. Paravalvular leak after transcatheter aortic valve replacement: the new Achilles' heel? A comprehensive review of the literature. J. Am. Coll. Cardiol. 61, 1125–1136 (2013).
Sinning, J. M. et al. Evaluation and management of paravalvular aortic regurgitation after transcatheter aortic valve replacement. J. Am. Coll. Cardiol. 62, 11–20 (2013).
Al-Attar, N., Himbert, D., Vahanian, A. & Nataf, P. Severe intraprosthetic regurgitation by immobile leaflet after trans-catheter aortic valve implantation. Eur. J. Cardiothorac. Surg. 39, 591–592 (2011).
Agostoni, P., Buijsrogge, M. P. & Stella, P. R. “Frozen” leaflet: a dreadful complication of transcatheter aortic valve implantation. Circ. Cardiovasc. Interv. 5, 321–323 (2012).
Willson, A. B. et al. Computed tomography-based sizing recommendations for transcatheter aortic valve replacement with balloon-expandable valves: comparison with transesophageal echocardiography and rationale for implementation in a prospective trial. J. Cardiovasc. Comput. Tomogr. 6, 406–414 (2012).
Binder, R. K. et al. The impact of integration of a multidetector computed tomography annulus area sizing algorithm on outcomes of transcatheter aortic valve replacement: a prospective, multicenter, controlled trial. J. Am. Coll. Cardiol. 62, 431–438 (2013).
Schultz, C. J. et al. Three dimensional evaluation of the aortic annulus using multislice computer tomography: are manufacturer's guidelines for sizing for percutaneous aortic valve replacement helpful? Eur. Heart J. 31, 849–856 (2010).
Hayashida, K. et al. Impact of CT-guided valve sizing on post-procedural aortic regurgitation in transcatheter aortic valve implantation. EuroIntervention 8, 546–555 (2012).
Dvir, D. et al. Multicenter evaluation of Edwards SAPIEN positioning during transcatheter aortic valve implantation with correlates for device movement during final deployment. JACC Cardiovasc. Interv. 5, 563–570 (2012).
Binder, R. K. et al. Transcatheter aortic valve replacement with the SAPIEN 3: a new balloon-expandable transcatheter heart valve. JACC Cardiovasc. Interv. 6, 293–300 (2013).
Ussia, G. P. et al. Transcatheter aortic bioprosthesis dislocation: technical aspects and midterm follow-up. EuroIntervention 7, 1285–1292 (2012).
Sinning, J. M., Vasa-Nicotera, M., Werner, N., Nickenig, G. & Hammerstingl, C. Interventional closure of paravalvular leakage after transcatheter aortic valve implantation. Eur. Heart J. 33, 2498 (2012).
Clavel, M. A. et al. Severe valvular regurgitation and late prosthesis embolization after percutaneous aortic valve implantation. Ann. Thorac. Surg. 87, 618–621 (2009).
Pang, P. Y., Chiam, P. T., Chua, Y. L. & Sin, Y. K. A survivor of late prosthesis migration and rotation following percutaneous transcatheter aortic valve implantation. Eur. J. Cardiothorac. Surg. 41, 1195–1196 (2012).
Makkar, R. R. et al. Determinants and outcomes of acute transcatheter valve-in-valve therapy or embolization: a study of multiple valve implants in the US PARTNER trial (Placement of AoRTic TraNscathetER Valve Trial Edwards SAPIEN Transcatheter Heart Valve). J. Am. Coll. Cardiol. 62, 418–430 (2013).
Tay, E. L. et al. Outcome of patients after transcatheter aortic valve embolization. JACC Cardiovasc. Interv. 4, 228–234 (2011).
Dumonteil, N. et al. Left ventricular embolization of an aortic balloon-expandable bioprosthesis: balloon capture and reimpaction as an alternative to emergent conversion to open-heart surgery. JACC Cardiovasc. Interv. 6, 308–310 (2013).
Dvir, D. et al. Transcatheter aortic valve replacement for degenerative bioprosthetic surgical valves: results from the global valve-in-valve registry. Circulation 126, 2335–2344 (2012).
Ribeiro, H. B. et al. Coronary obstruction following transcatheter aortic valve implantation: a systematic review. JACC Cardiovasc. Interv. 6, 452–461 (2013).
Holmes, D. R. Jr et al. 2012 ACCF/AATS/SCAI/STS expert consensus document on transcatheter aortic valve replacement. J. Am. Coll. Cardiol. 59, 1200–1254 (2012).
Himbert, D. et al. Results of transfemoral or transapical aortic valve implantation following a uniform assessment in high-risk patients with aortic stenosis. J. Am. Coll. Cardiol. 54, 303–311 (2009).
Stabile, E. et al. Acute left main obstructions following TAVI. EuroIntervention 6, 100–105 (2010).
Bourantas, C. V. et al. Transcatheter aortic valve implantation: new developments and upcoming clinical trials. EuroIntervention 8, 617–627 (2012).
Author information
Authors and Affiliations
Contributions
A.-A. Fassa, researched data for the article. All the authors contributed to the discussion of content, wrote the article, and reviewed/edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
A. Vahanian has received consulting fees/honoraria from Abbott, Edwards Lifesciences, Medtronic, and Valtech. D. Himbert is Proctor for Edwards Lifesciences and Medtronic. A.-A. Fassa declares no competing interests.
Rights and permissions
About this article
Cite this article
Fassa, AA., Himbert, D. & Vahanian, A. Mechanisms and management of TAVR-related complications. Nat Rev Cardiol 10, 685–695 (2013). https://doi.org/10.1038/nrcardio.2013.156
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrcardio.2013.156
This article is cited by
-
CT and MR imaging prior to transcatheter aortic valve implantation: standardisation of scanning protocols, measurements and reporting—a consensus document by the European Society of Cardiovascular Radiology (ESCR)
European Radiology (2020)
-
An in vitro proof-of-principle study of sonobactericide
Scientific Reports (2018)
-
Morphology, Clinicopathologic Correlations, and Mechanisms in Heart Valve Health and Disease
Cardiovascular Engineering and Technology (2018)
-
Transcatheter Aortic Valve Implantation
Current Atherosclerosis Reports (2016)