Abstract
Background
There is variability in the use of sedatives and analgesics in neonatal intensive care units (NICUs). We aimed to investigate the use of analgesics and sedatives and the management of neonatal pain and distress.
Methods
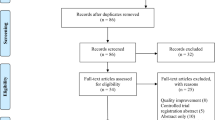
This was a global, prospective, cross-sectional study. A survey was distributed May–November 2022. The primary outcome of this research was to compare results between countries depending on their socio-sanitary level using the sociodemographic index (SDI). We organized results based on geographical location.
Results
The survey collected 1304 responses, but we analyzed 924 responses after database cleaning. Responses from 98 different countries were analyzed. More than 60% of NICUs reported having an analgosedation guideline, and one-third of respondents used neonatal pain scales in more than 80% of neonates. We found differences in the management of sedation and analgesia between NICUs on different continents, but especially between countries with different SDIs. Countries with a higher SDI had greater availability of and adherence to analgosedation guidelines, as well as higher rates of analgosedation for painful or distressing procedures. Countries with different SDIs reported differences in analgosedation for neonatal intubation, invasive ventilation, and therapeutic hypothermia, among others.
Conclusions
Socio-economic status of countries impacts on neonatal analgosedation management.
Impact
-
There is significant variability in the pain management practices in neonates.
-
There is a lack of knowledge related to how neonatal pain management practices differ between regions.
-
Sociodemographic index is a key factor associated with differences in neonatal pain management practices across global regions.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
McPherson, C. & Grunau, R. E. Pharmacologic analgesia and sedation in neonates. Clin. Perinatol. 49, 243–265 (2022).
Carbajal, R. et al. Epidemiology and treatment of painful procedures in neonates in intensive care units. JAMA 300, 60–70 (2008).
McPherson, C., Ortinau, C. M. & Vesoulis, Z. Practical approaches to sedation and analgesia in the newborn. J. Perinatol. 41, 383–395 (2021).
Allegaert, K., Tibboel, D. & van den Anker, J. Pharmacological treatment of neonatal pain: in search of a new equipoise. Semin. Fetal Neonatal Med. 18, 42–47 (2013).
Ten Barge, J. A., Vermeulen, M. J., Simons, S. H. P. & van den Bosch, G. E. Pain management for necrotizing enterocolitis: getting the balance right. Pediatr. Res. 92, 1423–1431 (2022).
Hall, R. W. & Anand, K. J. Pain management in newborns. Clin. Perinatol. 41, 895–924 (2014).
Kinoshita, M., Borges do Nascimento, I. J., Styrmisdottir, L. & Bruschettini, M. Systemic opioid regimens for postoperative pain in neonates. Cochrane Database Syst. Rev. 4, CD015016 (2023).
Kinoshita, M., Olsson, E., Borys, F. & Bruschettini, M. Opioids for procedural pain in neonates. Cochrane Database Syst. Rev. 4, CD015056 (2023).
Bellu, R. et al. Opioids for newborn infants receiving mechanical ventilation. Cochrane Database Syst. Rev. 3, CD013732 (2021).
Romantsik, O., Calevo, M. G., Norman, E. & Bruschettini, M. Clonidine for sedation and analgesia for neonates receiving mechanical ventilation. Cochrane Database Syst. Rev. 5, CD012468 (2017).
Ng, E., Taddio, A. & Ohlsson, A. Intravenous midazolam infusion for sedation of infants in the neonatal intensive care unit. Cochrane Database Syst. Rev. 1, CD002052 (2017).
Agakidou, E. et al. Changes in physicians’ perceptions and practices on neonatal pain management over the past 20 years. A survey conducted at two time-points. Front Pediatr. 9, 667806 (2021).
Wade, C. et al. Development of locally relevant clinical guidelines for procedure-related neonatal analgesic practice in Kenya: a systematic review and meta-analysis. Lancet Child Adolesc. Health 4, 750–760 (2020).
Brindle, M. E. et al. Consensus Guidelines for Perioperative Care in Neonatal Intestinal Surgery: Enhanced Recovery after Surgery (Eras((R))) Society Recommendations. World J. Surg. 44, 2482–2492 (2020).
Carbajal, R. et al. Sedation and analgesia practices in neonatal intensive care units (europain): results from a prospective cohort study. Lancet Respir. Med. 3, 796–812 (2015).
Bansal, A. Comparison of outcome of very-low-birth-weight babies with developed countries: a prospective longitudinal observational study. J. Clin. Neonatol. 7, 254–258 (2018).
Fajolu, I. B. et al. Rates and predictors of mortality of very low birthweight infants in three Nigerian tertiary hospitals. Acta Paediatr. 112, 1766–1773 (2022).
Vain, N., Farina, D. & Vazquez, L. Neonatology in the emerging countries: the strategies and health-economics challenges related to prevention of neonatal and infant infections. Early Hum. Dev. 88, S53–S59 (2012).
Bowe, T. et al. The current state of retinopathy of prematurity in India, Kenya, Mexico, Nigeria, Philippines, Romania, Thailand, and Venezuela. Digital J. Ophthalmol.: DJO 25, 49 (2019).
Gilbert, C. et al. Characteristics of Infants with severe retinopathy of prematurity in countries with low, moderate, and high levels of development: implications for screening programs. Pediatrics 115, e518–e525 (2005).
Kunle-Olowu, O. E., Peterside, O. & Adeyemi, O. O. Prevalence and outcome of preterm admissions at the neonatal unit of a tertiary health centre in Southern Nigeria. Open J. Pediatr. 4, 67–75 (2014).
Network, G. B. o. D. C. Global Burden of Disease Study 2015 (Gbd 2015) Socio-Demographic Index (Sdi) 1980–2015. (Institute for Health Metrics and Evaluation (IHME), Seattle, United States of America, 2016).
Cao, G., Liu, J. & Liu, M. Global, regional, and national incidence and mortality of neonatal preterm birth, 1990-2019. JAMA Pediatr. 176, 787–796 (2022).
Boulkedid, R., Abdoul, H., Loustau, M., Sibony, O. & Alberti, C. Using and reporting the Delphi method for selecting healthcare quality indicators: a systematic review. PLoS ONE 6, e20476 (2011).
Eubank, B. H. et al. Using the modified Delphi method to establish clinical consensus for the diagnosis and treatment of patients with rotator cuff pathology. BMC Med. Res. Methodol. 16, 56 (2016).
WHO. Total Fertility Rate (Per Woman), <https://www.who.int/data/gho/indicator-metadata-registry/imr-details/123> (Consulted June 2023).
Hollestein, L. M. et al. Multiple ways to correct for multiple comparisons in multiple types of studies. Br. J. Dermatol. 185, 1081–1083 (2021).
Daverio, M. et al. Pain and sedation management and monitoring in pediatric intensive care units across europe: an espnic survey. Crit. Care 26, 88 (2022).
Hasson, F., Keeney, S. & McKenna, H. Research guidelines for the Delphi survey technique. J. Adv. Nurs. 32, 1008–1015 (2000).
Network., G. B. o. D. C. Global Burden of Disease Study 2019 (Gbd 2019) Socio-Demographic Index (Sdi) 1950–2019. (Institute for Health Metrics and Evaluation (IHME), Seattle, United States of America, 2020).
Tang, Z. & Jia, J. The association between the burden of Pm(2.5)-related neonatal preterm birth and socio-demographic index from 1990 to 2019: a global burden study. Int J. Environ. Res. Public Health 19, 10068 (2022).
Tang, Z. & Jia, J. Pm(2.5)-related neonatal encephalopathy due to birth asphyxia and trauma: a global burden study from 1990 to 2019. Environ. Sci. Pollut. Res. Int. 30, 33002–33017 (2023).
Zhang, Z., Wang, J., Song, N., Shi, L. & Du, J. The global, regional, and national burden of stomach cancer among adolescents and young adults in 204 countries and territories, 1990-2019: a population-based study. Front. Public Health 11, 1079248 (2023).
Allegaert, K. & Bellieni, C. V. Analgosedation in neonates: what we know and how we act. Research and Reports in Neonatology 3, 51–61 (2013).
Basnet, S., Adhikari, N. & Koirala, J. Challenges in setting up pediatric and neonatal intensive care units in a resource-limited country. Pediatrics 128, e986–e992 (2011).
Diaconu, K. et al. Methods for medical device and equipment procurement and prioritization within low-and middle-income countries: findings of a systematic literature review. Glob. Health 13, 1–16 (2017).
Mirbaha-Hashemi, F. et al. Progress towards every newborn action plan (Enap) implementation in iran: obstacles and bottlenecks. BMC Pregnancy Childbirth 21, 1–10 (2021).
Bapat, R. et al. A multicenter collaborative to improve postoperative pain management in the NICU. Pediatrics 152, e2022059860 (2023).
Franck, L. S. et al. Parent involvement in pain management for NICU infants: a randomized controlled trial. Pediatrics 128, 510–518 (2011).
Avila-Alvarez, A. et al. Clinical assessment of pain in spanish neonatal intensive care units. An. de. Pediatr.ía (Engl. Ed.) 85, 181–188 (2016).
de Melo, G. M., Lelis, A. L., de Moura, A. F., Cardoso, M. V. & da Silva, V. M. Pain assessment scales in newborns: integrative review. Rev. Paul. Pediatr. 32, 395–402 (2014).
Olsson, E. et al. The use and reporting of neonatal pain scales: a systematic review of randomized trials. Pain 162, 353–360 (2021).
Espinosa Fernández, M. G. et al. Sedoanalgesia en las unidades neonatales. An. de. Pediatr.ía 95, 126.e121–126.e111 (2021).
Giordano, V. et al. Pain and sedation scales for neonatal and pediatric patients in a preverbal stage of development: a systematic review. JAMA Pediatr. 173, 1186–1197 (2019).
Akuma, A. O. & Jordan, S. Pain management in neonates: a survey of nurses and doctors. J. Adv. Nurs. 68, 1288–1301 (2012).
Kumar, P. et al. Premedication for nonemergency endotracheal intubation in the neonate. Pediatrics 125, 608–615 (2010).
Wheeler, B., Broadbent, R. & Reith, D. Premedication for neonatal intubation in Australia and New Zealand: a survey of current practice. J. Paediatr. Child Health 48, 997–1000 (2012).
Duan, X., Li, Y., Zhou, C., Huang, L. & Dong, Z. Dexmedetomidine provides neuroprotection: impact on ketamine-induced neuroapoptosis in the developing rat brain. Acta Anaesthesiol. Scand. 58, 1121–1126 (2014).
Wang, Y., Han, R. & Zuo, Z. Dexmedetomidine–induced neuroprotection: is it translational? Transl. Perioper. Pain Med. 1, 15 (2016).
Maier, C., Steinberg, G. K., Sun, G. H., Zhi, G. T. & Maze, M. Neuroprotection by the alpha 2-adrenoreceptor agonist dexmedetomidine in a focal model of cerebral ischemia. Anesthesiology 79, 306–312 (1993).
Mantecon-Fernandez, L., Lareu-Vidal, S., Gonzalez-Lopez, C., Solis-Sanchez, G. & Suarez-Rodriguez, M. Dexmedetomidine: an alternative to pain treatment in neonatology. Child. (Basel) 10, 454 (2023).
Simbruner, G., Mittal, R. A., Rohlmann, F. & Muche, R., neo.n, E. n. T. P. Systemic Hypothermia after neonatal encephalopathy: outcomes of Neo.Neuro.Network Rct. Pediatrics 126, e771–e778 (2010).
Liow, N. et al. Preemptive morphine during therapeutic hypothermia after neonatal encephalopathy: a secondary analysis. Ther. Hypothermia Temp. Manag. 10, 45–52 (2020).
Lally, P. J. et al. Magnetic resonance biomarkers in neonatal encephalopathy (marble): a prospective multicountry study. BMJ Open 5, e008912 (2015).
Lally, P. J. et al. Magnetic resonance spectroscopy assessment of brain injury after moderate hypothermia in neonatal encephalopathy: a prospective multicentre cohort study. Lancet Neurol. 18, 35–45 (2019).
Jimeno Ruiz, S., Riaza Gomez, M., Cardenas Rebollo, J. M. & Lopez-Escobar, A. Material and sedation-analgesia in the neonatal lumbar puncture procedure. An. Pediatr. (Engl. Ed.) 95, 246–252 (2021).
Evans, S. M. et al. Attitudes and barriers to incident reporting: a collaborative hospital study. Qual. Saf. Health Care 15, 39–43 (2006).
Kotaniemi, J. T. et al. Does non-responder bias have a significant effect on the results in a postal questionnaire study? Eur. J. Epidemiol. 17, 809–817 (2001).
Acknowledgements
We would like to thank all neonatal staff who took some time to share their experience responding to this survey. All contributors who shared their email will receive feedback or results. Special thanks to https://99nicu.org/, ESPR (European Society for Pediatric Research), and all pediatric and neonatal societies, who helped with the circulation of the survey.
Funding
This study was (partially) funded by the Italian Ministry of Health—Current Research IRCCS.
Author information
Authors and Affiliations
Consortia
Contributions
Conceptualization: C.A., F.G., E.V., K.A., G.C. Methodology: C.A., F.G., G.C., K.A. Software: F.G., G.C. Validation, K.A., E.V., C.A., G.R. Formal analysis: C.A., F.G., C.L., J.L.G. Investigation: F.G., C.A., G.C., G.R. Resources: F.G., C.A., G.C. Data curation: F.G., C.L., J.L.G., C.L. Writing—original draft preparation: F.G., C.A., J.L.G., G.C. Writing—review and editing, F.G., G.C., G.R., K.A., E.V., A.S., S.S., C.L., J.L.G. Supervision: K.A., E.V. Funding acquisition, F.G., G.C. All authors have read and agreed to the published version of the manuscript. Major revisions edited by: F.G., J.L.G., G.C.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Patients’ consent was not required to perform this study, as confirmed by the Ethics Committee, as patients are not involved. The certificate of this Committee can be downloaded at https://doi.org/10.5061/dryad.1zcrjdfzb.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Arribas, C., Cavallaro, G., Gonzalez, JL. et al. Global cross-sectional survey on neonatal pharmacologic sedation and analgesia practices and pain assessment tools: impact of the sociodemographic index (SDI). Pediatr Res (2024). https://doi.org/10.1038/s41390-024-03032-7
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41390-024-03032-7