Abstract
No consensus exists whether women at increased risk for trisomy 21, 13, and 18 should be offered stand-alone rapid aneuploidy detection (RAD) or karyotyping. In this paper, the ethical implications of a fast, relatively cheap and targeted RAD are examined. The advantages of RAD seem less robust than its proponents suggest. Fast test results only give a short-term psychological benefit. The cost advantage of RAD is apparent, but must be weighed against consequences like missed abnormalities, which are evaluated differently by professionals and pregnant women. Since pre-test information about RAD will have to include telling women about karyotyping as a possible alternative, the advantage of RAD in terms of the quantity of information that needs to be given may also be smaller than suggested. We conclude that none of the supposed arguments in favour of RAD is decisive in itself. Whether the case for RAD may still be regarded as convincing when taking these arguments together seems to depend on one's implicit view of what prenatal screening is about. Are we basically dealing with a test for trisomy 21 and a few conditions more? Or are there good grounds for also testing for the wider range of abnormalities that karyotyping can detect? As professionals and pregnant women may have different views about this, we suggest that the best approach is to offer women a choice between RAD and karyotyping. This approach is most in line with the general aim of prenatal screening: providing opportunities for autonomous reproductive choice.
Similar content being viewed by others
INTRODUCTION
Prenatal screening strategies for chromosomal abnormalities consist of two steps.1, 2 First, a risk assessment for the most common trisomies (21 and generally also 13 and 18) is carried out. This is based on a combination of maternal serum testing and fetal nuchal translucency measurement.3 Second, a diagnostic test is offered to women found to be at an increased risk of having a child with one of those trisomies. The diagnosis (usually karyotyping) is performed on fetal material obtained through either chorionic villus sampling (CVS; at 11–14 weeks’ gestation) or amniocentesis (at 15–18 weeks’ gestation). These are invasive tests that hold a small but significant risk (0.3–1.0%) of iatrogenic miscarriage.4, 5 Karyotyping has been the gold standard for prenatal diagnostic testing for nearly half a century. It has a high reliability in diagnosing numeric chromosome aberrations, as well as (major) structural abnormalities. These include unbalanced translocations, balanced translocations (familial and de novo), mosaicism, supernumerary chromosomes, triploidy, and sex chromosome abnormalities. Down's syndrome (trisomy 21) is the most common aneuploidy causing intellectual and developmental disability.6 Other chromosomal abnormalities are less frequent and highly variable. Some of those are lethal (eg, trisomy 13 and trisomy 18), others are asymptomatic, relatively mild (eg, XXY (Klinefelter's syndrome), XXX, XYY), or are of uncertain clinical significance.7, 8
Karyotyping is a labour intensive and thus a rather expensive technique, which takes an average time of 14 days before the test results can be reported. As karyotyping reveals all chromosomal abnormalities that can be microscopically detected, it may lead to other findings than the aneuploidies targeted in prenatal screening. Among those ‘incidental’ (or with a misnomer: ‘unexpected’) findings, there can be severe but also mild abnormalities or abnormalities of which the impact on the health of the child is unsure.7, 9, 10, 11 The development of techniques for rapid aneuploidy detection (RAD) allows cheaper and rapid diagnosis of some selected chromosomal anomalies. A ‘narrow’ RAD targets the chromosomes 21, 13, and 18, whereas a ‘broad’ RAD also includes the sex chromosomes. This development has led to an increased discussion as to whether a full karyotype is always indicated. RAD has already been introduced in several countries, but the question whether and if so, how, RAD should be offered is still under debate.7, 8, 11, 12, 13, 14 Four prenatal diagnostic test options for women at increased risk can be distinguished: karyotyping as stand-alone; RAD with subsequent karyotyping;15, 16 offering women a choice between RAD and karyotyping14, 17, 18 and a stand-alone RAD. Because a stand-alone RAD has been recommended by the UK National Screening Committee and several individual commentators,11, 19, 20 the discussion in this paper focuses on this approach. We will do so by exploring the main arguments in favour of RAD as stand-alone that can be found in the literature: (a) RAD detects the most important abnormalities; (b) RAD enables fast test results and reduces anxiety; (c) RAD is cheaper than karyotyping; (d) the limited scope of RAD simplifies pre-test counselling and enables adequate informed consent; (e) RAD produces only clear test results and eases post-test counselling and decision-making; and (f) RAD guarantees a consistent scope of testing throughout the screening strategy. Although these arguments may appear to be only ‘technical’, they actually are morally charged arguments as well. Therefore, an ethical reflection is needed. The insights gained will be of use to professionals and policymakers in deciding what prenatal diagnostic test offer is to be preferred in the screening context.
NORMATIVE FRAMEWORK FOR PRENATAL SCREENING
To clarify the perspective of our reflection, we first briefly address the normative framework for prenatal screening. This framework is based on the four central principles of health-care ethics. First, the principle of respect for autonomy not only requires that the woman concerned should give her adequate informed consent for screening but is also at the basis of the classical account of the aim of prenatal screening. There is a strong consensus, at least in Western countries, that prenatal screening for fetal abnormalities should have the purpose of facilitating autonomous reproductive choice for pregnant women and their partners.20, 21 The alternative aim of maximising the prevention of the birth of children with congenital abnormalities is regarded as morally problematic for two reasons. It not only sends the implied message that persons with the relevant handicaps are not welcome in society, but it may also lead to pressure upon pregnant women to undergo screening and decide to abort in the case of a fetal abnormality. That would run counter to the principle of autonomy.
Second, the twin principles of beneficence and non-maleficence require that the benefits to pregnant women from participating should clearly outweigh the disadvantages that all screening programmes do have. Finally, the principle of justice requires equality of access and cost-effective use of financial means, especially when programmes are collectively or publicly funded.4, 22, 23
ARGUMENTS IN FAVOUR OF RAD AS STAND-ALONE: AN EVALUATION
RAD detects the most important abnormalities
The debate about RAD and karyotyping is very much about the scope of prenatal testing. Although both diagnostic tests are offered as a follow-up to screening for a fairly limited set of abnormalities, RAD leads to narrowing the range of possible findings as compared with karyotyping. In the debate about this, karyotyping is often presented as the obvious reference point, meaning that the onus of justification rests with those arguing in favour of more limited testing.24 The incidence of clinically relevant abnormalities missed by RAD is estimated to be 1:1000–1:1659, whereas missed abnormalities of mild or uncertain clinical significance are more frequent.7, 14, 19 Proponents of RAD estimate these residual risks to be of limited relevance.25, 26 This is however not obvious, because both the quantity and quality (or seriousness) of chromosomal abnormalities missed by RAD can be evaluated differently. A difference in appreciation already manifests itself in the decision to offer either a ‘broad’ or a ‘narrow’ RAD, which respectively identifies or misses the X and Y chromosomes. The clinical significance of sex chromosomal abnormalities is not always clear and may vary from a relatively mild to an asymptomatic phenotype. An example is XYY, which has been associated with intellectual and behavioural problems but does often not actually lead to any problems at all. To avoid complex pre-test counselling about the possible outcome of findings of limited or uncertain clinical significance and to spare women difficult decisions based on such findings, some professionals want to avoid detecting sex chromosomal abnormalities. Others find it important not to miss them, just to offer parents maximum information and maximum autonomy.27
Both a broad and a narrow RAD miss clinically relevant and unclear autosomal abnormalities that karyotyping does identify. A recent study including 24 prenatal experts suggests that professionals largely prefer to detect abnormalities with severe consequences and would rather not detect chromosomal abnormalities without clinical consequences.28 Dissensus exists with regard to abnormalities with mild or uncertain outcomes. Interestingly, neither RAD nor karyotyping corresponds with these wishes of professionals, because RAD covers only some of the more severe abnormalities, while karyotyping also detects abnormalities without clinical consequences.28 Proponents of RAD seem to value the fact that it misses abnormalities as ‘acceptable, in view of their limited or uncertain clinical relevance’,25 whereas proponents of karyotyping favour access to these findings because they have potential (ranging from uncertain to major) clinical significance.7 Pregnant women themselves have different attitudes towards these findings as well. This is shown by their preference for either RAD or karyotyping12, 14, 29 and by the different reproductive choices they make in case of test results with uncertain clinical significance: most decide to continue with the pregnancy, but some decide for abortion.7 Different views have been found in the general public and between countries as well.30, 31 In short, no consensus exists about the relevance of the abnormalities missed by RAD.
A preference for a narrow RAD, a broad RAD, or karyotyping reflects various views on what delineation of the scope of diagnostic testing is most in line with facilitating autonomous reproductive choice as the aim of prenatal screening.
Fast test results
A second reason to prefer RAD is that it generates test results within 1–4 days. This is considerably faster than karyotyping, which takes ≥14 days in Europe, although results can be ready as early as from 7 days in the United States.8 This reduced waiting time for RAD is clearly advantageous, if it diminishes anxiety for women.19, 31, 32 Still, three qualifying remarks need to be made.
First, the striking contrast between the speed of karyotyping in the United States and Europe in itself bears moral relevance. The difference between fast (7 days) and slow (21 days) karyotyping is 2 weeks. This substantial difference raises the question whether RAD is the only way to shorten the lengthy waiting period that is indeed hard to justify in view of maternal anxiety, the time left for decision making, and the emotional burden of (later) termination of the pregnancy. Furthermore, the difference between fast karyotyping (7 days) and a slow RAD (4 days) is only 3 days, which diminishes the advantage of reduced maternal anxiety that a choice for RAD would entail. The absence of a substantial extra waiting time for more comprehensive information may also motivate women to choose a broad test instead of a narrow test.29
Second, in the face of the existing rather large difference in reporting time between karyotyping and RAD, the consequences of a fast or slow test result should be accounted for. Waiting for test results of karyotyping can place a significant emotional burden on women and their partners,26, 31 but studies also suggest that RAD has no overall psychological benefit compared with karyotyping despite reduced anxiety and stress in the short term.33, 34 Moreover, a recent study, including 103 pregnant women considering amniocentesis, suggests that anxiety and length of waiting time have some effect on women's preferences, but that the clinical consequences of detected abnormalities appear to have the greatest influence on the test that these women would choose.12
Third, part of the clinically relevant abnormalities missed by RAD will be found by the routine ultrasound scan that most pregnant women undergo in the second trimester.35, 36 If so, test results will be delayed by 2–10 weeks, compared with, respectively, a late amniocentesis and an early CVS. This leaves little time for the emotionally burdening decision about continuing or terminating the pregnancy, as abortion is legally prohibited after 20–24 weeks of gestation in many countries. In case of adverse findings that could have been detected earlier, it will be difficult for professionals to explain that they chose a rapid but limited test for the sake of the woman's well-being. Restricting and postponing autonomous choice for this reason is clearly paternalistic. Besides, there is an inconsistency in saying that findings not detected by RAD are of limited value while at the same time presenting the later ultrasound scan as a safety net where at least part of the missed abnormalities will still be found.
To conclude, the ability to produce test results within only a few days counts in favour of RAD, but this advantage is not unchallenged and does not seem to provide a decisive reason to offer a stand-alone RAD.
Financial costs
In the third place, RAD is favoured because it is relatively cheap to perform. Expenses per trisomy 21 case detected (‘detection/cost’ ratio) are less for RAD when compared with karyotyping.31, 37 Furthermore, a recent study suggests that both short- and long-term costs, including incremental cost for a live-born child having a chromosomal abnormality missed by a broad RAD, are lower for a stand-alone RAD than for standard karyotyping.12 According to the same study, allowing women a choice between karyotyping and RAD reduces costs compared with standard karyotyping. If confirmed in further research, these data would seem to suggest that, from a purely economic perspective, a stand-alone RAD is the preferred diagnostic test. Of course, financial considerations are relevant in the ethical assessment of what test to offer. It is a requirement of distributive justice that publicly or collectively funded programmes for prenatal screening should be cost-effective. But that does not amount to saying that the least costly option is always the best choice. Even though it should be acknowledged that budgetary constraints may in practice limit the range of alternative tests available, the challenge is indeed to offer the test that best serves the aim of prenatal screening, while being proportional in the sense that the costs involved can be justified from a health-care economic point of view.
Pre-test counselling: informed consent
Proponents of RAD assert that the limited amount of abnormalities targeted by RAD ensures that prospective parents can be better informed about the test and that adequate informed consent can be obtained more easily. To inform prospective parents about karyotyping is more complicated, because this test may also generate a much wider range of findings, including abnormalities of which the clinical significance is limited or unclear.11, 38 A real concern is indeed that an offer of karyotyping is not always preceded by adequate counselling and informed consent and may therefore lead to outcomes that are ‘unexpected’. Not, of course, for the professional, but for the woman and her partner who were not informed beforehand about the possibility of such outcomes. RAD would avoid this. Still, ‘easy’ pre-test counselling for RAD may be challenged by two factors.
First, a narrow RAD includes the chromosomes 21, 13, and 18, and a broad RAD the chromosomes X and Y as well. This means that proper counselling and informed consent for RAD can still not be limited to Down's syndrome, but will also have to include the differences between trisomies 21, 13, and 18 and the sex chromosomal abnormalities. In order to enable deliberate choices based on sufficient and relevant information and consistent with the decision maker's values,39 pre-test counselling requires an adequate amount of information, adjusted to the patient's knowledge and capabilities.40 In the context of RAD, a distinction can be made between three categories of abnormalities: (1) lethal conditions (trisomies 13 and 18); (2) serious conditions implying lifelong intensive (medical) aid (Down's syndrome); and (3) conditions implying hardly any infirmities (most sex chromosomal abnormalities). A narrow RAD may detect abnormalities of categories (1) and (2), whereas a broad RAD will also find category (3) abnormalities. Karyotyping can detect the same categories of abnormalities, but will also lead to (4) abnormal findings of which the clinical implications are unknown. Given this overlap in types of abnormalities possibly detected by RAD and karyotyping, the pre-test counselling advantage of RAD may be limited, at least where a broad RAD is concerned.
Second, it is reasonable to assume that at least some pregnant women are well acquainted with karyotyping, which has for decades been the accepted diagnostic test. To prevent that women agree to a test on the basis of false assumptions, information about the more limited scope of RAD as compared with karyotyping should be available. An important aspect of women's decision making that will also have to be addressed is their views about whether the narrow focus of RAD provides sufficient justification for undergoing risky invasive testing.41, 42 Because RAD thus requires more extensive counselling than generally accounted for by its proponents, the pre-test counselling advantage of RAD compared with karytoyping may be less than is often assumed.
The different views on RAD suggest an underlying controversy on the interpretation of reproductive autonomy and on how pregnant women's autonomy could best be served. Should the emphasis be on optimising and easing the process of decision making for them, or on maximising the amount of information and reproductive options that they will be provided with? With regard to decision making, a pro-RAD assumption would be that information related to karyotyping is too complicated. However, research among pregnant women has shown that they differ in their preference for either a limited or more extensive amount of information.38, 43 The challenge will be to adapt the information accordingly, while ensuring it is not too much but yet enough information to facilitate adequate informed consent. To restrain information and to limit choices, based on evaluations by professionals, may indeed make counselling more easy, but these evaluations do not necessarily correspond with those of future parents themselves.
From a moral point of view, the question is which approach is most in line with the principles underlying the normative framework. On the one hand, it can be argued that restricting the scope of diagnostic testing violates the principle of respect for autonomy and falls short of the requirement of beneficence. On the other hand, respect for autonomy need not mean that pregnant women should be provided with as much information about the fetus as possible, as that might have the adverse effect of undermining rather than furthering their ability of making autonomous choices and perhaps even lead to harming the women in question. Indeed, more choice is not necessarily better than less. But the question here is about restricting the scope of testing prior to any evidence that women would otherwise be burdened with information that they cannot handle. Pregnant women are found to have different information needs regarding the health of the fetus and also tend to evaluate the features of RAD differently.12, 14 It is therefore not evident that the balance of benefits and burdens is more favourable in case of a stand-alone RAD as compared with karyotyping.
Post-test counselling: burden of choice and anxiety
Another contended advantage is that by avoiding findings of limited and unclear clinical significance, RAD does not confront prospective parents with difficult and unwanted reproductive choices.25, 38 Some professionals are especially uneasy about reporting unclear or mild abnormalities, because of the dilemmas stemming from it.7 Where test results are ambivalent or uncertain, prospective parents will have to decide whether to terminate a wanted pregnancy while the chances of having a healthy child are quite large, or to continue the pregnancy with the implication of continued worries even until after the child's birth, through its childhood or further. Therefore, some conclude that generating these findings is not always in the best interest of the woman or the couple.11, 44
However, pregnant women also show interest in findings with clinically mild consequences and in practice some choose to terminate a pregnancy in case of unclear or mild findings, as they cannot accept the uncertainty of the clinical outcome.7, 12 Although the possibility of an ‘unnecessary abortion’ is a burdening prospect for both professionals and pregnant women, the potential benefit of information about the fetus possibly being affected should be accounted for as well. Clearly, decisions regarding testing and termination of pregnancy should explicitly be left to pregnant women's own views and values in order to respect their autonomous reproductive decision making.
The argument that RAD avoids difficult decisions with regard to terminating or continuing the pregnancy, does not apply to a broad RAD, which also includes X and Y. To target these abnormalities undermines this purpose and supposed advantage of RAD, because most of the sex chromosomal abnormalities are associated with a relatively mild or asymptomatic phenotype, thus being exactly the findings that RAD intends to avoid.
The logic of the prenatal screening strategy
In prenatal screening strategies, a positive risk assessment for trisomy 21 (13 and 18) generally functions as the ‘gateway’ to subsequent diagnostic testing. Because RAD targets these same abnormalities, the screening strategy itself remains consistent in scope throughout its subsequent steps. For this reason, RAD is argued to be the most adequate diagnostic test: test what you screen for. However, to really avoid any breach in this ‘logic of the screening strategy’, RAD should only target those abnormalities for which screening is offered in the first place. If pregnant women are offered prenatal screening for trisomies 21, 13, and 18, the thrust of the argument would be that subsequent testing should not also include X and Y.13 Or, for that matter, RAD should only include trisomy 21 if women are offered screening for Down's syndrome only.
An as yet overlooked consequence of standard karyotyping is that it implies unequal access to diagnostic testing. Pregnant women at an increased risk for trisomies 21, 13, and 18 are given the possibility of having the fetus tested for a range of other abnormalities as well, whereas testing for those ‘further’ abnormalities is unavailable for other pregnant women.
Are we to conclude that in order to end this inequality, justice requires a choice between either offering a narrow RAD to the increased risk group, or offering karyotyping to all pregnant women (as is the case in the United States)?16 Not necessarily. Although the inequality in access may be unfortunate, it is not unfair. Both RAD and karyotyping are performed on fetal material obtained by risky invasive procedures, although this may change within the years to come as soon as non-invasive prenatal diagnostic techniques become widely available.45, 46
Until then the miscarriage risk adhered to current invasive procedures has to be reckoned with, which raises the issue of proportionality. Central to this assessment is the detection/miscarriage ratio. Since women in the group with an increased risk for the few conditions screened for will already be offered invasive testing for RAD, this ratio will become more favourable for them if karyotyping is performed. This ratio will a priori be less favourable for pregnant women without an increased risk for those conditions. Furthermore, the principles of non-maleficence and respect for autonomy are at stake when women are denied the possibility of getting additional information from fetal material obtained through a procedure with a miscarriage risk.13, 47 For this reason, some argue in favour of further expanding the range of abnormalities to be included in diagnostic testing offered to those having CVS or amniocentesis in the context of prenatal screening, for example, by including relatively common heritable diseases like cystic fibrosis and hemoglobinopathies.11 However, the problem of unequal access will make itself even more clearly felt when such a broader test is offered only to those with a positive test for a limited number of chromosomal abnormalities.
Although unequal access to the ‘surplus’ findings of karyotyping may not be a decisive reason to offer a stand-alone RAD, it does constitute a moral reason to reconsider current access to karyotyping.
CONCLUSION
There is no consensus whether women at increased risk for trisomy 21 (13 and 18) should be offered RAD or karyotyping. RAD has some advantageous features: it is fast, relatively cheap, and produces clear test results. Assessment of these aspects, however, shows that the advantages ascribed to RAD are not conclusive. Fast test results have a short term but not an overall psychological benefit over later results. Therefore, the time gain is of minor importance when weighing a fast but limited test (RAD) against a slower but more extensive test (karyotyping). The relevance of abnormalities missed by RAD are evaluated differently between and among professionals and women, and the counselling advantages due to the targeted scope of RAD in the pre-test and post-test situation are relative. RAD is cheaper than karyotyping, but this cannot settle the issue.
We conclude that, from a moral point of view, the case for RAD is less strong than it may at first seem. It is not immediately obvious that RAD is more in line with the requirement of respect for autonomy than karyotyping. Nor is it clear that the balance of advantages and disadvantages is more favourable for the women concerned in the case of RAD. Neither does the fact that women with a prior risk for common aneuploidies are offered wider testing to which others have no access amount to a serious injustice. However, even if a separate assessment of the alleged advantages of RAD does not show any of them to be decisive, it can still be asked whether their cumulative effect might not decide the argument in favour of RAD. The answer to this will depend mainly on what one thinks the scope of prenatal screening and testing should be. The moral framework of prenatal screening itself is not decisive in this regard. For those who think that testing for trisomy 21 or perhaps for common aneuploidies is what prenatal screening is really about, the arguments for limiting the test offer to a narrow or broader RAD may sound convincing. However, others may find that there are good grounds for wanting prenatal screening to at least include the wider range of conditions that karyotyping might detect. Given that there is no objective perspective from whence to decide between these views, leaving the choice to the women concerned would at least have the benefit of being in line with the general aim of offering opportunities for autonomous reproductive choice.
This approach would also have the more practical advantage of being open towards future debates that are most likely about broadening rather than limiting the scope of prenatal screening. The dynamics of the field points in the opposite direction from that proposed by those arguing for RAD. New techniques that can identify an even broader scope of heterogeneous abnormalities than karyotyping are already on the horizon.48, 49 Broader diagnostic testing may even become possible on cell-free fetal DNA that is present in the plasma of pregnant women.45 Apart from the advantage of allowing testing early in pregnancy and without the miscarriage risk adhered to current invasive techniques, the possibility of broad non-invasive diagnostic testing raises further ethical issues.50 Without wanting to pre-empt the debate about whether these developments should lead to further broadening the scope of prenatal screening, we suggest that offering RAD as a stand-alone sends the wrong message. Is protecting pregnant women from difficult choices the best way of preparing for the challenges ahead? Instead of assuming that anything beyond RAD is too difficult for them, it may be better to invest in finding approaches to counselling and informed consent that are adjusted to broader kinds of testing without compromising central moral principles.
References
Boyd P, Devigan C, Khoshnood B et al: Survey of prenatal screening policies in Europe for structural malformations and chromosome anomalies, and their impact on detection and termination rates for neural tube defects and Down's syndrome. BJOG 2008; 115: 689–696.
Tapon D : Prenatal testing for Down syndrome: comparison of screening practices in the UK and USA. J Genet Couns 2010; 19: 112–130.
Saller DN, Canick JA : Current methods of prenatal screening for down syndrome and other fetal abnormalities. Clin Obstetr Gynecol 2008; 51: 24–36.
Health Council of the Netherlands: Prenatal Screening. Down's syndrome, neural tube defects, routine-ultrasonography. Publication no. 2001/11. The Hague, Health Council of the Netherlands, 2001, available at: http://www.gezondheidsraad.nl/en/publications/prenatal-screening-down-s-syndrome-neural-tube-defects-routine-ultrasonography.
Mujezinovic F, Alfirevic Z : Procedure-related complications of amniocentesis and chorionic villous sampling; a systematic review. Obstetr Gynecol 2007; 110: 687–694.
Bui T-H, Meiner V : State of the art in prenatal diagnosis. In: Leuzinger-Bohleber M, Engels E-M, Tsiantis J (eds): The Janus Face of Prenatal Diagnostics. A European Study Bridging Ethics, Psycholanalysis, and Medicine. London: Karnac Books, 2008, pp 61–86.
Leung W, Lau E, Lau W et al: Rapid aneuploidy testing (knowing less) versus traditional karyotyping (knowing more) for advanced maternal age: what would be missed, who should decide? Hong Kong Med J 2008; 14: 6–13.
Caine A, Maltby AE, Parkin CA, Waters JJ, Crolla JA : Prenatal detection of Down's syndrome by rapid aneuploidy without a full karyotype: a cytogenetic risk assessment. Lancet 2005; 366: 123–128.
Bui T-H, Blennow E, Nordenskjöld M : Prenatal diagnosis: molecular genetics and cytogenetics. Best Practice Res Clin Obstetr Gynaecol 2002; 16: 629–643.
Mann K, Fox SP, Abbs SJ et al: Development and implementation of a new rapid aneuploidy diagnostic service within the UK National Health Service and implications for the future of prenatal diagnosis. Lancet 2001; 358: 1057–1061.
Ogilvie CM, Yaron Y, Beaudet AL : Current controversies in prenatal diagnosis 3: For prenatal diagnosis, should we offer less or more than metaphase karyotyping? Prenat Diagn 2009; 29: 11–14.
Boormans EA : Rapid Aneuploidy Detection in Prenatal Diagnosis. The Clinical use of Multiplex Ligation-Dependent Probe Amplification. Thesis, Amsterdam: Buijten & Schipperheijn, 2010.
de Jong A, Dondorp W, de Wert G : The scope of prenatal diagnostic testing for chromosomal aberrations: broad or narrow? Ethical considerations on the choice of tests. Ned Tijdschr Geneeskd 2009; 153: A1060 (in Dutch).
Bui T-H : Prenatal cytogenetic diagnosis: gone FISHing, BAC soon! Ultrasound Obstet Gynecol 2007; 30: 247–251.
Cirigliano V, Voglino G, Ordoñez E et al: Rapid prenatal diagnosis of common chromosome aneuploidies by QF-PCR, results of 9 years of clinical experience. Prenat Diagn 2009; 29: 40–49.
ACOG: ACOG Practice Bulletin No. 88: invasive prenatal testing for aneuploidy. Obestetr Gynecol 2007; 110: 1459–14567.
Boormans E, Birnie E, Oepkes D et al: Individualized choice in prenatal diagnosis: the impact of karyotyping and standalone rapid aneuploidy detection on quality of life. Prenat Diagn 2010; 30: 928–936.
The Swedish Council on Technology Assessment in Health Care (SBU): Methods of Early Prenatal Diagnosis. Report no: 182, 2006, available at: http://www.sbu.se/en/Published/Yellow/Methods-of-Early-Prenatal-Diagnosis/.
Mann K, Donaghue C, Fox S, Docherty Z, Ogilvie C : Strategies for the rapid prenatal diagnosis of chromosome aneuploidy. Eur J Hum Genet 2004; 12: 907–915.
UK National Screening Committee: NHS Fetal Anomaly Screening Programme – Screening for Down's syndrome: UK NSC Policy recommendations 2007-2010: Model of Best Practice, 2008, available at: http://www.dh.gov.uk/publications.
Health Council of the Netherlands: Screening: Between Hope and Hype, Publication no. 2008/05. The Hague: Health Council of the Netherlands, 2008, available at: http://www.gezondheidsraad.nl/sites/default/files/200805E_0.pdf.
Beauchamp TL, Childress JF : Principles of Biomedical Ethics. 6th edn. New York/Oxford: Oxford University Press Inc., 2008.
Nuffield Council on Bioethics: Genetic Screening, Ethical Issues. London: Nuffield Council on Bioethics, 1993, available at: http://www.nuffieldbioethics.org/genetic-screening.
Dudarewicz L, Holzgreve W, Jeziorowska A, Jakubowski L, Zimmermann B : Molecular methods for rapid detection of aneuploidy. J Appl Genet 2005; 46: 207–215.
Nicolini U, Lalatta F, Natacci F, Curcio C, Bui T-H : The introduction of QF-PCR in prenatal diagnosis of fetal aneuploidies: time for reconsideration. Hum Reprod Update 2004; 10: 541–548.
Ogilvie CM : Prenatal diagnosis for chromosome abnormalities: past, present and future. Pathol Biol 2003; 51: 156–160.
Leung TN : Rapid aneuploidy testing versus traditional karyotyping: is it better to know more? Hong Kong Med J 2008; 14: 4–5.
Boormans E, Birnie E, Knegt A, Schuring-Blom G, Bonsel G, van Lith J : Aiming at multidisciplinary consensus: what should be detected in prenatal diagnosis? Prenat Diagn 2010; 30: 1049–1056.
Ryan M, Diack J, Watson V, Smith N : Rapid prenatal diagnostic testing for Down syndrome only or longer wait for full karyotype: the views of pregnant women. Prenat Diagn 2005; 25: 1206–1211.
Chan Y, Sahota D, Leung T, Choy K, Chan O, Lau T : Chinese women's preferences for prenatal diagnostic procedure and their willingness to trade between procedures. Prenat Diagn 2009; 29: 1270–1276.
Grimshaw G, Szczepura A, Hultén M et al: Evaluation of molecular tests for prenatal diagnosis of chromosome abnormalities. Health Technol Assess 2003; 7: 1–146.
Ogilvie C, Lashwood A, Chitty L, Waters J, Scriven P, Flinter F : The future of prenatal diagnosis: rapid testing or full karyotype? An audit of chromosome abnormalities and pregnancy outcomes for women referred for Down's syndrome testing. BJOG 2005; 112: 1369–1375.
Boormans E, Birnie E, Oepkes D et al: The impact of rapid aneuploidy detection (RAD) in addition to karyotyping versus karyotyping on maternal quality of life. Prenat Diagn 2010; 30: 425–433.
Mujezinovic F, Prosnik A, Alfirevic Z : Different communication strategies for disclosing results of diagnostic prenatal testing. Cochrane Database Syst Rev 2010; 11: CD007750.
Kagan K, Chitty L, Cicero S, Eleftheriades M, Nicolaides K : Ultrasound findings before amniocentesis in selecting the method of analysing the sample. Prenat Diagn 2007; 27: 34–39.
Leung W, Waters J, Chitty L : Prenatal diagnosis by rapid aneuploidy detection and karyotyping: a prospective study of the role of ultrasound in 1589 second-trimester amniocenteses. Prenat Diagn 2004; 24: 790–795.
Gekas J, van den Berg D, Durand A et al: Rapid testing versus karyotyping in Down's syndrome screening: cost-effectiveness and detection of clinically significant chromosome abnormalities. Eur J Hum Genet 2011; 19: 3–9.
van Zwieten M : The Target of Testing. Dealing with ‘Unexpected’ Findings in Prenatal Diagnosis. Amsterdam: Uitgeverij Buijten & Schipperheijn, 2006, available at: http://www.myravanzwieten.nl/pdf/The_target_of_testing_Thesis.pdf.
van den Berg M, Timmermans D, Ten Kate L, van Vugt J, van der Wal G : Are pregnant women making informed choices about prenatal screening? Genet Med 2005; 7: 332–338.
Chervenak FA, McCullough LB, Sharma G, Davis J, Gross S : Enhancing patient autonomy with risk assessment and invasive diagnosis: an ethical solution to a clinical challenge. Am J Obstet Gynecol 2008; 199: 19.e11–19.e14.
Dickinson J, Harcourt E, Murch A : The selective use of rapid aneuploidy screening in prenatal diagnosis. Aust N Z J Obstet Gynaecol 2009; 49: 28–33.
Wenstrom KD : Aneuploidy screening: the changing scene. Obstet Gynaecol 2003; 101: 840–842.
Ormond KE, Iris M, Banuvar S, Minogue J, Annas GJ, Elias S : What do patients prefer: informed consent models for genetic carrier testing. J Genet Counsel 2007; 16: 539–550.
Donaghue C, Roberts A, Mann K, Ogilvie CM : Development and targeted application of a rapid QF-PCR test for sex chromosome imbalance. Prenat Diagn 2003; 23: 201–210.
Lo YMD, Chan KCA, Sun H et al: Maternal plasma DNA sequencing reveals the genome-wide genetic and mutational profile of the fetus. Sci Transl Med 2010; 2: 61ra91.
Chiu R, Akolekar R, Zheng Y et al: Non-invasive prenatal assessment of trisomy 21 by multiplexed maternal plasma DNA sequencing: large scale validity study. BMJ 2011; 342: c7401.
Lim A, Lim T, Hess M et al: Rapid aneuploidy screening with fluorescence in-situ hybridisation: is it a sufficiently robust stand-alone test for prenatal diagnosis? Hong Kong Med J 2010; 16: 427–433.
Zuffardi O, Vetro A, Brady P, Vermeesch J : Array technology in prenatal diagnosis. Semin Fetal Neonatal Med 2011; 16: 94–98.
Hillman S, Pretlove S, Coomarasamy A et al: Additional information from array comparative genomic hybridization technology over conventional karyotyping in prenatal diagnosis: a systematic review and meta-analysis. Ultrasound Obstet Gynecol 2011; 37: 6–14.
de Jong A, Dondorp W, de Die-Smulders C, Frints S, de Wert G : Non-invasive prenatal testing: ethical issues explored. Eur J Hum Genet 2010; 18: 272–277.
Acknowledgements
We thank professor Bartha Knoppers for her helpful comments on an earlier draft of this paper. This research was supported by the Centre for Society and Genomics, funded by the Netherlands Genomics Initiative (research project number: 70.1.061b).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
de Jong, A., Dondorp, W., Timmermans, D. et al. Rapid aneuploidy detection or karyotyping? Ethical reflection. Eur J Hum Genet 19, 1020–1025 (2011). https://doi.org/10.1038/ejhg.2011.82
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejhg.2011.82
Keywords
This article is cited by
-
FISH is not Suitable as a Standalone Test for Detecting Fetal Chromosomal Abnormalities
Journal of Fetal Medicine (2015)
-
Microarrays as a diagnostic tool in prenatal screening strategies: ethical reflection
Human Genetics (2014)
-
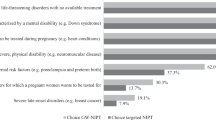
The scope of prenatal diagnosis for women at increased risk for aneuploidies: views and preferences of professionals and potential users
Journal of Community Genetics (2013)
-
Advances in prenatal screening: the ethical dimension
Nature Reviews Genetics (2011)