Abstract
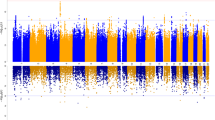
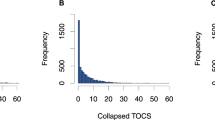
Genetic association studies of SLC6A4 (SERT) and obsessive-compulsive disorder (OCD) have been equivocal. We genotyped 1241 individuals in 278 pedigrees from the OCD Collaborative Genetics Study for 13 single-nucleotide polymorphisms, for the linked polymorphic region (LPR) indel with molecular haplotypes at rs25531, for VNTR polymorphisms in introns 2 and 7 and for a 381-bp deletion 3′ to the LPR. We analyzed using the Family-Based Association Test (FBAT) under additive, dominant, recessive and genotypic models, using both OCD and sex-stratified OCD as phenotypes. Two-point FBAT analysis detected association between Int2 (P=0.0089) and Int7 (P=0.0187) (genotypic model). Sex-stratified two-point analysis showed strong association in females with Int2 (P<0.0002), significant after correction for linkage disequilibrium, and multiple marker and model testing (PAdj=0.0069). The SLC6A4 gene is composed of two haplotype blocks (our data and the HapMap); FBAT whole-marker analysis conducted using this structure was not significant. Several noteworthy nonsignificant results have emerged. Unlike Hu et al., we found no evidence for overtransmission of the LPR LA allele (genotype relative risk=1.11, 95% confidence interval: 0.77–1.60); however, rare individual haplotypes containing LA with P<0.05 were observed. Similarly, three individuals (two with OCD/OCPD) carried the rare I425V SLC6A4 variant, but none of them passed it on to their six OCD-affected offspring, suggesting that it is unlikely to be solely responsible for the ‘OCD plus syndrome’, as reported by Ozaki et al. In conclusion, we found evidence of genetic association at the SLC6A4 locus with OCD. A noteworthy lack of association at the LPR, LPR-rs25531 and rare 425V variants suggests that hypotheses about OCD risk need revision to accommodate these new findings, including a possible gender effect.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Hu XZ, Lipsky RH, Zhu G, Akhtar LA, Taubman J, Greenberg BD et al. Serotonin transporter promoter gain-of-function genotypes are linked to OCD. Am J Hum Genet 2006; 78: 815–826.
Ozaki N, Goldman D, Kaye WH, Plotnicov K, Greenberg BD, Lappalainen J et al. Serotonin transporter missense mutation associated with a complex neuropsychiatric phenotype. Mol Psychiatry 2003; 8: 933–936.
Nestadt G, Lan T, Samuels J, Riddle M, Bienvenu III OJ, Liang KY et al. Complex segregation analysis provides compelling evidence for a major gene underlying OCD for heterogeneity by sex. Am J Hum Genet 2000; 67: 1611–1616.
Nestadt G, Samuels J, Riddle M, Bienvenu III OJ, Liang KY, Labuda M et al. A family study of OCD. Arch Gen Psychiatry 2000; 57: 358–363.
Hanna GL, Fingerlin TE, Himle JA, Boehnke M . Complex segregation analysis of OCD in families with pediatric probands. Hum Hered 2005; 60: 1–9.
Hanna GL, Veenstra-VanderWeele J, Cox NJ, Boehnke M, Himle JA, Curtis GC et al. Genome-wide linkage analysis of families with OCD ascertained through pediatric probands. Am J Med Genet 2002; 114: 541–552.
Willour VL, Yao SY, Samuels J, Grados M, Cullen B, Bienvenu III OJ et al. Replication study supports evidence for linkage to 9p24 in OCD. Am J Hum Genet 2004; 75: 508–513.
Arnold PD, Sicard T, Burroughs E, Richter MA, Kennedy JL . Glutamate transporter gene SLC1A1 associated with OCD. Arch Gen Psychiatry 2006; 63: 769–776.
Stewart SE, Fagerness JA, Platko J, Smoller JW, Scharf JM, Illmann C et al. Association of the SLC1A1 glutamate transporter gene OCD. Am J Med Genet B Neuropsychiatr Genet 2007; 144B: 1027–1033.
Dickel DE, Veenstra-VanderWeele J, Bivens NC, Wu X, Fischer DJ, Van Etten-Lee M et al. Association studies of serotonin system candidate genes in early-onset OCD. Biol Psychiatry 2007; 61: 322–329.
Wendland JR, Moya PR, Timpano KR, Anavitarte AP, Kruse MR, Wheaton MG et al. A haplotype containing quantitative trait loci for SLC1A1 gene expression and its association with OC. Arch Gen Psychiatry 2009; 66: 408–416.
Shugart YY, Samuels J, Willour VL, Grados MA, Greenberg BD, Knowles JA et al. Genome-wide linkage scan for OCD: evidence for susceptibility loci on chromosomes 3q 7p 1q 15q 6q. Mol Psychiatry 2006; 11: 763–770.
Goddard AW, Shekhar A, Whiteman AF, McDougle CJ . Serotoninergic mechanisms in the treatment of OCD. Drug Discov Today 2008; 13: 325–332.
Stengler-Wenzke K, Muller U, Angermeyer MC, Sabri O, Hesse S . Reduced serotonin transporter-availability in OCD. Eur Arch Psychiatry Clin Neurosci 2004; 254: 252–255.
Hesse S, Müller U, Lincke T, Barthel H, Villmann T, Angermeyer MC et al. Serotonin dopamine transporter imaging in patients with obsessive-compulsive disorder. Psychiatry Res 2005; 140: 63–72.
Hasselbalch SG, Hansen ES, Jakobsen TB, Pinborg LH, Lønborg JH, Bolwig TG . Reduced midbrain-pons serotonin transporter binding in patients with OCD. Acta Psychiatr Scand 2007; 115: 388–394.
Prasad HC, Zhu CB, McCauley JL, Samuvel DJ, Ramamoorthy S, Shelton RC et al. Human serotonin transporter variants display altered sensitivity to protein kinase G and p38 mitogen-activated protein kinase. Proc Natl Acad Sci USA 2005; 102: 11545–11550.
Roberts J, Scott AC, Howard MR, Breen G, Bubb VJ, Klenova E et al. Differential regulation of the serotonin transporter gene by lithium is mediated by transcription factors, CCCTC binding protein and Y-box binding protein 1, through the polymorphic intron 2 variable number tandem repeat. J Neurosci 2007; 27: 2793–2801.
Bloch MH, Landeros-Weisenberger A, Sen S, Dombrowski P, Kelmendi B, Coric V et al. Association of the SERT polymorphism and OCD: Systematic review. Am J Med Genet B Neuropsych Genet 2008; 147B: 850–858.
McDougle CJ, Epperson CN, Price LH, Gelernter J . Evidence for linkage disequilibrium between serotonin transporter protein gene (SLC6A4) and OCD. Mol Psychiatry 1998; 3: 270–273.
Bengel D, Greenberg BD, Cora-Locatelli G, Altemus M, Heils A, Li Q et al. Association of the serotonin transporter promoter regulatory region polymorphism and OCD. Mol Psychiatry 1999; 4: 463–466.
Camarena B, Rinetti G, Cruz C, Hernandez S, de la Fuente JR, Nicolini H . Association study of the serotonin transporter gene polymorphism in OCD. Int J Neuropsychopharmacol 2001; 4: 269–272.
Cavallini MC, Di Bella D, Siliprandi F, Malchiodi F, Bellodi L . Exploratory factor analysis of obsessive-compulsive patients and association with 5-HTTLPR polymorphism. Am J Med Genet 2002; 114: 347–353.
Di Bella D, Erzegovesi S, Cavallini MC, Bellodi L . OCD, 5-HTTLPR polymorphism and treatment response. Pharmacogenomics J 2002; 2: 176–181.
Kim SJ, Lee HS, Kim CH . OCD, factor-analyzed symptom dimensions and serotonin transporter polymorphism. Neuropsychobiology 2005; 52: 176–182.
Kinnear CJ, Niehaus DJ, Moolman-Smook JC, du Toit PL, van Kradenberg J, Weyers JB et al. OCD and the promoter region polymorphism (5- HTTLPR) in the serotonin transporter gene (SLC6A4): a negative association study in the Afrikaner population. Int J Neuropsychopharmacol 2000; 3: 327–331.
Frisch A, Finkel B, Michaelovsky E, Sigal M, Laor N, Weizman R . A rare short allele of the serotonin transporter promoter region (5- HTTLPR) found in an aggressive schizophrenic patient of Jewish Libyan origin. Psychiatr Genet 2000; 10: 179–183.
Walitza S, Wewetzer C, Gerlach M, Klampfl K, Geller F, Barth N et al. Transmission disequilibrium studies in children and adolescents with OCD pertaining to polymorphisms of genes of the serotonergic pathway. J Neural Transm 2004; 111: 817–825.
Chabane N, Millet B, Delorme R, Lichtermann D, Mathieu F, Laplanche JL et al. Lack of evidence for association between serotonin transporter gene (5-HTTLPR) and OCD by case control and family association study in humans. Neurosci Lett 2004; 363: 154–156.
Lin PY . Meta-analysis of the association of serotonin transporter gene polymorphism with OCD. Prog Neuropsychopharmacol Biol Psychiatry 2007; 31: 683–689.
Kilic F, Murphy DL, Rudnick G . A human serotonin transporter mutation causes constitutive activation of transport activity. Mol Pharmacol 2003; 64: 440–446.
Wendland JR, DeGuzman TB, McMahon F, Rudnick G, Tera-Wadleigh SD, Murphy DL . SERT Ileu425Val in autism, Asperger syndrome and OCD. Psychiatr Genet 2008; 18: 31–39.
Samuels JF, Riddle MA, Greenberg BD, Fyer AJ, McCracken JT, Rauch SL al. The OCD collaborative genetics study: methods and sample description. Am J Med Genet B Neuropsychiatr Genet 2006; 141: 201–207.
Rabinowitz D, Laird N . A unified approach to adjusting association tests for population admixture with arbitrary pedigree structure and arbitrary missing marker information. Hum Hered 2000; 50: 211–223.
Horvath S, Xu X, Laird NM . The family based association test method: strategies for studying general genotype-phenotype associations. Eur J Hum Genet 2001; 9: 301–306.
Martin ER, Monks SA, Warren LL, Kaplan NL . A test for linkage and association in general pedigrees: the pedigree disequilibrium test. Am J Hum Genet 2001; 68: 1065–1067.
Conneely KN, Boehnke M . So many correlated tests, so little time! Rapid adjustment of P values for multiple correlated tests. Am J Hum Genet 2007; 81; (e-pub ahead of print).
Kraft P, Stram DO . Re: the use of inferred haplotypes in downstream analysis. Am J Hum Genet 2007; 81: 863–865.
Sinnwell JP, Schaid DJ, Yu Z . R Development Core Team. R: a language and environment for statistical computing. 2008. ISBN 3–900051–07–0, http://www.R-project.org.
Statistical Analysis of Haplotypes with Traits and Covariates when Linkage Phase is Ambiguous. R package version 1.3.8. URL http://mayoresearch.mayo.edu/mayo/research/schaid_lab/software.cfm.
Flattem NL, Blakely RD . Modified structure of the human serotonin transporter promoter. Mol Psychiatry 2000; 5: 110–115.
Nakamura M, Ueno S, Sano A, Tanabe H . The human serotonin transporter gene linked polymorphism (5-HTTLPR) shows ten novel allelic variants. Mol Psychiatry 2000; 5: 32–38.
Enoch MA, Greenberg BD, Murphy DL, Goldman D . Sexually dimorphic relationship of a 5-HT2A promoter polymorphism with OCD. Biol Psychiatry 2001; 49: 385–388.
Karayiorgou M, Sobin C, Blundell ML, Galke BL, Malinova L, Goldberg P et al. Family-based association studies support a sexually dimorphic effect of COMT and MAOA on genetic susceptibility to OCD. Biol Psychiatry 1999; 45: 1178–1189.
Alsobrook JP, Zohar AH, Leboyer M, Chabane N, Ebstein RP, Pauls DL . Association between the COMT locus and OCD in females but not males. Am J Med Genet 2002; 114: 116–120.
Denys D, Van NF, Deforce D, Westenberg HG . Association between serotonergic candidate genes and specific phenotypes of OCD. J Affect Disord 2006; 91: 39–44.
Ogilvie AD, Battersby S, Bubb VJ, Fink G, Harmar AJ, Goodwim GM et al. Polymorphism in serotonin transporter gene associated with susceptibility to major depression. Lancet 1996; 347: 731–733.
Battersby S, Ogilvie AD, Smith CA, Blackwood DH, Muir WJ, Quinn JP et al. Structure of a variable number tandem repeat of the SERT gene and association with affective disorder. Psychiatr Genet 1996; 6: 177–181.
Collier DA, Arranz MJ, Sham P, Battersby S, Vallada H, Gill P et al. The serotonin transporter is a potential susceptibility factor for bipolar affective disorder. Neuroreport 1996; 7: 1675–1679.
Fan JB, Sklar P . Meta-analysis reveals association between serotonin transporter gene STin2 VNTR polymorphism and schizophrenia. Mol Psychiatry 2005; 10: 928–938, 891.
Conroy J, Meally E, Kearney G, Fitzgerald M, Gill M, Gallagher L . Serotonin transporter gene and autism: a haplotype analysis in an Irish autistic population. Mol Psychiatry 2004; 9: 587–593.
Ohara K, Suzuki Y, Ochiai M, Tsukamoto T, Tani K, Ohara K . A variable-number-tandem-repeat of the serotonin transporter gene and anxiety disorders. Prog Neuropsychopharm Biol Psychiatry 1999; 23: 55–65.
Smits KM, Smits LJ, Schouten JS, Stelma FF, Nelemans P, Prins MH et al. Influence of SERTPR and STin2 on the effect of selective serotonin reuptake inhibitors in depression: a systematic review. Mol Psychiatry 2004; 9: 433–441.
Baca-Garcia E, Vaquero-Lorenzo C, Diaz-Hernandez M, Rodriguez-Salgado B, Dolengevich-Segal H, Arrojo-Romero M et al. Association between OCD and a variable number of tandem repeats polymorphism in intron 2 of the serotonin transporter gene. Prog Neuropsychopharmacol Biol Psychiatry 2007; 31: 416–420.
Hranilovic D, Stefulj J, Schwab S, Borrmann-Hassenbach M, Albus M, Jernej B et al. SERT promoter and intron 2 polymorphisms: relationship between allelic variants and gene expression. Biol Psychiatry 2004; 55: 1090–1094.
MacKenzie A, Quinn J . A SERT gene intron 2 polymorphic region, correlated with affective disorders, has allele-dependent differential enhancer-like properties in the mouse embryo. Proc Natl Acad Sci USA 1999; 96: 15251–15255.
Lovejoy EA, Scott AC, Fiskerstrand CE, Bubb VJ, Quinn JP . The serotonin transporter intronic VNTR enhancer correlated with a predisposition to affective disorders has distinct regulatory elements within the domain based on the primary DNA sequence of the repeat unit. Eur J Neurosci 2003; 17: 417–420.
Lesch KP, Bengel D, Heils A, Sabol SZ, Greenberg BD, Petri S et al. Association of anxiety-related traits with a polymorphism in the serotonin transporter gene regulatory region. Science 1996; 274: 1527–1531.
Greenberg BD, Tolliver TJ, Huang SJ, Li Q, Bengel D, Murphy DL . Genetic variation in the SERT promoter region affects serotonin uptake in human blood platelets. Am J Med Genet 1999; 88: 83–87.
Altemus M, Murphy DL, Greenberg B, Lesch KP . Intact coding region of the serotonin transporter gene in obsessive-compulsive disorder. Am J Med Genet 1996; 67: 409–411.
Wendland JR, Moya PR, Kruse MR, Ren-Patterson RF, Jensen CL, Timpano KR et al. A novel, putative gain-of-function haplotype at SLC6A4 associates with OCD. Hum Mol Genet 2008; 17: 717–723.
Martin J, Cleak J, Willis-Owen SA, Flint J, Shifman S . Mapping regulatory variants for the serotonin transporter gene based on allelic expression imbalance. Mol Psychiatry 2007; 12: 421–422.
Kim SJ, Herzing LB, Veenstra-Vanderweele J, Lord C, Courchesne R, Leventhal BL et al. Mutation screening and transmission disequilibrium study of ATP10C in autism. Am J Med Genet 2002; 114: 137–143.
Kraft JB, Slager SL, McGrath PJ, Hamilton SP . Sequence analysis of the serotonin transporter and associations with antidepressant response. Biol Psychiatry 2005; 58: 374–381.
Delorme R, Betancur C, Wagner M, Krebs MO, Gorwood P, Pearl P et al. Support for association between the rare functional variant I425V of the serotonin transporter gene and susceptibility to OCD. Mol Psychiatry 2005; 10: 1059–1061.
Glatt CE, DeYoung JA, Delgado S, Service SK, Giacomini KM, Edwards RH et al. Screening a large reference sample to identify very low frequency sequence variants: comparisons between two genes. Nat Genet 2001; 27: 435–438.
Cross S, Kim SJ, Weiss LA, Delahanty RJ, Sutcliffe JS, Leventhal BL et al. Molecular genetics of the platelet serotonin system in first-degree relatives of patients with autism. Neuropsychopharm 2008; 33: 353–360.
Ikeda M, Iwata N, Suzuki T, Kitajima T, Yamanouchi Y, Kinoshita Y et al. No association of serotonin transporter gene (SLC6A4) with schizophrenia and bipolar disorder in Japanese patients: association analysis based on linkage disequilibrium. J Neural Transm 2006; 113: 899–905.
Levenstien MA, Ott J, Gordon D . 2006 Are molecular haplotypes worth the time and expense? A cost-effective method for applying molecular haplotypes. PLoS Genet 2006; 2: e127.
Nackley AG, Shabalina SA, Tchivileva IE, Satterfield K, Korchynskyi O, Makarov SS et al. Human COMT haplotypes modulate protein expression by altering mRNA secondary structure. Science 2006; 314: 1930–1933.
Nicodemus KK, Liu W, Chase GA, Tsai Y-Y, Fallin MD . Comparison of type I error for multiple test corrections in large single-nucleotide polymorphism studies using principal components versus haplotype blocking algorithms. BMC Genetics 2005; 6 (Suppl 1): S78.
Acknowledgements
We thank the many families who have participated in the OCGS; the OCF; Ann Pulver, PhD, Kathleen Merikangas, PhD, David Houseman, MD and Alec Wilson, PhD, for consultation; and clinicians and coordinators at each OCGS site: Providence (Maria Mancebo, PhD, Richard Marsland, RN and Shirley Yen, PhD); New York (Renee Goodwin, PhD, Joshua Lipsitz, PhD and Jessica Page, PsyD); Baltimore (Laura Eisen, BS, Karan Lamb, PsyD, Tracey Lichner, PhD, Yung-mei Leong, PhD and Krista Vermillion, BA); Boston (Dan Geller, MD, Anne Chosak, PhD, Michelle Wedig, BS, Evelyn Stewart, MD, Michael Jenike, MD, Beth Gershuny, PhD and Sabine Wilhelm, PhD); Bethesda (Lucy Jestement, Diane Kazuba, V Holland LaSalle-Ricci and Theresa B DeGuzman); and Los Angeles (R Lindsey Bergman, PhD, Susanna Chang, PhD, Audra Langley, PhD and Amanda Pearlman, BA). In addition, we wish to thank Jason Briggs at ABI for his technical assistance during set-up of the SNPlex assay in a high-throughput, 384-well robotized format, Ming-Chen Chien, MS, at the Columbia University Genome Center, Dave Conti, USC, Keck School, Biostatistics and Dr Jonathan Liu and colleagues, Soft Genetics, Inc. for early design versions of Gene Marker & Mutation Surveyor softwares.
Funding Source: This study is supported by NIMH R01 MH50214 and NIH/NCRR/OPD-GCRC RR00052 (GN). EV is a recipient of a 2006 grant award from the Obsessive Compulsive Foundation (OCF) and a departmental fellowship award (USC, Keck School, Psychiatry). OE received a Young Investigator Award from NARSAD. YYS initiated her contribution to this report while working at JHU, and is currently working at the Genomic Research Branch, NIMH. Part of this work was completed as her outside activity, and as such the views expressed in this article do not necessarily represent the views of the NIMH, NIH, HHS, or the US Government. SAR and DLP are funded by the NIMH. SLR has received honoraria and/or consultation fees from Neurogen, Sepracor, Novartis and Medtronic, and has conducted research funded by Medtronic, Cyberonics, Cephalon and Northstar. JTM has received research support from Eli Lilly, Bristol Myers, Squibb, Seaside Pharmaceuticals, and Aspect. Other relevant NIMH awards: K23-MH066284 (MG) & K23-MH64543 (OJB). JAK is funded by the NIMH, CMREF and NARSAD, and this project was funded by NIMH grants MH079494 & MH050214. He is a member of the scientific advisory boards of SoftGenetics, Inc. & Life Technologies, Inc. and has received compensation from the latter.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Molecular Psychiatry website
Rights and permissions
About this article
Cite this article
Voyiaziakis, E., Evgrafov, O., Li, D. et al. Association of SLC6A4 variants with obsessive-compulsive disorder in a large multicenter US family study. Mol Psychiatry 16, 108–120 (2011). https://doi.org/10.1038/mp.2009.100
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/mp.2009.100
Keywords
This article is cited by
-
Can social support during pregnancy affect maternal DNA methylation? Findings from a cohort of African-Americans
Pediatric Research (2020)
-
Serotonin system gene variants and regional brain volume differences in pediatric OCD
Brain Imaging and Behavior (2020)
-
Appetitive and reactive aggression are differentially associated with the STin2 genetic variant in the serotonin transporter gene
Scientific Reports (2018)
-
Association between serotonin transporter gene polymorphisms and increased suicidal risk among HIV positive patients in Uganda
BMC Genetics (2017)
-
Neurobiology of rodent self-grooming and its value for translational neuroscience
Nature Reviews Neuroscience (2016)