Abstract
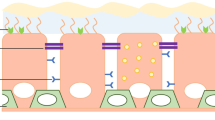
An efficient adeno-associated virus (AAV) vector was constructed for the treatment of respiratory diseases. AAV serotypes, promoters and routes of administration potentially influencing the efficiency of gene transfer to airway cells were examined in the present study. Among the nine AAV serotypes (AAV1–9) screened in vitro and four serotypes (AAV1, 2, 6, 9) evaluated in vivo, AAV6 showed the strongest transgene expression. As for promoters, the cytomegalovirus (CMV) early enhancer/chicken β-actin (CAG) promoter resulted in more robust transduction than the CMV promoter. Regarding delivery routes, intratracheal administration resulted in strong transgene expression in the lung, whereas the intravenous and intranasal administration routes yielded negligible expression. The combination of the AAV6 capsid and CAG promoter resulted in sustained expression, and the intratracheally administered AAV6-CAG vector transduced bronchial cells and pericytes in the lung. These results suggest that AAV6-CAG vectors are more promising than the previously preferred AAV2 vectors for airway transduction, particularly when administered into the trachea. The present study offers an optimized strategy for AAV-mediated gene therapy for lung diseases, such as cystic fibrosis and pulmonary fibrosis.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Cystic Fibrosis Foundation. Cystic Fibrosis Foundation Patient Registry 2014 Annual Data Report; 2015 [Bethesda, MD, USA].
Bjoraker JA, Ryu JH, Edwin MK, Myers JL, Tazelaar HD, Schroeder DR et al. Prognostic significance of histopathologic subsets in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 1998; 157: 199–203.
Riordan JR, Rommens JM, Kerem B, Alon N, Rozmahel R, Grzelczak Z et al. Identification of the cystic fibrosis gene: cloning and characterization of complementary DNA. Science 1989; 245: 1066–1073.
Seibold MA, Wise AL, Speer MC, Steele MP, Brown KK, Loyd JE et al. A common MUC5B promoter polymorphism and pulmonary fibrosis. N Engl J Med 2011; 364: 1503–1512.
Mueller C, Flotte TR . Clinical gene therapy using recombinant adeno-associated virus vectors. Gene Ther 2008; 15: 858–863.
Asokan A, Schaffer DV, Samulski RJ . The AAV vector toolkit: poised at the clinical crossroads. Mol Ther 2012; 20: 699–708.
Nathwani AC, Reiss UM, Tuddenham EG, Rosales C, Chowdary P, McIntosh J et al. Long-term safety and efficacy of factor IX gene therapy in hemophilia B. N Engl J Med 2014; 371: 1994–2004.
Muramatsu S, Fujimoto K, Kato S, Mizukami H, Asari S, Ikeguchi K et al. A phase I study of aromatic L-amino acid decarboxylase gene therapy for Parkinson's disease. Mol Ther 2010; 18: 1731–1735.
LeWitt PA, Rezai AR, Leehey MA, Ojemann SG, Flaherty AW, Eskandar EN et al. AAV2-GAD gene therapy for advanced Parkinson's disease: a double-blind, sham-surgery controlled, randomized trial. Lancet Neurol 2011; 10: 309–319.
Ashtari M, Cyckowski LL, Monroe JF, Marshall KA, Chung DC, Auricchio A et al. The human visual cortex responds to gene therapy-mediated recovery of retinal function. J Clin Invest 2011; 121: 2160–2168.
Testa F, Maguire AM, Rossi S, Pierce EA, Melillo P, Marshall K et al. Three-year follow-up after unilateral subretinal delivery of adeno-associated virus in patients with Leber congenital Amaurosis type 2. Ophthalmology 2013; 120: 1283–1291.
Aitken ML, Moss RB, Waltz DA, Dovey ME, Tonelli MR, McNamara SC et al. A phase I study of aerosolized administration of tgAAVCF to cystic fibrosis subjects with mild lung disease. Hum Gene Ther 2001; 12: 1907–1916.
Moss RB, Rodman D, Spencer LT, Aitken ML, Zeitlin PL, Waltz D et al. Repeated adeno-associated virus serotype 2 aerosol-mediated cystic fibrosis transmembrane regulator gene transfer to the lungs of patients with cystic fibrosis: a multicenter, double-blind, placebo-controlled trial. Chest 2004; 125: 509–521.
Moss RB, Milla C, Colombo J, Accurso F, Zeitlin PL, Clancy JP et al. Repeated aerosolized AAV-CFTR for treatment of cystic fibrosis: a randomized placebo-controlled phase 2B trial. Hum Gene Ther 2007; 18: 726–732.
Halbert CL, Allen JM, Miller AD . Adeno-associated virus type 6 (AAV6) vectors mediate efficient transduction of airway epithelial cells in mouse lungs compared to that of AAV2 vectors. J Virol 2001; 75: 6615–6624.
Gao G, Vandenberghe LH, Alvira MR, Lu Y, Calcedo R, Zhou X et al. Clades of adeno-associated viruses are widely disseminated in human tissues. J Virol 2004; 78: 6381–6388.
Virella-Lowell I, Zusman B, Foust K, Loiler S, Conlon T, Song S et al. Enhancing rAAV vector expression in the lung. J Gene Med 2005; 7: 842–850.
Limberis MP, Vandenberghe LH, Zhang L, Pickles RJ, Wilson JM . Transduction efficiencies of novel AAV vectors in mouse airway epithelium in vivo and human ciliated airway epithelium in vitro. Mol Ther 2009; 17: 294–301.
Flotte TR, Fischer AC, Goetzmann J, Mueller C, Cebotaru L, Yan Z et al. Dual reporter comparative indexing of rAAV pseudotyped vectors in chimpanzee airway. Mol Ther 2010; 18: 594–600.
Song S, Morgan M, Ellis T, Poirier A, Chesnut K, Wang J et al. Sustained secretion of human alpha-1-antitrypsin from murine muscle transduced with adeno-associated virus vectors. Proc Natl Acad Sci USA 1998; 95: 14384–14388.
Sirninger J, Muller C, Braag S, Tang Q, Yue H, Detrisac C et al. Functional characterization of a recombinant adeno-associated virus 5-pseudotyped cystic fibrosis transmembrane conductance regulator vector. Hum Gene Ther 2004; 15: 832–841.
Niwa H, Yamamura K, Miyazaki J . Efficient selection for high-expression transfectants with a novel eukaryotic vector. Gene 1991; 108: 193–199.
Halbert CL, Lam SL, Miller AD . High-efficiency promoter-dependent transduction by adeno-associated virus type 6 vectors in mouse lung. Hum Gene Ther 2007; 18: 344–354.
Duan D, Yue Y, Yan Z, McCray PB Jr, Engelhardt JF . Polarity influences the efficiency of recombinant adenoassociated virus infection in differentiated airway epithelia. Hum Gene Ther 1998; 9: 2761–2776.
Yan Z, Lei-Butters DC, Liu X, Zhang Y, Zhang L, Luo M et al. Unique biologic properties of recombinant AAV1 transduction in polarized human airway epithelia. J Biol Chem 2006; 281: 29684–29692.
Gruntman AM, Mueller C, Flotte TR, Gao G . Gene transfer in the lung using recombinant adeno-associated virus. Curr Protoc Microbiol 2012; Chapter 14: Unit 14D.2.
Wu Z, Miller E, Agbandje-McKenna M, Samulski RJ . α2,3 and α2,6N-linked sialic acids facilitate efficient binding and transduction by adeno-associated virus types 1 and 6. J Virol 2006; 80: 9093–9103.
Ng R, Govindasamy L, Gurda BL, McKenna R, Kozyreva OG, Samulski RJ et al. Structural characterization of the dual glycan binding adeno-associated virus serotype 6. J Virol 2010; 84: 12945–12957.
Thompson CI, Barclay WS, Zambon MC, Pickles RJ . Infection of human airway epithelium by human and avian strains of influenza a virus. J Virol 2006; 80: 8060–8068.
Favaro P, Finn JD, Siner JI, Wright JF, High KA, Arruda VR . Safety of liver gene transfer following peripheral intravascular delivery of adeno-associated virus (AAV)-5 and AAV-6 in a large animal model. Hum Gene Ther 2011; 22: 843–852.
Damdindorj L, Karnan S, Ota A, Hossain E, Konishi Y, Hosokawa Y et al. A comparative analysis of constitutive promoters located in adeno-associated viral vectors. PLoS One 2014; 9: e106472.
Chen BD, He CH, Chen XC, Pan S, Liu F, Ma X et al. Targeting transgene to the heart and liver with AAV9 by different promoters. Clin Exp Pharmacol Physiol 2015; 42: 1108–1117.
Gray SJ, Foti SB, Schwartz JW, Bachaboina L, Taylor-Blake B, Coleman J et al. Optimizing promoters for recombinant adeno-associated virus-mediated gene expression in the peripheral and central nervous system using self-complementary vectors. Hum Gene Ther 2011; 22: 1143–1153.
Ostedgaard LS, Rokhlina T, Karp PH, Lashmit P, Afione S, Schmidt M et al. A shortened adeno-associated virus expression cassette for CFTR gene transfer to cystic fibrosis airway epithelia. Proc Natl Acad Sci USA 2005; 102: 2952–2957.
Fischer AC, Smith CI, Cebotaru L, Zhang X, Askin FB, Wright J et al. Expression of a truncated cystic fibrosis transmembrane conductance regulator with an AAV5-pseudotyped vector in primates. Mol Ther 2007; 15: 756–763.
Mueller C, Torrez D, Braag S, Martino A, Clarke T, Campbell-Thompson M et al. Partial correction of the CFTR-dependent ABPA mouse model with recombinant adeno-associated virus gene transfer of truncated CFTR gene. J Gene Med 2008; 10: 51–60.
Yin L, Greenberg K, Hunter JJ, Dalkara D, Kolstad KD, Masella BD et al. Intravitreal injection of AAV2 transduces macaque inner retina. Invest Ophthalmol Vis Sci 2011; 52: 2775–2783.
Duan D, Yue Y, Engelhardt JF . Expanding AAV packaging capacity with trans-splicing or overlapping vectors: a quantitative comparison. Mol Ther 2001; 4: 383–391.
Song Y, Lou HH, Boyer JL, Limberis MP, Vandenberghe LH, Hackett NR et al. Functional cystic fibrosis transmembrane conductance regulator expression in cystic fibrosis airway epithelial cells by AAV6.2-mediated segmental trans-splicing. Hum Gene Ther 2009; 20: 267–281.
Hirsch ML, Li C, Bellon I, Yin C, Chavala S, Pryadkina M et al. Oversized AAV transductifon is mediated via a DNA-PKcs-independent, Rad51C-dependent repair pathway. Mol Ther 2013; 21: 2205–2216.
Liqun Wang R, McLaughlin T, Cossette T, Tang Q, Foust K, Campbell-Thompson M et al. Recombinant AAV serotype and capsid mutant comparison for pulmonary gene transfer of alpha-1-antitrypsin using invasive and noninvasive delivery. Mol Ther 2009; 17: 81–87.
Daya S, Berns KI . Gene therapy using adeno-associated virus vectors. Clin Microbiol Rev 2008; 21: 583–593.
Boutin S, Monteilhet V, Veron P, Leborgne C, Benveniste O, Montus MF et al. Prevalence of serum IgG and neutralizing factors against adeno-associated virus (AAV) types 1, 2, 5, 6, 8, and 9 in the healthy population: implications for gene therapy using AAV vectors. Hum Gene Ther 2010; 21: 704–712.
Vidović D, Gijsbers R, Quiles Jimenez A, Dooley J, Van den Haute C, Van der Perren A et al. Noninvasive imaging reveals stable transgene expression in mouse airways after delivery of a nonintegrating recombinant adeno-associated viral vector. Hum Gene Ther 2016; 27: 60–71.
Halbert CL, Rutledge EA, Allen JM, Russell DW, Miller AD . Repeat transduction in the mouse lung by using adeno-associated virus vectors with different serotypes. J Virol 2000; 74: 1524–1532.
Manning WC, Zhou S, Bland MP, Escobedo JA, Dwarki V . Transient immunosuppression allows transgene expression following readministration of adeno-associated viral vectors. Hum Gene Ther 1998; 9: 477–485.
Calcedo R, Wilson JM . Humoral immune response to AAV. Front Immunol 2013; 4: 341.
Armulik A, Genové G, Betsholtz C . Pericytes: developmental, physiological, and pathological perspectives, problems, and promises. Dev Cell 2011; 21: 193–215.
Dickie R, Wang YT, Butler JP, Schulz H, Tsuda A . Distribution and quantity of contractile tissue in postnatal development of rat alveolar interstitium. Anat Rec (Hoboken) 2008; 291: 83–93.
Di Pasquale G, Chiorini JA . AAV transcytosis through barrier epithelia and endothelium. Mol Ther 2006; 13: 506–516.
Patton JS . Mechanisms of macromolecule absorption by the lungs. Adv Drug Deliv Rev 1996; 19: 3–36.
Hung C, Linn G, Chow YH, Kobayashi A, Mittelsteadt K, Altemeier WA et al. Role of lung pericytes and resident fibroblasts in the pathogenesis of pulmonary fibrosis. Am J Respir Crit Care Med 2013; 188: 820–830.
Hutchison N, Fligny C, Duffield JS . Resident mesenchymal cells and fibrosis. Biochim Biophys Acta 2013; 1832: 962–971.
Ogura M, Urabe M, Akimoto T, Onishi A, Ito C, Ito T et al. Interleukin-10 expression induced by adeno-associated virus vector suppresses proteinuria in Zucker obese rats. Gene Ther 2012; 19: 476–482.
Mochizuki S, Mizukami H, Kume A, Muramatsu S, Takeuchi K, Matsushita T et al. Adeno-associated virus (AAV) vector-mediated liver- and muscle-directed transgene expression using various kinds of promoters and serotypes. Gene Ther Mol Biol 2004; 8: 9–18.
Muramatsu S, Mizukami H, Young NS, Brown KE . Nucleotide sequencing and generation of an infectious clone of adeno-associated virus 3. Virology 1996; 221: 208–217.
Chiorini JA, Yang L, Liu Y, Safer B, Kotin RM . Cloning of adeno-associated virus type 4 (AAV4) and generation of recombinant AAV4 particles. J Virol 1997; 71: 6823–6833.
Chiorini JA, Kim F, Yang L, Kotin RM . Cloning and characterization of adeno-associated virus type 5. J Virol 1999; 73: 1309–1319.
Rutledge EA, Halbert CL, Russell DW . Infectious clones and vectors derived from adeno-associated virus (AAV) serotypes other than AAV type 2. J Virol 1998; 72: 309–319.
Gao GP, Alvira MR, Wang L, Calcedo R, Johnston J, Wilson JM . Novel adeno-associated viruses from rhesus monkeys as vectors for human gene therapy. Proc Natl Acad Sci USA 2002; 99: 11854–11859.
Lock M, McGorray S, Auricchio A, Ayuso E, Beecham EJ, Blouin-Tavel V et al. Characterization of a recombinant adeno-associated virus type 2 reference standard material. Hum Gene Ther 2010; 21: 1273–1285.
Ayuso E, Blouin V, Lock M, McGorray S, Leon X, Alvira MR et al. Manufacturing and characterization of a recombinant adeno-associated virus type 8 reference standard material. Hum Gene Ther 2014; 25: 977–987.
Marques TEBS, de Mendonça LR, Pereira MG, de Andrade TG, Garcia-Cairasco N, Paçó-Larson ML et al. Validation of suitable reference genes for expression studies in different pilocarpine-induced models of mesial temporal lobe epilepsy. PLoS One 2013; 8: e71892.
Acknowledgements
We thank Miyoko Mitsu, Satomi Fujiwara and Tomonori Tsukahara for their technical assistance; and Dr Ryoko Saito (Tohoku University) for thoughtful advice and suggestions. This work was supported by a Jichi Medical University Graduate Student Start-up Grant for Young Investigators to FK in 2015. This study was also supported by the Research Program on HIV/AIDS and the Practical Research Project for Rare/Intractable Diseases from the Japan Agency for Medical Research and Development.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on Gene Therapy website
Rights and permissions
About this article
Cite this article
Kurosaki, F., Uchibori, R., Mato, N. et al. Optimization of adeno-associated virus vector-mediated gene transfer to the respiratory tract. Gene Ther 24, 290–297 (2017). https://doi.org/10.1038/gt.2017.19
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/gt.2017.19
This article is cited by
-
GITRL on dendritic cells aggravates house dust mite-induced airway inflammation and airway hyperresponsiveness by modulating CD4+ T cell differentiation
Respiratory Research (2021)
-
Tissue and cell-type-specific transduction using rAAV vectors in lung diseases
Journal of Molecular Medicine (2021)