Abstract
Objective:
To determine the reliability of an objective measure of pain, agitation and sedation using the Neonatal Pain, Agitation and Sedation Scale (N-PASS) compared with nursing bedside assessment.
Study Design:
Neonates admitted in neonatal intensive care unit over a 6-month period were eligible. Pain and sedation were assessed with N-PASS, and a subjective questionnaire was administered to the bedside nurse.
Result:
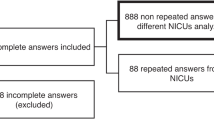
A total of 218 neonates were eligible (median: gestational age 34.6 weeks, age at assessment 7 days). N-PASS pain score correlated significantly with both nurses’ pain score (Spearman coefficient (r)=0.37; P<0.001) and agitation score (r=0.56; P<0.001). N-PASS sedation score correlated with nurses’ sedation score (r=−0.39; P<0.001). Adjusting for gestational age, day of life, intrauterine drug exposure and use of high frequency ventilation only slightly attenuated the correlations (r=0.36, 0.55 and −0.31, respectively).
Conclusion:
The N-PASS captures nursing assessment of pain, agitation and sedation in this broad population and provides a quantitative assessment of subjective descriptions that often drives patient therapy.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Anand KJ . Pharmacological approaches to the management of pain in the neonatal intensive care unit. J Perinatol 2007; 27 (Suppl 1): S4–S11.
Anand KJ . Pain assessment in preterm neonates. Pediatrics 2007; 119: 605–607.
Anand KJ, Aranda JV, Berde CB, Buckman S, Capparelli EV, Carlo W et al. Summary proceedings from the neonatal pain-control group. Pediatrics 2006; 117: S9–S22.
Anand KJ . Consensus statement for the prevention and management of pain in the newborn. Arch Pediatr Adolesc Med 2001; 155: 173–180.
Batton DG, Barrington KJ, Wallman C . Prevention and management of pain in the neonate: an update. Pediatrics 2006; 118: 2231–2241.
Taylor BJ, Robbins JM, Gold JI, Logsdon TR, Bird TM, Anand KJ . Assessing postoperative pain in neonates: a multicenter observational study. Pediatrics 2006; 118: e992–1000.
Hummel P, Puchalski M, Creech SD, Weiss MG . Clinical reliability and validity of the N-PASS: neonatal pain, agitation and sedation scale with prolonged pain. J Perinatol 2008; 28: 55–60.
Hummel P, Lawlor-Klean P, Weiss MG . Validity and reliability of the N-PASS assessment tool with acute pain. J Perinatol 2010; 30: 474–478.
Johansson M, Kokinsky E . The COMFORT behavioural scale and the modified FLACC scale in paediatric intensive care. Nurs Crit Care 2009; 14: 122–130.
Ballantyne M, Stevens B, McAllister M, Dionne K, Jack A . Validation of the premature infant pain profile in the clinical setting. Clin J Pain 1999; 15: 297–303.
Lawrence J, Alcock D, McGrath P, Kay J, MacMurray SB, Dulberg C . The development of a tool to assess neonatal pain. Neonatal Netw 1993; 12: 59–66.
Krechel SW, Bildner J . CRIES: a new neonatal postoperative pain measurement score. Initial testing of validity and reliability. Paediatr Anaesth 1995; 5: 53–61.
Debillon T, Zupan V, Ravault N, Magny JF, Dehan M . Development and initial validation of the EDIN scale, a new tool for assessing prolonged pain in preterm infants. Arch Dis Child Fetal Neonatal Ed 2001; 85: F36–F41.
Stevens B, Johnston C, Taddio A, Gibbins S, Yamada J . The premature infant pain profile: evaluation 13 years after development. Clin J Pain 2010; 26: 813–830.
Pokela ML . Pain relief can reduce hypoxemia in distressed neonates during routine treatment procedures. Pediatrics 1994; 93: 379–383.
Anand KJ, Barton BA, McIntosh N, Lagercrantz H, Pelausa E, Young TE et al. Analgesia and sedation in preterm neonates who require ventilatory support: results from the NOPAIN trial. Neonatal Outcome and Prolonged Analgesia in Neonates. Arch Pediatr Adolesc Med 1999; 153: 331–338.
Anand KJ, Hall RW, Desai N, Shephard B, Bergqvist LL, Young TE et al. Effects of morphine analgesia in ventilated preterm neonates: primary outcomes from the NEOPAIN randomised trial. Lancet 2004; 363: 1673–1682.
Simons SH, van Dijk M, van Lingen RA, Roofthooft D, Duivenvoorden HJ, Jongeneel N et al. Routine morphine infusion in preterm newborns who received ventilatory support: a randomized controlled trial. JAMA 2003; 290: 2419–2427.
Ng E, Taddio A, Ohlsson A . Intravenous midazolam infusion for sedation of infants in the neonatal intensive care unit. Cochrane Database Syst Rev 2000; CD002052.
Hummel P, van Dijk M . Pain assessment: current status and challenges. Semin Fetal Neonatal Med 2006; 11: 237–245.
Johnston CC, Stevens BJ, Franck LS, Jack A, Stremler R, Platt R . Factors explaining lack of response to heel stick in preterm newborns. J Obstet Gynecol Neonatal Nurs 1999; 28: 587–594.
Acknowledgements
We thank the NICU staff nurses at Johns Hopkins Hospital for their cooperation in this research. We also thank Christoph Lehmann, MD, for informatics support and Lauren Jansson, MD, and W Christopher Golden, MD, for their support as members of the B. Hillman’s scholarship oversight committee. Kathryn A Carson’s work on this publication was made possible by the Johns Hopkins Institute for Clinical and Translational Research (ICTR) which is funded in part by Grant Number UL1 TR 000424-06 from the National Center for Advancing Translational Sciences (NCATS), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. The contents are solely the responsibility of the authors and do not necessarily represent the official view of the Johns Hopkins ICTR, NCATS or NIH. None of the authors have financial relationships relevant to this article to disclose.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Hillman, B., Tabrizi, M., Gauda, E. et al. The Neonatal Pain, Agitation and Sedation Scale and the bedside nurse’s assessment of neonates. J Perinatol 35, 128–131 (2015). https://doi.org/10.1038/jp.2014.154
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2014.154
This article is cited by
-
Opioid and benzodiazepine use during therapeutic hypothermia in encephalopathic neonates
Journal of Perinatology (2020)
-
Neonatal Pain, Agitation, and Sedation Scale’s use, reliability, and validity: a systematic review
Journal of Perinatology (2020)