Abstract
Cholecystokinin modulates pain and anxiety via its functions within brain regions such as the midbrain periaqueductal gray (PAG). The aim of this study was to examine the cellular actions of cholecystokinin on PAG neurons. Whole-cell patch clamp recordings were made from rat midbrain PAG slices in vitro to examine the postsynaptic effects of cholecystokinin and its effects on synaptic transmission. Sulfated cholecystokinin-(26–33) (CCK-S, 100–300 nM), but not non-sulfated cholecystokinin-(26–33) (CCK-NS, 100–300 nM) produced an inward current in a sub-population of opioid sensitive and insensitive PAG neurons, which did not reverse over a range of membrane potentials. The CCK-S-induced current was abolished by the CCK1 selective antagonist devazepide (100 nM), but not by the CCK2 selective antagonists CI988 (100 nM, 1 μM) and LY225910 (1 μM). CCK-S, but not CCK-NS produced a reduction in the amplitude of evoked GABAA-mediated inhibitory postsynaptic currents (IPSCs) and an increase in the evoked IPSC paired-pulse ratio. By contrast, CCK-S had little effect on the rate and amplitude of TTX-resistant miniature IPSCs under basal conditions and when external K+ was elevated. The CCK-S-induced inhibition of evoked IPSCs was abolished by the cannabinoid CB1 receptor antagonist AM251 (3 μM), the mGluR5 antagonist MPEP (10 μM) and the 1, 2-diacylglycerol lipase (DAGLα) inhibitor tetrahydrolipstatin (10 μM). In addition, CCK-S produced an increase in the rate of spontaneous non-NMDA-mediated, TTX-dependent excitatory postsynaptic currents (EPSCs). These results suggest that cholecystokinin produces direct neuronal depolarisation via CCK1 receptors and inhibits GABAergic synaptic transmission via action potential-dependent release of glutamate and mGluR5-induced endocannabinoid signaling. Thus, cholecystokinin has cellular actions within the PAG that can both oppose and reinforce opioid and cannabinoid modulation of pain and anxiety within this brain structure.
Similar content being viewed by others
INTRODUCTION
Cholecystokinin is one of the most abundant neuropeptides within the central nervous system and has been implicated in the control of satiety, anxiety, depression, cognition, and pain (Faris et al, 1983; Lovick, 2008; Noble et al, 1999). Cholecystokinin produces its effects via two Gq-coupled receptors, CCK1 and CCK2 (Noble et al, 1999). The midbrain periaqueductal gray (PAG) co-ordinates an animal's behavioral, somatic, and autonomic responses to various forms of threat, stress, and pain (Keay and Bandler, 2001). The PAG receives a relatively dense network of cholecystokinin immunoreactive nerve fibers (Kubota et al, 1983; Liu et al, 1994), many of which arise from the midbrain tegmentum (Luo et al, 1998). Although CCK2 receptors are the predominant CCK receptor within the brain, both CCK1 and CCK2 receptors are present within the PAG (Carlberg et al, 1992; Mercer and Beart, 2004; Mercer et al, 1996). Microinjection of cholecystokinin into the PAG reduces opioid-induced analgesia and increases anxiety-related behaviors, blood pressure and defensive behavior. The functions of cholecystokinin are largely thought to be mediated by CCK2 receptors (Bertoglio and Zangrossi, 2005; Brack et al, 2006; Li and Han, 1989; Luo et al, 1998; Netto and Guimaraes, 2004; Tortorici et al, 2003). These studies have also shown that PAG microinjection of cholecystokinin antagonists, particularly CCK2 ligands, into the PAG enhances morphine-induced analgesia and reduces morphine tolerance, facilitates defensive rage behavior and has an anxiolytic effect (Bertoglio and Zangrossi, 2005; Li and Han, 1989; Luo et al, 1998; Tortorici et al, 2003).
In vitro studies have shown that cholecystokinin increases the excitability of PAG neurons (Brack and Lovick, 2007; Liu et al, 1994). Cholecystokinin, however, has complex effects on PAG neurons, including inhibition of voltage-dependent calcium currents, a potassium current and the apamin-sensitive after-hyperpolarization (Yang et al, 2006, 2007). In addition, cholecystokinin increases spontaneous miniature glutamatergic synaptic transmission within the PAG via a presynaptic mechanism (Yang et al, 2006). Although functional studies have shown that the GABAergic system has a key role in the modulation of pain and anxiety within the PAG (Fields et al, 2006; Graeff et al, 1993), the effect of cholecystokinin on GABAergic synaptic transmission within this brain structure is unknown. We have recently demonstrated that activation of other Gq-coupled receptors, including metabotropic glutamate (mGluR5), muscarinic (M1 mAChR), neurokinin (NK1/2), and neurotensin (NTS1/2) receptors, indirectly inhibits GABAergic synaptic transmission via the endocannabinoid system within the PAG (Drew et al, 2008, 2009; Lau and Vaughan, 2008; Mitchell et al, 2009). In this regard, cannabinoid agonists and endocannabinoids modulate analgesic and anxiolytic activity within the PAG, including a component of stress-induced analgesia (Finn et al, 2003; Hohmann et al, 2005; Lichtman et al, 1996; Moreira et al, 2007). In this study, we therefore examined the effect of cholecystokinin on PAG neurons and GABAergic synaptic transmission, also the role of the endocannabinoid system in these processes.
METHODS
Slice Preparation
Experiments were carried out on male and female Sprague-Dawley rats (15–24 days old), following the guidelines of the National Health and Medical Research Council ‘Australian code of practice for the care and use of animals for scientific purposes’ and with the approval of the Royal North Shore Hospital Animal Care and Ethics Committee. Animals were deeply anaesthetized with isoflurane, decapitated, and coronal midbrain slices (300 μm) containing PAG were cut using a vibratome (VT1000S, Leica Microsystems, Nussloch, Germany) in ice-cold artificial cerebrospinal fluid (ACSF), of the following composition: (in mM): NaCl 126, KCl 2.5, NaH2PO4 1.4, MgCl2 1.2, CaCl2 2.4, glucose 11, NaHCO3 25, as described previously (Drew et al, 2008). The slices were maintained at 34°C in a submerged chamber containing ACSF equilibrated with 95% O2 and 5% CO2. Individual slices were then transferred to a chamber and superfused continuously (1.8 ml/min) with ACSF at 34°C. In experiments where external K+ was elevated (KCl 17.5 mM), NaCl was reduced to 111 mM to maintain constant osmolality.
Electrophysiology
PAG neurons were visualized using infrared Dodt contrast gradient optics on an upright microscope (BX50; Olympus, Tokyo, Japan). Whole-cell voltage-clamp recordings at −60 mV (liquid junction potential corrected) were made using an Axopatch 200B (Molecular Devices, Sunnyvale, USA), with an internal solution comprising (mM): K-gluconate 95, KCl 30, NaCl 15, MgCl2 2, HEPES 10, EGTA 11, MgATP 2, and NaGTP 0.3 for recording direct postsynaptic effects, or with an internal solution containing (in mM): CsCl 140, Hepes 10, EGTA 0.2, MgCl2 1, MgATP 2, NaGTP 0.3, and QX-314 3 for recording effects on evoked and miniature postsynaptic currents; both with pH of 7.3 and osmolality of 280–285 mosmol/l. Series resistance (<30 MΩ) was compensated by 80% and continuously monitored during the experiments.
Electrically evoked inhibitory postsynaptic currents (IPSCs) were elicited in neurons via unipolar glass electrodes (containing ACSF) placed 20–100 μm from the recording electrode (stimuli: 5–50 V, 20–400 μs), in the presence of the non-NMDA glutamate receptor antagonist CNQX (5 μM), and the glycine receptor antagonist strychnine (5 μM). Spontaneous miniature IPSCs were recorded in the presence of tetrodotoxin (300 nM), CNQX (5 μM), and strychnine (5 μM). Evoked and miniature IPSCs were abolished by the GABAA antagonist SR95531 (10 μM, n=4, 5). Spontaneous excitatory postsynaptic currents (EPSCs) were obtained in the presence of picrotoxin (100 μM) and strychnine (5 μM), and were abolished by CNQX (5 μM, n=3).
Analysis
Recordings of currents to examine direct postsynaptic effects were filtered (1 kHz low-pass filter) and sampled (2 kHz) for analysis (Axograph X, Axograph Scientific Software, Sydney, Australia). IPSCs and EPSCs were filtered (2, 5 kHz low-pass filter) and sampled (5, 10 kHz) for on-line and later off-line analysis (Axograph X). Spontaneous IPSCs and EPSCs were sampled in 5 s epochs every 6 s, and PSCs above a preset threshold (4–5 SD above baseline noise) were automatically detected by a sliding template algorithm, then manually checked off-line. All numerical data are expressed as mean±SEM. Statistical comparisons of mean drug effects were made using paired Student's t-test, and comparisons between multiple treatment groups with a one-way ANOVA (using Dunnett's correction for post-hoc comparisons), or a two-way ANOVA (using Bonferroni's correction for post-hoc comparisons). Comparisons of proportions were made using Chi-squared, or Fisher's exact tests. Comparisons of individual cumulative probability distributions of IPSC/EPSC amplitude and rate were made using the Kolmogorov–Smirnov (K-S) test. Differences were considered significant, if p<0.05.
Drug Solutions
Sulfated cholecystokinin(26–33) (CCK-S) was obtained from Auspep (Parkville, Australia) and Sigma-Aldrich (Sydney, Australia) (CCK-S from both sources produced similar effects); atropine, (±)−baclofen, non-sulfated cholecystokinin-(26–33) (CCK-NS), methionine enkephalin (met-enkephalin), picrotoxin, strychnine hydrochloride, and (−)-tetrahydrolipstatin from Sigma-Aldrich (Sydney, Australia); 1-(2,4-dichlorophenyl)-5-(4-iodophenyl)-4-methyl-N-1-piperidinyl-1H-pyrazole-3-carboxamide (AM251) from Cayman Chemicals (Ann Arbor, USA); CI988 (PD-134,308), devazepide (L-364,718), L732138, LY225910, 2-Methyl-6-(phenylethynyl)pyridine hydrochloride (MPEP), and SR142948 from Tocris Bioscience (Bristol, UK); 6-Cyano-7-nitroquinoxaline-2,3-dione disodium (CNQX), QX314, SR95531 and tetrodotoxin (TTX) from Ascent Scientific (Bristol, UK). Stock solutions of all drugs were made in distilled water, except AM251 and MPEP, which were made in dimethylsulfoxide. All agents were diluted to working concentrations in ACSF (solvent ⩽0.03% v/v) immediately before use and applied by superfusion. Cholecystokinin, cannabinoid, and mGluR agents were used at concentrations that have previously been shown to be maximally effective in PAG slices (Drew et al, 2009; Drew et al, 2008; Yang et al, 2007). The entire system was washed in 30% ethanol after AM251 experiments.
RESULTS
Cholecystokinin Produces Inward Currents in Opioid-Sensitive and Insensitive Neurons
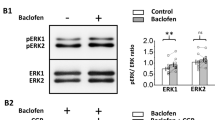
Superfusion of supramaximal concentrations of sulfated cholecystokinin-(26–33) (CCK-S, 100–300 nM) produced an inward current in a sub-population of PAG neurons (Figures 1a and b, 71% of neurons, n=48/68, inward current at 100 nM and 300 nM=29±7 pA and 22±3 pA). Subsequent superfusion of the GABAB agonist baclofen (10 μM) produced an outward current in all neurons that did, or did not respond to CCK-S (Figures 1a and b). The proportion of CCK-S responding neurons was similar in the dorsolateral (75%, n=6/8), lateral (68%, n=23/34), and ventrolateral PAG columns (73%, n=19/26) (p=0.9). CCK-S produced an inward current in similar proportions of neurons that did (n=37/49), or did not (n=5/8) respond with an outward current to the μ/δ-opioid agonist met-enkephalin (10 μM) (Figures 1a, b and ci, p=0.4). The CCK-S-induced current was similar in met-enkephalin responding and non-responding neurons (Figure 1cii, p=0.9). The inward current produced by CCK-S (100–300 nM) persisted in the combined presence of tetrodotoxin (300 nM), CNQX (3 μM), picrotoxin (100 μM), and strychnine (3 μM) (mean inward current=18±2 pA, n=8).
Cholecystokinin produces an inward current in sub-populations of μ-opioid sensitive and insensitive neurons. Current traces of opioid (a) sensitive and (b) insensitive PAG neurons during superfusion of met-enkephalin (ME, 10 μM), sulfated cholecystokinin-(26–33) (CCK-S, 300 nM) and baclofen (10 μM). (c) Bar charts depicting the (i) percentage of neurons that responded to CCK-S with an inward current, and (ii) the average inward current in CCK-S-responding neurons for ME responding and non-responding neurons (ME +ve and −ve). (d) Current–voltage relationship for the neuron in (b) before (control), during (CCK-S), and after washout (wash) of CCK-S and then during baclofen. Membrane currents were evoked by voltage steps in 10 mV increments from –50 mV to –120 mV (250 ms duration). Current traces in (a and b) are from different neurons.
The inward current produced by CCK-S (100–300 nM) was associated with a near parallel inward shift in the current–voltage relationship (Figure 1d). The mean slope conductance in these neurons was 2.6±0.3 nS and 4.1±0.5 nS in the absence and 2.9±0.4 nS and 4.0±0.6 nS in the presence of CCK-S, when measured between –60/–90 mV and –110/–130 mV (n=9). By contrast, baclofen (10 μM) produced an outward current which reversed polarity at –108±3 mV (Figure 1d, n=9). In these neurons, baclofen (10 μM) increased the slope conductance from 2.5±0.3 nS and 4.0±0.6 nS to 3.5±0.4 nS and 4.9±0.7 nS, when measured between –60/–90 mV and –110/–130 mV.
Cholecystokinin Exerts an Effect Largely Via Postsynaptic CCK1 Receptors
We next examined whether these effects were mediated by CCK1, or CCK2 receptors. The selective CCK2 agonist non-sulfated cholecystokinin-(26–33) (CCK-NS, 100–1 μM) had no effect on membrane current in all neurons tested (Figure 2a, mean current=−0.5±0.3 pA, p=0.1, n=17). In 6/10 of these neurons, subsequent superfusion of CCK-S (100 nM) produced an inward current (Figure 2a). All of these neurons subsequently responded to baclofen with an outward current (Figure 2a, n=17).
The postsynaptic effects of cholecystokinin are largely mediated by CCK1 receptors. (a) Current trace of a neuron during superfusion of non-sulfated cholecystokinin-(26–33) (CCK-NS, 100 nM), sulfated cholecystokinin-(26–33) (CCK-S, 100 nM), and baclofen (Bacl, 10 μM). (b, c) Current traces of two neurons during repeated application of CCK-S (100 nM) at a 10 min interval, and then baclofen (10 μM). In (c) devazepide (1 μM) was added after the first washout of CCK-S. (d) Bar chart showing the inward currents produced during two consecutive applications of 100 nM CCK-S (CCK 1st and 2nd), in which either no antagonist (Ctl, Control), devazepide (Devaz, 100 nM, 1 μM), CI988 (100 nM, 1 μM), or LY225910 (LY, 1 μM) was applied continuously after washout of the first application of CCK-S. In (d) *p<0.05 and **p<0.01 (t-tests for 1st and 2nd CCK-S currents individually), #p<0.05, ##p<0.01 and ###p<0.001 for post-hoc comparisons between 1st and 2nd CCK-S currents for individual treatment groups with two-way ANOVA. Current traces in (a–c) are from different neurons.
We also examined the effect of CCK1/2 receptor antagonists on the response to CCK-S in neurons, which initially responded to CCK-S. To do this, cholecystokinin (100 nM) was applied twice at a 10–12 min interval with, or without addition of selective CCK1 (devazepide), or CCK2 (CI988, LY225910) receptor antagonists after the first application of cholecystokinin (Figures 2b and c). The current produced by the first and second applications of CCK-S differed significantly across treatment groups (Figure 2b, p=0.008, F5,23=4.19). When no antagonist was added, CCK-S produced inward currents, which were similar during the first and second applications (Figures 2b and d, n=5, p>0.05). In neurons that initially responded to CCK-S with an inward current, subsequent application of CCK-S did not produce a change in membrane current in the presence of 100 nM, or 1 μM devazepide (Figures 2c and d, p=0.6 and 0.1, n=4, 5). In neurons that initially responded to CCK-S with an inward current, subsequent application of CCK-S produced an inward current in the presence of 100 nM, or 1 μM CI988 (Figure 2d, p=0.02 and 0.01, n=6, 5). Similarly, in neurons that initially responded to CCK-S with an inward current, subsequent application of CCK-S in the presence of LY225910 (1 μM) produced an inward current (Figure 2d, p=0.003, n=5). The CCK-S-induced inward current was, however, less in the presence of CI988 (1 μM), or LY225910 (1 μM) than in their absence (Figure 2d, p<0.05). Subsequent application of baclofen (10 μM) produced an outward current in these neurons, which was similar in the absence and presence of devazepide, CI988, and LY225910 (Figures 2a–c, p=0.2).
Cholecystokinin Inhibits Evoked IPSCs
In the presence of CNQX (5 μM) and strychnine (3 μM), superfusion of CCK-S (300 nM), but not CCK-NS (300 nM) produced a reduction in the amplitude of evoked GABAA-mediated IPSCs in PAG neurons (Figures 3a and b). On average, the amplitude of evoked IPSCs in the presence of CCK-S and CCK-NS was 75±3% (p<0.0001) and 99±2% (p=0.7) of the pre-CCK-S and CCK-NS levels (Figure 3d, n=22, 11). Subsequent application of baclofen (10 μM, p<0.0001), or met-enkephalin (10 μM, p=0.0004) produced a reduction in evoked IPSC amplitude (Figures 3a and b, 18 (7 and 45±4% of pre-baclofen and met-enkephalin levels, n=9, 5).
Cholecystokinin inhibits evoked inhibitory postsynaptic currents (IPSCs). (a) Time course of evoked IPSC amplitude (eIPSC Ampl) during application of non-sulfated cholecystokinin-(26–33) (CCK-NS, 300 nM), sulfated cholecystokinin-(26–33) (CCK-S, 300 nM), and then baclofen (10 μM). (b) Averaged evoked IPSCs before (Pre), and during application of CCK-NS, CCK-S, and baclofen. (c) Averaged evoked IPSCs in response to identical paired stimuli (inter-stimulus interval=80 ms) before (Pre) and during CCK-NS and CCK-S, with IPSC1 normalized to demonstrate relative facilitation of IPSC2 during superfusion of CCK-S. (d) Scatter plot showing the amplitude of the first evoked IPSC (eIPSC1) and the ratio of evoked IPSC2/IPSC1 (eIPSC2 : 1) in the presence of CCK-NS and CCK-S expressed as a percentage of the pre-CCK-NS and CCK-S values, respectively. In (d) ***p<0.001. Traces in (a–c) are from the same neuron. In (b–c) stimulus artifacts have been blanked for clarity.
In these neurons, paired evoked IPSCs were elicited by two stimuli of identical strength in close succession (inter-stimulus interval=70 ms) to determine whether the CCK-S-induced inhibition of the first evoked IPSC was associated with relative facilitation of the second evoked IPSC. Initially, the mean ratio of the amplitude of the paired evoked IPSCs was 0.91±0.05, with both paired-pulse depression and facilitation being observed (Figure 3c, evoked IPSC2/evoked IPSC1 range: 0.46−1.43, n=22). Application of CCK-S (p<0.0001), but CCK-NS (p=0.6) produced a significant increase in the paired-pulse ratio of evoked IPSCs (Figures 3c and d, n=22, 11). There was no correlation between the initial paired-pulse ratio of evoked IPSCs and the subsequent CCK-S-induced inhibition of the first evoked IPSC (r2=0.12, p=0.1).
Cholecystokinin Does not Affect Miniature IPSCs
The above experiments indicate that cholecystokinin exerts an effect by reducing GABA release. We next examined the effect of CCK-S on Na+-channel-independent (TTX-resistant) spontaneous miniature IPSCs. In the presence of CNQX (5 μM), strychnine (3 μM), and TTX (300 nM), superfusion of CCK-S (300 nM) did not significantly affect the rate (p=0.6), or amplitude (p=0.8) of miniature IPSCs (Figures 4a, b, and f, n=8). In these neurons, superfusion of met-enkephalin (10 μM) reduced the rate (p=0.003), but had no effect on the amplitude (p=0.5) of miniature IPSCs (Figures 4a, b and f, n=5). Met-enkephalin produced a rightward shift, but CCK-S did not alter the miniature IPSC inter-event interval cumulative probability distribution (Figure 4c). Both CCK-S and met-enkephalin had no effect on the kinetics of miniature IPSCs, or their amplitude cumulative probability distributions (Figures 4d–e).
Effect of cholecystokinin on miniature IPSCs. (a) Time course of miniature inhibitory postsynaptic current (IPSC) (mIPSC) rate during superfusion of sulfated cholecystokinin-(26–33) (CCK-S, 300 nM) and met-enkephalin (ME, 10 μM) in normal artificial cerebrospinal fluid (ACSF). (b) Raw current traces of miniature IPSCs before (Pre) and during superfusion of CCK-S and ME. Cumulative probability distribution plots of miniature IPSC, (c) inter-event interval, and (d) amplitude, before and during superfusion of CCK-S and ME. (e) Averaged traces of miniature IPSCs before and during superfusion of CCK-S and ME, for the corresponding epochs used in (c) and (d). (f) Bar chart of the mean rate and amplitude of miniature IPSCs in the presence of CCK-S and ME, expressed as a percentage of the pre-drug value, in normal ACSF (K+=2.5 mM) and in elevated external K+ (17.5 mM). In (f) **p<0.01 and ***p<0.001. Traces in (a–e) are from the same neuron.
Under basal conditions, miniature IPSCs within the PAG are largely Ca2+ independent (Vaughan and Christie, 1997). The lack of effect CCK-S on miniature IPSCs may have been because CCK-S modulation of GABAergic synaptic transmission is mediated via inhibition of presynaptic voltage-dependent calcium channels, as observed previously for somatostatin (Connor et al, 2004). We therefore examined the effect of CCK-S on miniature IPSCs under conditions, in which voltage-dependent calcium currents are tonically active. When the external concentration of potassium was elevated ([K+]ext=17.5 mM), CCK-S (300 nM) produced a reduction in miniature IPSC rate in two neurons (rate=48 and 65% of pre-CCK-S, inter-event interval cumulative probability distributions p<0.01) and had no effect in the other eight neurons (rate=85–111% of pre-CCK-S, inter-event interval cumulative probability distributions p>0.05). When averaged across all neurons, CCK-S did not significantly affect miniature IPSC rate (Figure 4f, p=0.08, n=10). Under these conditions, met-enkephalin (10 μM) reduced the miniature IPSC rate (Figure 4f, p<0.0001, n=10). CCK-S and met-enkephalin had no effect on the amplitude of miniature IPSCs (Figure 4f, p=0.3 and 0.2). The relatively minor inhibitory effect of CCK-S on miniature IPSCs, compared with evoked IPSCs suggests that it was exerting an effect via an indirect upstream mechanism external to the synapse.
Cholecystokinin Inhibits IPSCs Via an mGluR5-endocannabinoid-Dependent Mechanism
We have recently demonstrated that activation of Gq-coupled NK1 and NTS1/2 receptors inhibit GABAergic synaptic transmission by elevating endogenous glutamate, which engages mGluR5-induced endocannabinoid signaling (Drew et al, 2009; Mitchell et al, 2009). To address this, we first examined whether CCK-S increased action potential-dependent release of glutamate. CCK-S (300 nM) produced an increase in the rate of spontaneous EPSCs in 6/12 neurons tested (120–930% of pre-CCK-S, inter-event interval cumulative probability distributions p<0.001). By contrast, met-enkephalin (10 μM) produced a reduction in the rate of spontaneous EPSCs in all neurons tested (60±7% of pre-met-enkephalin, p<0.01, n=6). CCK-S and met-enkephalin had no effect on the amplitude of spontaneous EPSCs (107±7 and 101±1% of pre-CCK-S and met-enkephalin, p=0.4, 0.6, n=12, 6).
We next examined the role of mGluR5 and cannabinoid CB1 receptors in the CCK-S-induced inhibition of evoked IPSCs. Unlike control untreated slices, addition of CCK-S (300 nM) had no effect on the amplitude, or the paired-pulse ratio of evoked IPSCs in PAG neurons from slices pre-incubated in the mGluR5 antagonist MPEP (10 μM) (Figures 5a and d, p=0.8, 0.9, n=5). In slices pre-incubated in the cannabinoid CB1 receptor antagonist/inverse agonist AM251 (3 μM), addition of CCK-S did not have a significant effect on the amplitude of evoked IPSCs, or the paired-pulse ratio of evoked IPSCs (Figures 5b and d, p=0.4 and 0.1, n=5). In slices pre-incubated in the 1,2-diacylglycerol lipase (DAGLα) inhibitor tetrahydrolipstatin (10 μM), did not have a significant effect on the amplitude of evoked IPSCs, or the paired-pulse ratio of evoked IPSCs (Figures 5c and d, p=0.9 and 0.1, n=4). Finally, in slices pre-incubated in the NK1, NTS1/2 and mAChR antagonists L732138 (10 μM), SR142948 (300 nM) and atropine (1 μM), addition of CCK-S produced a reduction in the amplitude of evoked IPSCs (p=0.005) and an increase in the paired-pulse ratio of evoked IPSCs (p=0.03) (Figure 5d, n=6), which was not significantly different to that produced by CCK-S alone (p>0.05). This suggests that CCK-induced inhibition is independent of other receptor systems, which induce endocannabinoid signaling within PAG.
Cholecystokinin inhibition of evoked inhibitory postsynaptic currents (IPSCs) is mediated by mGluR5-induced endocannabinoid signaling. Traces of averaged evoked IPSCs before and after addition of sulfated cholecystokinin-(26–33) (CCK-S, 300 nM) in PAG neurons from slices, which were pre-incubated in either (a) the mGluR5 antagonist MPEP (5 μM), (b) the cannabinoid CB1 antagonist AM251 (1 μM), or (c) the DAG lipase inhibitor tetrahydrolipstatin (THL, 10 μM). (d) Bar chart showing the effect of CCK-S (300 nM) on the first evoked IPSC (eIPSC1) and the ratio of evoked IPSC2/IPSC1 (eIPSC2 : 1), in control untreated slices (Ctl) and slices pre-incubated in either MPEP, AM251, THL, or a cocktail of NK1 (L732138 10 μM), NTS1/2 (SR142948 300 nM) and mAChR (atropine 1 μM) antagonists (Cktail). The data in (d) is the mean eIPSC amplitude and eIPSC2 : 1 ratio in the presence of CCK-S expressed as a percentage of the pre-CCK-S value. In (d) *p<0.05, **p<0.01 and ***p<0.001 (comparing values before and during addition of CCK-S). Traces in (a–c) are from different neurons, and stimulus artifacts have been blanked for clarity.
DISCUSSION
This study has demonstrated that cholecystokinin exerts an effect largely via CCK1 receptors to modulate PAG neuronal activity by two partially overlapping mechanisms. These include direct postsynaptic excitation, plus downstream inhibition of GABAergic synaptic transmission via mGluR-induced endocannabinoid signaling. These observations provide a cellular basis for the modulation of pain and anxiety by cholecystokinin within the PAG, also the potential for an interaction with the endocannabinoid system.
Sulfated cholecystokinin-(26–33) (CCK-S), but not non-sulfated cholecystokinin-(26–33) (CCK-NS) produced an inward current in PAG neurons at concentrations between 100–300 nM. This suggests that the effects of cholecystokinin were mediated by CCK1 receptors because CCK-S has low nanomolar affinity for both CCK1 and CCK2 receptors, whereas CCK-NS only has low nanomolar affinity for CCK1 receptors (eg, Smeets et al, 1998). To confirm this, we also examined the effect on CCK-S-induced currents of the selective antagonists devazepide and CI-988, which have low nanomolar affinity for CCK1 and CCK2 receptors, respectively (Noble et al, 1999). The CCK-S (100 nM) current was abolished by devazepide at both 100 nM and 1 μM concentrations. By contrast, CI988 had no effect and only partially reduced the CCK-S-induced current at 100 nM and 1 μM concentrations, respectively. In addition, the CCK2 receptor antagonist LY225910 (1 μM) partially reduced the CCK-S-induced inward current. Together, these results suggest that the cholecystokinin-induced inward current is largely mediated by CCK1 receptors; however, a role for CCK2 receptors cannot be excluded. The present results differ to previous studies in the PAG where the postsynaptic effects of CCK-S were largely abolished by the CCK2 receptor antagonist L-365, 260 (10 μM), but not by 10 μM devazepide (Yang et al, 2006, 2007). It might also be noted that CCK2 antagonists have been reported to block the increase in firing rate of PAG neurons, also the anxiety-related activity, defensive rage, and the pro-nociceptive/anti-opioid effects produced by CCK-S and pentagastrin within the PAG (Bertoglio and Zangrossi, 2005; Brack and Lovick, 2007; Chen et al, 1998; Liu et al, 1994; Luo et al, 1998; Netto and Guimaraes, 2004; Tortorici et al, 2003). Although these findings suggest that CCK1 receptors alter neuronal excitability within the PAG, the role of CCK1 receptors in the coordinated functions of the PAG remain to be determined, and may differ to that of CCK2 receptors.
CCK-S produced an inward current in ∼75% of PAG neurons, some of which were opioid responsive. This is similar to the proportion of neurons that respond to the Gq-coupled excitatory neurotransmitters neurotensin and substance P within the PAG (Drew et al, 2005; Mitchell et al, 2009). Thus, like substance P and neurotensin, cholecystokinin has a direct excitatory effect on PAG neurons, which opposes the postsynaptic inhibitory functions of μ-opioids. Many of these CCK-S-responding neurons were likely to be interneurons, because relatively few PAG neurons are output projection neurons (Reichling and Basbaum, 1990) and only a small proportion of PAG output neurons are opioid responsive (Osborne et al, 1996). This suggests that a range of Gq-coupled GPCRs activate similar sub-populations of PAG interneurons. The CCK-S-induced inward current was likely to be mediated by activation of a non-selective cation conductance and inhibition of an inwardly rectifying potassium conductance, because it was associated with a near parallel shift in the current–voltage relationship. Although this differs to a previous study, in which it was found that CCK-S exerted an effect solely by inhibiting an inwardly rectifying potassium conductance in dorsolateral PAG neurons (Yang et al, 2006, 2007), it is similar to our previous findings for neurotensin and substance P (Drew et al, 2005; Mitchell et al, 2009).
CCK-S, but not CCK-NS also produced a reduction in GABAA-mediated evoked IPSCs, suggesting that the inhibition of GABAergic synaptic transmission was also largely mediated by CCK1 receptors. In a number of brain regions it has been demonstrated that activation of postsynaptic Gq-coupled GPCRs inhibits synaptic transmission via retrograde endocannabinoid signaling (Kano et al, 2009). In this regard, we have previously shown that postsynaptic mGluR5 and M1 mAChR activation produces endocannabinoids that travel retrogradely across the synapse to activate cannabinoid CB1 receptors on presynaptic nerve terminals, reducing the probability of GABA release and thereby inhibiting synaptic transmission onto that neuron (Drew et al, 2008; Lau and Vaughan, 2008; see also Figure 6). These findings suggest that the cholecystokinin-induced inhibition of evoked IPSCs is also mediated by the endocannabinoid system, because it was abolished by the cannabinoid CB1 antagonist/inverse agonist AM251. Furthermore, the endocannabinoid involved in this process was likely to be 2-arachidonyl glycerol because the CCK-S-induced inhibition was blocked by an inhibitor of DAGLα, the enzyme which mediates its production via Gq-coupled GPCRs in a number of brain regions, including the PAG (Bisogno et al, 2003; Drew et al, 2009; Jung et al, 2005; Lau and Vaughan, 2008; Uchigashima et al, 2007).
Proposed model for CCK-induced suppression of GABAergic transmission in PAG. Cholecystokinin (CCK) activates postsynaptic CCK1 (and possibly CCK2) receptors located on glutamatergic (GLU) neurons (1) to elicit action potential (AP)-driven glutamate release (2). This endogenous glutamate then activates postsynaptic mGluR5 receptors (3), which causes the production of the endocannabinoid 2-arachidonoylglycerol (2-AG) via the enzyme 1,2-diacylglycerol lipase (DAGLα) (4). 2-AG leaves the postsynaptic neuron, exerts an effect as a retrograde messenger to activate presynaptic cannabinoid CB1 receptors located on the terminals of GABAergic neurons (5) and reduces GABA release (6). The subsequent inhibition of GABAergic synaptic transmission (7) leads to disinhibition (excitation) of the postsynaptic neuron. It might be noted that the CCK-induced endocannabinoid inhibition of GABAergic synaptic transmission will be enhanced by agonists exerting an effect at presynaptic μ-opioid receptors (8). By contrast, neuronal excitation produced by postsynaptic CCK1 receptor activation will oppose postsynaptic μ-opioid receptor-mediated inhibition (9).
The CCK-S-induced inhibition of GABAergic synaptic transmission was likely to be mediated by a presynaptic mechanism because it was associated with an increase in the evoked IPSC paired-pulse ratio, as observed previously for opioids and cannabinoids within the PAG (Vaughan and Christie, 1997; Vaughan et al, 2000). CCK-S, however had little effect on the rate of spontaneous action potential-independent miniature IPSCs in the presence of TTX, either under basal conditions, or when presynaptic calcium channel activation was enhanced. The lack of effect of cholecystokinin on TTX-resistant miniature IPSCs suggests that the cholecystokinin-induced reduction in presynaptic GABA release involved additional mechanisms external to the synapse, rather than direct postsynaptic CCK1 receptor-induced retrograde endocannabinoid signaling, as observed for mGluR5 and M1 mAChR receptor signaling in PAG (Drew et al, 2008; Lau and Vaughan, 2008). We have previously shown that activation of Gq-coupled NK1 and NTS1/2 receptors indirectly activates the mGluR5-endocannabinoid system by enhancing endogenous glutamate release (Drew et al, 2009; Mitchell et al, 2009). In this study, CCK-S produced neuronal depolarization and an increase in spontaneous action potential-dependent glutamatergic EPSCs, however, we cannot rule out a direct CCK receptor-mediated enhancement of presynaptic glutamate release (Yang et al, 2006). In addition, the cholecystokinin-induced inhibition of evoked IPSCs was abolished by the mGluR5 antagonist MPEP. These observations suggest that cholecystokinin exerts an effect via a complex network involving CCK1/2-mediated postsynaptic neuronal excitation, leading to enhanced action potential-dependent glutamate release and postsynaptic mGluR5-induced retrograde endocannabinoid signaling (Figure 6).
The PAG is a major site of the analgesic and anxiolytic functions of cannabinoids and opioids (Finn et al, 2003; Hohmann et al, 2005; Lichtman et al, 1996; Moreira et al, 2007; Resstel et al, 2008). Functional studies have shown that cholecystokinin opposes the analgesic and anxiolytic functions of opioids and cannabinoids within the PAG (Li and Han, 1989; Luo et al, 1998; Netto and Guimaraes, 2004). The modulation of pain and anxiety from within the PAG is intimately linked to GABAergic mechanisms (Fields et al, 2006; Graeff et al, 1993). In particular, opioids and cannabinoids activate PAG output neurons by reducing GABAergic inhibition of these neurons, a process known as disinhibition (Fields et al, 2006). At the cellular level, disinhibition is observed as direct postsynaptic inhibition of opioid-sensitive interneurons and presynaptic inhibition of GABA release (Osborne et al, 1996; Vaughan and Christie, 1997; Vaughan et al, 2000). In this study, cholecystokinin produced postsynaptic excitation of a substantial sub-population of opioid-sensitive neurons within the PAG, providing a cellular substrate for its anti-opioid functions (Figure 6). These findings suggest that cholecystokinin may interact with opioids and cannabinoids in a more complex manner than simple functional antagonism. The postsynaptic excitatory and inhibitory effects of cholecystokinin and opioids only overlapped in sub-populations of PAG neurons, also cannabinoids have no postsynaptic effects within PAG (Vaughan et al, 2000). In addition, like opioids and cannabinoids, cholecystokinin inhibited GABAergic synaptic transmission in most neurons (Figure 6), and this would be expected to have an additive effect. It is also possible that the net effect of cholecystokinin on pain and anxiety changes when the balance of neuronal activity is altered by chronic stress and pain. Interestingly, the presynaptic inhibition produced by cholecystokinin was mediated by mGluR5-induced endocannabinoid signaling. Although the role of endocannabinoids in the behavioral functions of cholecystokinin within the PAG are unknown, there is evidence for a functional link between these systems in the control of stress, pain and conditioned fear within other brain regions (Chhatwal et al, 2009; Kurrikoff et al, 2008).
References
Bertoglio LJ, Zangrossi Jr H (2005). Involvement of dorsolateral periaqueductal gray cholecystokinin-2 receptors in the regulation of a panic-related behavior in rats. Brain Res 1059: 46–51.
Bisogno T, Howell F, Williams G, Minassi A, Cascio MG, Ligresti A et al (2003). Cloning of the first sn1-DAG lipases points to the spatial and temporal regulation of endocannabinoid signaling in the brain. J Cell Biol 163: 463–468.
Brack KE, Jeffery SM, Lovick TA (2006). Cardiovascular and respiratory responses to a panicogenic agent in anaesthetised female Wistar rats at different stages of the oestrous cycle. Eur J Neurosci 23: 3309–3318.
Brack KE, Lovick TA (2007). Neuronal excitability in the periaqueductal grey matter during the estrous cycle in female Wistar rats. Neuroscience 144: 325–335.
Carlberg M, Gundlach AL, Mercer LD, Beart PM (1992). Autoradiographic localization of cholecystokinin A and B receptors in rat brain using [125I]d-Tyr25 (Nle28,31)-CCK 25–33S. Eur J Neurosci 4: 563–573.
Chen XH, Geller EB, Adler MW (1998). CCK(B) receptors in the periaqueductal grey are involved in electroacupuncture antinociception in the rat cold water tail-flick test. Neuropharmacology 37: 751–757.
Chhatwal JP, Gutman AR, Maguschak KA, Bowser ME, Yang Y, Davis M et al (2009). Functional interactions between endocannabinoid and CCK neurotransmitter systems may be critical for extinction learning. Neuropsychopharmacology 34: 509–521.
Connor M, Bagley EE, Mitchell VA, Ingram SL, Christie MJ, Humphrey PPA et al (2004). Cellular actions of somatostatin on rat periaqueductal grey neurons in vitro. Br J Pharmacol 142: 1273–1280.
Drew GM, Lau BK, Vaughan CW (2009). Substance P Drives endocannabinoid-mediated disinhibition in a midbrain descending analgesic pathway. J Neurosci 29: 7220–7229.
Drew GM, Mitchell VA, Vaughan CW (2005). Postsynaptic actions of substance P on rat periaqueductal grey neurons in vitro. Neuropharmacology 49: 587–595.
Drew GM, Mitchell VA, Vaughan CW (2008). Glutamate spillover modulates GABAergic synaptic transmission in the rat midbrain periaqueductal grey via metabotropic glutamate receptors and endocannabinoid signaling. J Neurosci 28: 808–815.
Faris PL, Komisaruk BR, Watkins LR, Mayer DJ (1983). Evidence for the neuropeptide cholecystokinin as an antagonist of opiate analgesia. Science 219: 310–312.
Fields HL, Basbaum AI, Heinricher MM (2006). Central nervous systems mechanisms of pain modulation. In: McMahon SB, Koltzenburg M (eds). Textbook of Pain, 5th edn. Elsevier, Churchill Livingston: Philadelphia, pp 125–142.
Finn DP, Jhaveri MD, Beckett SRG, Roe CH, Kendall DA, Marsden CA et al (2003). Effects of direct periaqueductal grey administration of a cannabinoid receptor agonist on nociceptive and aversive responses in rats. Neuropharmacology 45: 594–604.
Graeff FG, Silveira MC, Nogueira RL, Audi EA, Oliveira RM (1993). Role of the amygdala and periaqueductal gray in anxiety and panic. Behav Brain Res 58: 123–131.
Hohmann AG, Suplita RL, Bolton NM, Neely MH, Fegley D, Mangieri R et al (2005). An endocannabinoid mechanism for stress-induced analgesia. Nature 435: 1108–1112.
Jung KM, Mangieri R, Stapleton C, Kim J, Fegley D, Wallace M et al (2005). Stimulation of endocannabinoid formation in brain slice cultures through activation of group I metabotropic glutamate receptors. Mol Pharmacol 68: 1196–1202.
Kano M, Ohno-Shosaku T, Hashimotodani Y, Uchigashima M, Watanabe M (2009). Endocannabinoid-mediated control of synaptic transmission. Physiol Rev 89: 309–380.
Keay KA, Bandler R (2001). Parallel circuits mediating distinct emotional coping reactions to different types of stress. Neurosci Biobehav Rev 25: 669–678.
Kubota Y, Inagaki S, Shiosaka S, Cho HJ, Tateishi K, Hashimura E et al (1983). The distribution of cholecystokinin octapeptide-like structures in the lower brain stem of the rat: an immunohistochemical analysis. Neuroscience 9: 587–604.
Kurrikoff K, Inno J, Matsui T, Vasar E (2008). Stress-induced analgesia in mice: evidence for interaction between endocannabinoids and cholecystokinin. Eur J Neurosci 27: 2147–2155.
Lau BK, Vaughan CW (2008). Muscarinic modulation of synaptic transmission via endocannabinoid signalling in the rat midbrain periaqueductal gray. Mol Pharmacol 74: 1392–1398.
Li Y, Han JS (1989). Cholecystokinin-octapeptide antagonizes morphine analgesia in periaqueductal gray of the rat. Brain Res 480: 105–110.
Lichtman AH, Cook SA, Martin BR (1996). Investigation of brain sites mediating cannabinoid-induced antinociception in rats: evidence supporting periaqueductal gray involvement. J Pharmacol Exp Ther 276: 585–593.
Liu H, Chandler S, Beitz AJ, Shipley MT, Behbehani MM (1994). Characterization of the effect of cholecystokinin (CCK) on neurons in the periaqueductal gray of the rat: immunocytochemical and in vivo and in vitro electrophysiological studies. Brain Res 642: 83–94.
Lovick TA (2008). Pro-nociceptive action of cholecystokinin in the periaqueductal grey: a role in neuropathic and anxiety-induced hyperalgesic states. Neurosci Biobehav Rev 32: 852–862.
Luo B, Cheu JW, Siegel A (1998). Cholecystokinin B receptors in the periaqueductal gray potentiate defensive rage behavior elicited from the medial hypothalamus of the cat. Brain Res 796: 27–37.
Mercer LD, Beart PM (2004). Immunolocalization of CCK1R in rat brain using a new anti-peptide antibody. Neurosci Lett 359: 109–113.
Mercer LD, Beart PM, Horne MK, Finkelstein DI, Carrive P, Paxinos G (1996). On the distribution of cholecystokinin B receptors in monkey brain. Brain Res 738: 313–318.
Mitchell VA, Kawahara H, Vaughan CW (2009). Neurotensin inhibition of GABAergic transmission via mGluR-induced endocannabinoid signalling in rat periaqueductal grey. J Physiol (Lond) 587: 2511–2520.
Moreira FA, Aguiar DC, Guimaraes FS (2007). Anxiolytic-like effect of cannabinoids injected into the rat dorsolateral periaqueductal gray. Neuropharmacology 52: 958–965.
Netto CF, Guimaraes FS (2004). Anxiogenic effect of cholecystokinin in the dorsal periaqueductal gray. Neuropsychopharmacology 29: 101–107.
Noble F, Wank SA, Crawley JN, Bradwejn J, Seroogy KB, Hamon M et al (1999). International Union of Pharmacology. XXI. structure, distribution, and functions of cholecystokinin receptors. Pharmacol Rev 51: 745–781.
Osborne PB, Vaughan CW, Wilson HI, Christie MJ (1996). Opioid inhibition of rat periaqueductal grey neurones with identified projections to rostral ventromedial medulla in vitro. J Physiol (Lond) 490: 383–389.
Reichling DB, Basbaum AI (1990). Contribution of brain-stem GABAergic circuitry to descending antinociceptive controls.1. GABA-immunoreactive projection neurons in the periaqueductal gray and nucleus raphe magnus. J Comp Neurol 302: 370–377.
Resstel LB, Lisboa SF, Aguiar DC, Correa FM, Guimaraes FS (2008). Activation of CB1 cannabinoid receptors in the dorsolateral periaqueductal gray reduces the expression of contextual fear conditioning in rats. Psychopharmacology 198: 405–411.
Smeets RL, Fouraux MA, van Emst-de Vries SE, De Pont JJ, Willems PH (1998). Protein kinase C-mediated inhibition of transmembrane signalling through CCK(A) and CCK(B) receptors. Brit J Pharmacol 123: 1189–1197.
Tortorici V, Nogueira L, Salas R, Vanegas H (2003). Involvement of local cholecystokinin in the tolerance induced by morphine microinjections into the periaqueductal gray of rats. Pain 102: 9–16.
Uchigashima M, Narushima M, Fukaya M, Katona I, Kano M, Watanabe M (2007). Subcellular arrangement of molecules for 2-arachidonoyl-glycerol-mediated retrograde signaling and its physiological contribution to synaptic modulation in the striatum. J Neurosci 27: 3663–3676.
Vaughan CW, Christie MJ (1997). Presynaptic inhibitory action of opioids on synaptic transmission in the rat periaqueductal grey in vitro. J Physiol (Lond) 498: 463–472.
Vaughan CW, Connor M, Bagley EE, Christie MJ (2000). Actions of cannabinoids on membrane properties and synaptic transmission in rat periaqueductal gray neurons in vitro. Mol Pharmacol 57: 288–295.
Yang YM, Chung JM, Rhim H (2006). Cellular action of cholecystokinin-8S-mediated excitatory effects in the rat periaqueductal gray. Life Sci 79: 1702–1711.
Yang YM, Chung JM, Rhim H (2007). Cholecystokinin-8S-induced intracellular calcium signaling in acutely isolated periaqueductal gray neurons of the rat. Biol Pharm Bull 30: 297–302.
Acknowledgements
This work was supported by Australian National Health and Medical Research Council grant 1003097 to CWV and GMD.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Mitchell, V., Jeong, HJ., Drew, G. et al. Cholecystokinin Exerts an Effect via the Endocannabinoid System to Inhibit GABAergic Transmission in Midbrain Periaqueductal Gray. Neuropsychopharmacol 36, 1801–1810 (2011). https://doi.org/10.1038/npp.2011.59
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/npp.2011.59
Keywords
This article is cited by
-
Whey protein supplementation reducing fasting levels of anandamide and 2-AG without weight loss in pre-menopausal women with obesity on a weight-loss diet
Trials (2020)
-
Effects of THC/CBD oromucosal spray on spasticity-related symptoms in people with multiple sclerosis: results from a retrospective multicenter study
Neurological Sciences (2020)
-
Cholecystokinin receptor-1 mediates the inhibitory effects of exogenous cholecystokinin octapeptide on cellular morphine dependence
BMC Neuroscience (2012)