Abstract
As the availability of genetic tests has grown rapidly during the last decade along with the increasing knowledge of the genetic background of rare inherited diseases, sending DNA samples to another country for analysis has become more of a routine than an exception in clinical diagnostics. Nonetheless, few studies of cross-border genetic testing of rare diseases in the European Union (EU) have been carried out, and data about the challenges and problems related to cross-border testing are lacking. The purpose of this study was to investigate the experiences of the molecular genetic laboratories and the clinical genetics units concerning the cross-border genetic testing of rare diseases in the Member States of the EU. Data were collected using web-based questionnaires and phone interviews targeted at laboratories and clinical units registered with the Orphanet database. The specific aims were to clarify the volume, quality and challenges of cross-border genetic testing. The results revealed, for example, that the variability of the required documentation creates confusion and, unexpectedly, sample dispatch was considered a major problem in cross-border testing. In addition, the differences between countries regarding the reimbursement and authorization policies of cross-border testing were significant, thus confirming the pre-existing assumption about unequal access to genetic testing in the different Member States. To facilitate and organize cross-border testing, common practices need to be created at the level of the EU, and follow-up studies are needed to monitor their effects.
Similar content being viewed by others
Introduction
In the European Union (EU), a disease is considered rare if it affects fewer than 5 people per 10 000. On the basis of this, it has been estimated that there are approximately 5000–8000 rare diseases (RD)1 and that between 27 and 36 million people are affected in the EU alone. Around 80% of all RD are considered to be genetic in origin. The rarity of a condition creates an unequal situation in health care: patients with a common disease, such as diabetes, have well-developed health services with experienced personnel all over Europe. At the same time, patients with rare conditions find it difficult to get appropriate services or to find their way to an expert, leading to frequent delay in receiving the correct diagnosis and difficulties in accessing counselling, treatment, and reimbursement.
In an analysis based on the data from Orphanet in 2012, the number and scope of tests for genetically caused RD varies immensely between the Member States (MS), and the number of appropriate laboratories is not proportional to the size of the population.2 The type of testing available also varies widely between MS, with large MS, such as Germany, offering tests for 1880 genes at that time, whereas small MS, such as Latvia, offered tests for only 10 genes. In some countries, it is possible to routinely purchase tests from abroad, while in others financial and authorization procedures complicate purchasing tests. To create yet further inequality, even though in some MS it is possible to purchase tests from private sector laboratories, the cost of these tests is not refunded by the state. Currently, the only RD for which at least some testing is offered in 30 out of the 34 European countries represented in the Orphanet is cystic fibrosis. Moreover, 871 RD were tested in 1 country only, and 2285 diseases tested in 5 countries or fewer.3 In many cases, the developing technology will make it more practical and economical to use test panels instead of testing single genes, but thus far these are available in even fewer countries than single gene analyses.3
In this context, and given the large number of genetic disorders and the need to design and validate a specific set of diagnostic assays for each, no single country can be self-sufficient in providing the molecular genetic testing needed, and it is evident that cross-border testing has become a routine procedure. The previous figures reflecting the volume of cross-border testing in the EU are from the OECD 2005 report on quality assurance in genetic testing4 and from the more recent study by Berwouts et al5 on the quality assurance of European molecular genetic testing laboratories,5 where two-thirds of the studied laboratories had received samples from outside the country and half of laboratories had referred samples to laboratories in other countries. More importantly, while the data on the volume of cross-border testing are rather old or indirect, the possible challenges and problems encountered relating to such testing have not been studied at all. Thus, the purpose of this study was to investigate the experiences of the laboratories and the genetics clinics on the process of cross-border genetic testing for RD in the MS of the EU. The specific areas of interest in the study were as follows: (1) the actual number of samples crossing borders, (2) the reasons for purchasing tests abroad, (3) the factors influencing cross-border testing in different MS, and (4) the testing laboratories’ and counselling clinics’ experiences with the process. The final part of the research sought suggestions for overcoming the problems identified in this study, particularly those leading to unequal access to genetic testing.
Materials and methods
This research was conducted as a survey aimed at genetic testing laboratories and genetic counselling clinics in all of the 28 MS of the EU, and all those laboratories and clinics registered with the Orphanet database of rare diseases (www.orpha.net). The survey included questionnaires and phone interviews for both groups (Supplementary Information). The questionnaires consisted of 43 questions for laboratories and 41 questions for clinics (Supplementary Information A and B). The questions were divided into sections concerning the sample flow, different quality and financial aspects of testing, and national plans for RD. In addition, respondents were asked to highlight the major problems of cross-border testing and to give their opinions and suggestions on how these problems should be addressed at the level of the Union. Of these questions, 18 were the same in both questionnaires; these concerned issues relating to quality, financing, and national plans. The questionnaires included single choice, multiple choice, and open questions; the latter served as a basis for the phone interviews, which mainly concentrated on the major problems of testing and their solutions. The questionnaires were pre-evaluated, in collaboration with EuroGentest,6 by the heads of two major academic testing laboratories, one private testing laboratory, and one counselling clinic from different MS.
The questionnaires were formulated using the Webropol online survey and analysis tool (www.webropol.fi). The invitations and reminders to participate in the survey were sent by the Orphanet technical department. The questionnaire data were collected between 7 January and 4 March 2014, and the reminders to participate were sent 7 and 14 days after the first invitation. In addition, an invitation to participate was posted on the EuroGentest public website 19 days after the first invitation. The phone interviews were performed over the period 3–14 February 2014; five respondents from the laboratory survey and four respondents from the clinic survey were interviewed by phone. The interviewees represented large and small MS, as well as a range of States in different economic situations. The interviews were recorded and transcribed to paper, and then analysed by theme.
The results of the questionnaire were analysed by focusing on the empirical knowledge of the respondents. Both complete and partial responses were accepted, resulting in a difference in the number of responses to different questions. When estimating the sample flow, the laboratories were asked to give the estimated or true number of total, sent, and received samples in 2013. To estimate the number of samples sent abroad from the clinics, they were asked to choose either the scale or give the true number of outgoing samples in 2013.
Results
Respondents
In total, 173 responses were received from 1573 molecular genetic laboratories that were contacted (11%). Of those, 170 were eligible responses. The reasons for rejecting responses were that they came from a non-EU country or some other type of testing than genetic testing was performed. In the laboratory group, responses were received from all MS except for Lithuania, Luxembourg, and Slovenia (Table 1). In all, 77 respondents were from public, 43 from academic, 25 from research and 19 from private laboratories. Five respondents belonged to the group ‘Other’, consisting of laboratories that were both public and academic, or academic and research laboratories. For the questionnaire sent to 605 genetic counselling clinics, 105 responses (17%) were received in total. The respondents were most active in the United Kingdom, Italy, and Spain, whereas no responses were received from four countries (Estonia, Greece, Hungary, and Luxembourg, Table 1).
Sample flow
In the respondent’s laboratories, the estimated total number of genetests for RD in 2013 was 265 361, with a mean of 1561 samples per laboratory and a median of 335 samples (Table 2). The same estimated numbers for sent and received samples are presented in Table 2, and the sample flow based on laboratory type is presented in Table 3. Based on the number of the laboratories that the questionnaire was sent (1573), an estimation of the total number of RD samples tested in Europe in 2013 was ~2.5 million.
When looking at the volume of sent and received samples by laboratory, 59% of the laboratories sent and received 1–20 samples, 22 laboratories (24%) sent over 100 samples abroad, and 16 laboratories (17%) received more than 100 samples last year. Of all laboratories, 8 laboratories sent and received more than 100 samples per year. Of the laboratories, 59% reported having sent samples to other EU countries, and 66% had received samples from other EU countries in 2013. On the basis of the number of sent samples, it was estimated that approximately ~100 000 samples crossed borders between the MS in 2013. Typically, clinics sent 10–20 samples abroad in 2013 (38%), and 19% sent more than 50 samples out, the highest number being nearly 1500 samples, although this was exceptional among the respondents. Most commonly the percentage of outgoing tests in clinics was between 1 and 10% of all tested samples.
Laboratories (n=155, multiple choice question) most often offer cross-border testing of RD due to scientific interest (n=110, Table 4). The second reason was the offering of testing on a courtesy basis (n=66), and the third reason was the profitable nature of testing (n=30). According to the respondents, from the clinical point of view the sending of the samples abroad was possible in all MS except Romania, and 83% of the respondents were able to send the samples to any EU country they desired (n=101). If the test to be ordered was also available in the respondent’s home country, 53% were not allowed to order the test from abroad (n=99). When all of the respondents (n=243, multiple choice question) were asked, by far the most common reason for sending samples abroad was because the requested test was not performed in the respondent’s country (n=196). The second reason was financial – in some cases cross-border testing was more affordable than local testing (n=43). A faster turnaround time (n=17) or better quality (n=16) was more marginal reason for sending samples abroad.
Quality issues
Laboratories
For the majority of the laboratory respondents (71%), language was not an issue in cross-border testing (n=159). When asked to evaluate whether there was a difference in the quality of the referrals and samples between the MS (n=94), 80% did not observe any significant differences. Comprehension of the content of the requested tests was more of a problem (n=152), as 11% responded that clients often misunderstood the test content, and a further 11% sometimes misunderstood the content. When the samples were sent from another country to the laboratories as blood, they arrived the testing laboratory in good condition according to 51% of the respondents, whereas according to 4% the quality of the samples was often compromised. In addition to the normal diagnostic samples, cross-border travel for urgent samples is fairly frequent, as 36% reported receiving samples that needed urgent testing, for example fetal diagnostic samples (n=157).
When predictive testing was performed in a given laboratory (n=149), 69% of the respondents always knew based on the referral that the test was predictive, but 3% reported that there was often uncertainty about the nature of the test. If the test to be performed was predictive (n=127), then 35% of the laboratories reported that they were informed beforehand that the person to be tested had received pre-test counselling, and 24% of the laboratories had sent an enquiry to the customer, but the remaining 11% of the laboratories were not informed nor had they enquired into the situation regarding counselling before performing the test.
Counselling clinics
For most of the clinicians (88%), finding the testing laboratory was not challenging (n=98). Many of the clinicians left the sending of the sample to the local laboratory, but when sending samples themselves, the most common way of protecting patient privacy was to code the samples (14/53). Experiences concerning the informed consent practices of foreign laboratories were variable: 32% of the respondents never used a different consent process but their own, whereas 31% at least sometimes used the consent form required by the foreign laboratory, and 5% always. Also, experience of laboratories requesting an informed consent as a prerequisite for testing varied largely: 15% of the respondents stated that the laboratory had always requested the consent, but 16% had never had such requests. Furthermore, 21% had to deliver the consent often, 29% sometimes, and 20% only rarely. If the tests performed were urgent, such as prenatal tests, 40% of the respondents had always received the results in time and a further 55% often (n=75). In all, 27% of the respondents reported urgent tests failing rarely, and only 1% had experiences of tests failing often. For 19% of the respondents, the interpretation of the results from foreign laboratories was sometimes challenging, and 2% had constant problems in doing so (n=95). In general, ~80% of the respondents considered the results of the cross-border tests reliable, but 7% reported rarely or never relying on the results.
Shared quality questions
Of the information sources for finding the laboratory (n=246, multiple choice question), Orphanet was most commonly used (n=161) followed by the Genetests webpage (n=103). In addition, recommendation by colleagues (n=92) and reputation of the laboratories (n=76) had an important role in the selection of the laboratory, as did PubMed (n=73). Other means of finding the laboratory were, for example, long-term collaboration and the EDDNAL website. Contacting the laboratory of interest was unproblematic in general, as 76% of the respondents (n=225) reported that communication was always or often easy. Ordering the test from the home country was easier than from abroad for 63% of the respondents (n=176), and for 15% there were no differences, but interestingly, 13% responded that the ordering of a test from the home country was more difficult than from abroad.
When asking for the criteria for selecting a testing laboratory (multiple choice question, n=244), the quality status of the laboratory was the first criterion (n=183). It was closely followed by the price (n=148) and the reputation of the laboratory (n=124), but a faster turnaround time (n=82) or the country of the laboratory (n=33) seem to have played a more minor role in the decision-making. The proven quality status of the laboratory (n=238) was always used as a criterion in the search by 34%, and often by 33%, of the respondents, but with 10% of the respondents it was never used as a criterion. If the respondents were to choose between accredited academic or private laboratories (n=233), 36% of the respondents were uncertain which one to choose, but of the remaining respondents 58% would choose an academic laboratory over a private one. The use of broker companies does not seem to be common among the respondents, as 98% (n=231) replied that they prefer to send the sample directly to the chosen laboratory. The results of tests were most often returned by e-mail or as hard copy through the post (n=195). However, in half of the cases where the results were returned by e-mail, unprotected e-mail was used. The results were returned within the promised turnaround time in ~75% of the cases (n=214).
Financial issues
Laboratories received requests for tests free of charge fairly often, as only one-fourth (26%) had never had such requests (n=161). Twenty-five percent of the laboratories had received feedback from customers that the tests were too expensive (n=134). A different billing or rating system for RD samples received from abroad was used in 21% of the laboratories (n=137). The collection of payments of performed tests was challenging, as over half of the respondents (54%) had at least sometimes encountered difficulties in collecting payment from customers abroad (n=134).
The laboratories had experience of different ways to cover the costs of cross-border testing. Many laboratories had faced a situation where the expenses were in general covered by the health-care system (n=100), but in many instances the patient was to pay for the testing (n=53). The insurance companies were responsible for paying more rarely (n=26), and research grants were also used to cover for the costs of cross-border testing (n=153, multiple choice question). Cross-border testing seems to have both positive and negative effects on local testing services, as the income from the cross-border tests may help laboratories to maintain their expertise in certain RD, but at the same time, samples are sent abroad even if they could be tested locally.
Shared financial questions
When the respondents were asked to compare the costs of the testing abroad versus their home country, the responses were scattered (n=229). In the opinion of 29%, the price level varied depending on the country, 26% responded that the prices were much the same, 36% responded that the prices were higher abroad, and the remaining 8% felt that the prices were lower elsewhere. Opinions about the rational organization of the funding of RD testing also diverged (n=207): 36% were satisfied with the current system while 46% wished for changes. The funding policies of cross-border testing were variable between the countries (n=200): 25% responded that the tests were paid for without any restrictions or need to provide justification, 39% responded that there were either restrictions or preapprovals needed, 17% said that tests were not reimbursed, and 20% were unaware of whether reimbursement was available. In addition, 69% said that no specific funding stream existed for cross-border RD testing, and in countries where such a stream was said to exist, it was often considered insufficient to meet the demand and need for testing abroad (n=203).
Major problems
Concerning the laboratories, the major problems of cross-border testing were related to the different financial aspects of the testing (open-field question, n=170, Table 4). The costs of the tests, payment, and reimbursement issues were mentioned in one-third of the responses. Of the other problems, sending the samples across borders often caused concern in the laboratories (24/170), aroused issues regarding the quality of testing (18/170) and also increased the related bureaucracy (12/170). Other individual problems mentioned included, for example, a lack of knowledge of RD among the health-care authorities and a lack of reference centres and networking between laboratories.
Upon asking from the clinical respondents how they define the major problems (n=105), three aspects that received the most comments were the high costs of the testing (23/105), variable funding (16/105), and the quality of the testing laboratories (16/105). In addition, the lack of information concerning finding a laboratory for the test was sometimes mentioned (13/105). Administrative problems, difficulties in sample sending, and the lack of specific cross-border testing strategy in the EU were also mentioned as being among the major problems.
Discussion
The field of RD has gained increasing attention in the course of recent years as a result of the deep influence of, for example, the patient organizations, genetic societies, individual researchers and clinicians and, ultimately, initiatives from the European Commission. Such initiatives are, for instance, the adoption of the Commission Communication on Rare Diseases,1 the Regulation of Orphan Medicinal Products,7 and the Council Recommendation on an action in the field of Rare Diseases,8 the taking effect of the Directive on cross-border health care,9 the decision to establish the European Reference Networks (ERNs),9 and the assignment of the European Union Committee of Experts on Rare Diseases (EUCERD) (The Commission decision on establishing the (EUCERD) European Commission Decision of 30 November 2009 (2009/872/EC)) and later the Commission Expert Group on Rare Diseases (http://ec.europa.eu/health/rare_diseases/expert_group/index_en.htm). As knowledge of the specific genes and mutations behind the classical RD phenotypes has increased, the diseases have been split into new aetiologically distinct entities. The exact genetic diagnosis has growing importance because the genetic diagnosis has implications for the life of the patients and their families. In addition, new specific treatments are being developed and their optimal use demands an exact diagnosis. Consequently, the need for exact diagnosis based on a gene test has increased, itself leading to an increased demand in cross-border testing. This study aimed at exploring the possible difficulties in the processes of genetic testing in another country with the eventual intention of presenting these difficulties to the national and EU authorities in the hope of finding efficient solutions to them.
Although we aimed our survey at all MS through the comprehensive list of genetic laboratories and clinical genetic units listed on Orphanet, a response was received from only 11 and 17% of these, respectively. In addition, from several countries only one or very few laboratories and clinics responded (Table 1). It may well be that those laboratories and clinics that replied to our survey were biased in one or several ways. As the survey questionnaires were sent by Orphanet, there may be an overrepresentation of respondents who have had positive experiences regarding collaboration with Orphanet. In general, those with considerable experience of cross-border testing may have been more active, as may possibly have been those with the biggest problems. Another issue was that some MS were very active in responding while others were not; for instance, one-third of the responses from the clinical genetics units came from the United Kingdom, possibly skewing the results related to the situation in that MS or its health-care system. In some countries, the data were based on the opinion of a single respondent, also possibly skewing the results for the analysis. In spite of these problems, we believe that the survey gave a multi-faceted view on the many issues relating to cross-border testing in Europe today. The results cannot be regarded as an exact image of cross-border testing in EU but rather taken as qualitative results documenting the different aspects of the cross-border genetic testing practices.
The results corroborated the initial assumption of EU citizens having unequal access to genetic testing, but the extent of the inequality was unexpected. In some countries (see below) wide restrictions for testing, both locally and cross-border, are in use, leaving most of the patients without genetic diagnosis, when in other countries all testing is possible either in the country itself or through purchase from abroad without restrictions. The other unexpected result was the lack of any shared practices for cross-border testing, especially in terms of financial and authorization issues, leading to the fact that each country is applying its own rules for cross-border testing. Of the more specific issues, it was unexpected that the process of sending a sample abroad was ranked among the major problems according to both laboratories and clinics.
The respondents reported that Orphanet was primarily used when searching for a testing laboratory; nonetheless, the web interface of Orphanet received some criticism as not being particularly user-friendly. The respondents were frustrated with pages not being updated often enough and the feature that in order to find the information about the tests, one has to go to the laboratory’s home page, which may be closed, only in the native language or otherwise deficient. In particular, finding the prices was felt to be challenging. The respondents suggested a clear, simple interface listing the laboratories testing for RD with the possibility of direct contact, a uniform way of presenting the type and coverage of the test, the price and accreditation status. At the time of writing this article, Orphanet was in its latest phases of development of a new web interface for searching laboratories and tests (Ana Rath, personal communication).
Countries with specific situations
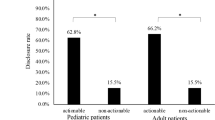
According to the survey, the citizens in the different MS have unequal access to genetic testing, both within the countries and abroad, and the responses also provided an insight into the downside of the genetic testing situation in certain countries. In the following, we describe the situation in the countries which, at the time of the survey, had major problems in availability of genetic testing. In Croatia, the genetic testing of RD is offered to all children if it is expected to have an impact on the treatment and outcome of the disease but to adult patients only if they have additional insurance. In Latvia, persons older than 18 years cannot be tested due to reimbursement issues and children only if the disease to be tested is fatal or very severe. In Poland, the authorization process for cross-border testing in practice cuts off all testing abroad, as the process is very exhaustive and time-consuming. In addition, the cutoff price for tests is very low, allowing only a few types of tests. In Romania, the patient is to pay for the testing, meaning that most of the patients cannot cover the costs and are left without a molecular diagnosis. Interestingly, when the Romanian clinicians were asked if they are allowed to send samples abroad, they response was negative, but the Romanian laboratories reported having sent samples abroad for testing. As a comparison, for example in Finland and Sweden, where a fairly large number of tests are sent abroad annually, all tests considered necessary by the clinicians are paid for by the public health care regardless of cost. Of note, all of the above-mentioned facts are based on the opinions of the individual respondents or interviewees and may not entirely reflect the situation in the specific countries.
Common practical problems
One issue raising several comments was the variability of the forms used for cross-border testing. The referrals, consent forms, documents needed for sending the sample abroad, and result reports are at present variable even between different laboratories in one MS but yet more so between different countries, and this creates extra work and confusion. As the documentation issue is partly related to the issue of accreditation, many of the respondents were hoping that the accreditation according to ISO15189 would become compulsory for those laboratories offering cross-border testing. However, in the case of ultra-RD, the accreditation requirement may exclude some of the diseases due to the low number of patients. These comments raised the question of whether there should be a general EU guideline on the information and documents needed if cross-border testing is offered, as well as on the level of quality control assurance.
Issues related to the sending of the samples were often commented upon by both groups. The current regulation concerning the transportation of biological material was considered to complicate the sending, and the costs of sending were also considered high. According to one respondent, the difficulties in sample sending made it necessary to refer the patients, whenever possible, abroad. In cases of urgent samples, the use of logistic companies increases the costs even further. There seems to be a demand for a review and possibly a revision of the European and national regulations for sending biological samples.
In both laboratories and clinics, the major problems were related to the financial aspects of testing. First, the variable pricing of the testing was felt to be problematic. Although there were no clear signs of the cross-border samples travelling to countries with lower testing prices, some countries have set the cutoff price for cross-border testing at a level that may direct the flow towards cheaper laboratories. The challenging economic situation prevailing in Europe may also drive the authorities to reduce the amount of money used in cross-border testing and, hence, force the selection towards cheaper laboratories/countries, as was reported, for example, from Lithuania. It remains to be discussed whether the subventions that are claimed to exist in some countries (according to some of the respondents) should be removed or whether other means to render the pricing more fair for both laboratories and clients should be developed. Second, in many countries the lack of reimbursement was one of the major problems, prohibiting test purchase from abroad even in cases where the clinical utility of the test is well defined.
Third, as the costs of the cross-border testing are paid by different bodies varying between and within countries, laboratories saw the collection of payments as one of the major problems in their cross-border work. The actual payer was often difficult to identify, and even if the payer was known, discussions regarding payment were sometimes lengthy and invoices still remained unpaid. One issue of note was that some of the laboratories have started to collect the payments upfront, while others have ceased to collect payments altogether, as the related work load is not proportional to the payment itself. How the payment procedure should be organized remains to be discussed; the respondents of the survey had no solutions to offer.
The considerable differences between countries with different economic situations raise the question of whether there should be financial support at the EU level for those countries less well off (for example, Bulgaria, Romania, and Latvia). On the basis of the individual comments, the general problem in these countries is the lack or minimal amount of reimbursement for testing by the state, both within the countries and internationally, which leaves most of the patients without both genetic diagnosis and treatment, even if available. The cost of genome-wide NGS-based testing makes the situation yet more challenging: at present the price for such testing is high, and, for instance, exome sequencing is totally inaccessible to patients from countries with low cutoff prices, or when the patients are to pay for the test themselves. A solution to be discussed might be organizing the testing resources in a more collaborative way, which could lead to a growing number of diagnoses and increasing expertise for laboratories in the testing of specific diseases. This would be in line with the objectives of the Commission based on the Council recommendation from 2009 that states that ‘gathering expertise at European level is therefore paramount in order to ensure equal access to accurate information, appropriate and timely diagnosis, and high quality care for RD patients.8
The next-generation sequencing-based testing will become a major issue in cross-border testing in the upcoming years, and it remains to be seen whether the number of samples crossing borders will rise or decline when the costs of the method and instrumentation become more affordable even for smaller laboratories. Another issue will likely be that, as the guidelines and recommendations are currently developing, the quality and content of testing may vary from laboratory to laboratory, and for the customers it may be difficult to compare the results and interpretation. The open questions include whether it would be best to have the run and variant analysis performed in the same or different laboratories and what the role of possible pan-European centres would be in relation to national expertise.
Finally, to our knowledge, at present there is no official compilation of statistics on cross-border testing data at the EU level. For the future, the collection of data on a regular basis could help to assess cross-border testing trends, including its costs, at the level of the Union. Such collection could also reveal gaps and sectors needing further improvement since this study predicts that the inequalities between the MS will most probably increase alongside the growing number of specific treatments being developed.
In November 2015, the Commission Expert Group on Rare Diseases has adopted a set of Recommendations on Cross-Border Genetic Testing of Rare Diseases based on this study (http://ec.europa.eu/health/rare_diseases/docs/2015_recommendation_crossbordergenetictesting_en.pdf). The Policy Recommendations espouse the fundamental principles of transparency, accessibility, collaboration, and competence in the process of cross-border genetic testing for RD.
In conclusion, this study revealed challenges related to cross-border genetic testing of RD that have not been studied before. To solve these issues and to rationalize the cross-border testing, there is a need for collaboration and combining resources between the Commission, the MS, testing laboratories, clinical units, and patient organizations. In addition, further studies are needed to evaluate the outcome of the implemented acts.
References
Communication from the Commission to the European Parliament, the Council, the European Economic and Social Committee and the Committee of the Regions on ‘Rare Diseases: Europe’s Challenge’. Available from http://ec.europa.eu/health/ph_threats/non_com/docs/rare_com_en.pdf.
Ayme S, Gribaldo L, Matthijs G et al: JRC Scientific and Policy Reports: European Workshop on Genetic Testing Offer in Europe. European Commission Joint Research Centre. Luxembourg: Publications Office of the European Union, 2013.
Aymé S, Rodwell C (eds). Report on the State of the Art of Rare Disease Activities in Europe—2014 Edition (Part 1: Overview of Rare Disease Activities in Europe). Available from http://www.eucerd.eu/upload/file/Reports/2014ReportStateofArtRDActivities.pdf.
OECD Quality Assurance and Proficiency Testing for Molecular Genetic Testing: Summary Report of a Survey of 18 OECD Member Countries, Paris 2005 OECD.
Berwouts S, Fanning K, Morris MA, Barton DE, Dequeker E : Quality assurance practices in Europe: a survey of molecular genetic testing laboratories. Eur J Hum Genet 2012; 11: 1118–1126.
Cassiman JJ : Research network: EuroGentest—a European Network of Excellence aimed at harmonizing genetic testing services. Eur J Hum Genet 2005; 10: 1103–1105.
Regulation (EC) No 141/2000 of the European Parliament and of the Council of 16 December 1999 on Orphan Medicinal Products. Available from http://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=OJ:L:2000:018:0001:0005:en:PDF.
Council Recommendation on an Action in the Field of Rare Diseases, 8 June 2009. Available from http://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=OJ:C:2009:151:0007:0010:EN:PDF.
Directive 2011/24/EU on Patients’ Rights in Cross-Border Healthcare. Available from http://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=OJ:L:2011:088:0045:0065:EN:PDF.
Acknowledgements
We would like to thank Ana Rath, Mark Hanauer, and the Orphanet technical team for technical assistance, Gert Matthijs, Katherine Bushby, Karin Writzl, Tero-Pekka Alastalo, and Bert Bakker for reviewing the questions, all interviewees for their participation, and Victoria Hedley for sharing her expertise. The study was part of the EUCERD Joint Action (EJA) and was included in Work Package 8, which focuses on the integration of rare disease initiatives across disease-specific and national areas. This work was financed by the EUCERD Joint Action: Working for Rare Diseases N° 2011 22 01.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on European Journal of Human Genetics website
Supplementary information
Rights and permissions
About this article
Cite this article
Pohjola, P., Hedley, V., Bushby, K. et al. Challenges raised by cross-border testing of rare diseases in the European union. Eur J Hum Genet 24, 1547–1552 (2016). https://doi.org/10.1038/ejhg.2016.70
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejhg.2016.70
This article is cited by
-
Clinical genetics in transition—a comparison of genetic services in Estonia, Finland, and the Netherlands
Journal of Community Genetics (2021)