Abstract
OBJECTIVE: The goal of this study was to evaluate the effect of two diets (‘food combining’ or dissociated vs balanced) on body weight and metabolic parameters during a 6-week period in an in-hospital setting.
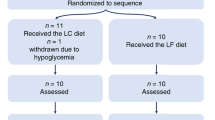
SUBJECTS AND DESIGN: 54 obese patients were randomly assigned to receive diets containing 4.5 MJ/day (1100 kcal/day) composed of either 25% protein, 47% carbohydrates and 25% lipids (dissociated diet) or 25% protein, 42% carbohydrates and 31% lipids (balanced diet). Consequently, the two diets were equally low in energy and substrate content (protein, fat and carbohydrate) but widely differed in substrate distribution throughout the day.
RESULTS: There was no significant difference in the amount of weight loss in response to dissociated (6.2 ± 0.6 kg) or balanced (7.5 ± 0.4 kg) diets. Furthermore, significant decreases in total body fat and waist-to-hip circumference ratio were seen in both groups, and the magnitude of the changes did not vary as a function of the diet composition. Fasting plasma glucose, insulin, total cholesterol and triacylglycerol concentrations decreased significantly and similarly in patients receiving both diets. Both systolic and diastolic blood pressure values decreased significantly in patients eating balanced diets. The results of this study show that both diets achieved similar weight loss. Total fat weight loss was higher in balanced diets, although differences did not reach statistical significance. Total lean body mass was identically spared in both groups.
CONCLUSION: In summary at identical energy intake and similar substrate composition, the dissociated (or ‘food combining’) diet did not bring any additional loss in weight and body fat.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Chan JM, Rimm EB, Colditz GA, Stampfer MJ, Willett WC . Obesity, fat distribution and weight gain as risk factor for clinical diabetes in men Diabetes Care 1994 17: 961–969.
Golay A, Munger R, Felber JP . Obesity and NIDDM: the retrograde regulation concept Diabetes Rev 1997 5 (1):: 69–82.
International Obesity Task Force (IOTF) . Obesity: preventing and managing the global epidemic. Report of a WHO Consultation on Obesity WHO: Geneva.
Kuczmarski RJ . Prevalence of overweight and weight gain in the United States Am J Clin Nutr 1992 55 (Suppl): 495–502.
Kuczmarski RJ, Flegal KM, Campbell SM, Johnson CL . Increasing prevalence of overweight among US adults. The National Health and Nutrition Examination Surveys, 1960 to 1986 Int J Obes 1991 15: 513–521.
Stevens J, Cai J, Pamuk ER, Williamson DF, Thun MJ, Wood JL . The effect of age on the association between body-mass index and mortality N Engl J Med 1998 338: 1–7.
Golay A, Allaz AF, Morel Y, de Tonnac N, Tankova S, Reaven G . Similar weight loss with low- or high-carbohydrate diets Am J Clin Nutr 1996 63: 174–178.
Alford BB, Blankenship AC, Hagen RD . The effects of variations in carbohydrate, protein and fat content of the diet upon weight loss, blood values and nutrient intake of adult obese women J Am Diet Assoc 1990 90: 534–540.
Piatti PM, Pontiroli AE, Saibene A, Santambrogio G, Paroni G, Magni F, Galli-Kienle M, Mistrali S, Monti LD, Pozza G . Insulin sensitivity and lipid levels in obese subjects after slimming diets with different complex and simple carbohydrate content Int J Obes 1993 17: 375–381.
Schlundt DG, Hill JO, Pope-Cordle J, Arnold D, Virts KL, Katahn M . Randomized evaluation of a low fat ad libitum carbohydrate diet for weight reduction Int J Obes 1993 17: 623–629.
Racette SB, Schoeller DA, Kushner RF, Neil KM, Herling-laffaldano K . Effects of aerobic exercise and dietary carbohydrate on energy expenditure and body composition during weight reduction in obese women Am J Clin Nutr 1995 61: 486–494.
Walker KZ, O'Dea K, Nicholson GC, Muir JG . Dietary composition, body weight and NIDDM Diabetes Care 1995 18 (3): 401–403.
Kassirer JP, Angell M . Losing weight—an ill-fated new year's resolution N Engl J Med 1998 338: 52–54.
Kendall A, Levitsky DA, Strupp BJ, Lissner L . Weight loss on a low-fat diet: consequences of the imprecision of the control of food intake in humans Am J Clin Nutr 1991 53: 1124–1129.
Miller WC, Niederpruem MG, Wallace JP, Lindeman AK . Dietary fat, sugar and fiber predict body fat content J Am Diet Assoc 1994 94: 612–615.
Shah M, McGovern P, French S, Baxter J . Comparison of a low-fat, ad libitum complex-carbohydrate diet with a low-energy diet in moderately obese women Am J Clin Nutr 1994 59: 980–984.
Sheppard L, Kristal AR, Kushi LH . Weight loss in women participating in a randomized trial of low-fat diets Am J Clin Nutr 1991 54: 821–828.
Montignac M . Je mange done je maigris! Ou les secrets de la nutrition Ed Artulen: Paris 1991.
Bobbioni-Harsch E, Habicht F, Lehmann T, James RW, Rohner-Jeanrenaud F, Golay A . Energy expenditure and substrates oxidative patterns, after glucose, fat or mixed load in normal weight subjects Eur J Clin Nutr 1997 20: 370–374.
Golay A, Morel Y, Lehmann T, Schutz Y . Fluctuations pondérales et régimes alimentaires Cah. Nutr. Diet. 1994 XXIX (2): 81–84.
Kluthe B . Prodi 3+. Interactive logic for food and nutritional advisers Univeŕsité de Fribourg 1989.
Souci SW, Fachmann W, Kraut H . La composition des aliments. Tableaux des valeurs nutritives 1989/1990 Wissentschaftliche Verlagsgesellschaft 1989.
Renaud S, Attil MC . La composition des aliments Astra-Calve Information lipodiététique, INSERM unité 63: Paris 1986.
Kadish AH, Litle RL, Sternberg JC . A new and rapid method for determination of glucose by measurements of rate of oxygen consumption Clin Chem 1968 14: 116–131.
Herbert V, Lau KS, Gottlieb CW, Bleicher SJ . Coated charcoal immunoassay of insulin J Clin Endocrinol 1965 25: 1375–1384.
Allain CA, Poon LS, Chang ES, Richmond W, Fu PC . Enzymatic determination of total serum cholesterol Clin Chem 1974 20: 470–475.
Wahfeld AW . Triglyceride determination after enzymatic hydrolysis. In Bergmeyer HV (ed) Methods of enzymatic analysis Academic Press: New York 1974 pp 1831–1835.
Hawk PB . Kjeldahl method. In Practical physiological chemistry, 12th edn Blackiston: Toronto 1947 pp 814–822.
Dehaven J, Sherwin R, Hendler R, Felig P . Nitrogen and sodium balance and sympathetic-nervous-system activity in obese subjects treated with a low-calorie protein or mixed diet N Engl J Med 1980 302: 477–482.
Segal KR, Van Loan M, Fitzgerald PI, Hogdon JA, Van Itallie TB . Lean body mass estimation by bioelectrical impedance analysis: a four-site cross-validation study Am J Clin Nutr 1988 47: 7–14.
Acknowledgements
We are grateful to the members of the Dietary staff of the Department of Medicine for their assistance, in particular to P Rigoli, C Bussien and J Duffey.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Golay, A., Allaz, AF., Ybarra, J. et al. Similar weight loss with low-energy food combining or balanced diets. Int J Obes 24, 492–496 (2000). https://doi.org/10.1038/sj.ijo.0801185
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ijo.0801185
Keywords
This article is cited by
-
Development and preliminary validity of an Indonesian mobile application for a balanced and sustainable diet for obesity management
BMC Public Health (2022)
-
Eating carbohydrate mostly at lunch and protein mostly at dinner within a covert hypocaloric diet influences morning glucose homeostasis in overweight/obese men
European Journal of Nutrition (2014)