Abstract
Background/objectives:
There is limited information to support definitive recommendations concerning the role of diet in the development of type 2 Diabetes mellitus (T2DM). The results of the latest meta-analyses suggest that an increased consumption of green leafy vegetables may reduce the incidence of diabetes, with either no association or weak associations demonstrated for total fruit and vegetable intake. Few studies have, however, focused on older subjects.
Subjects/methods:
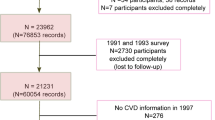
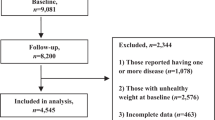
The relationship between T2DM and fruit and vegetable intake was investigated using data from the NIH-AARP study and the EPIC Elderly study. All participants below the age of 50 and/or with a history of cancer, diabetes or coronary heart disease were excluded from the analysis. Multivariate logistic regression analysis was used to calculate the odds ratio of T2DM comparing the highest with the lowest estimated portions of fruit, vegetable, green leafy vegetables and cabbage intake.
Results:
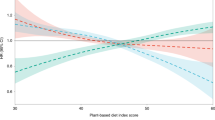
Comparing people with the highest and lowest estimated portions of fruit, vegetable or green leafy vegetable intake indicated no association with the risk of T2DM. However, although the pooled OR across all studies showed no effect overall, there was significant heterogeneity across cohorts and independent results from the NIH-AARP study showed that fruit and green leafy vegetable intake was associated with a reduced risk of T2DM OR 0.95 (95% CI 0.91,0.99) and OR 0.87 (95% CI 0.87,0.90) respectively.
Conclusions:
Fruit and vegetable intake was not shown to be related to incident T2DM in older subjects. Summary analysis also found no associations between green leafy vegetable and cabbage intake and the onset of T2DM. Future dietary pattern studies may shed light on the origin of the heterogeneity across populations.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Neel JV . Diabetes mellitus: a ‘thrifty’ genotype rendered detrimental by ‘progress’? Am J Hum Genet 1962; 14: 353.
Organization WH Diabetes 2011. Available at: www.who.int/mediacentre/factsheets/fs312/en/.
King H, Dowd J . Primary prevention of type 2 (non-insulin-dependent) diabetes mellitus. Diabetologia 1990; 33: 3–8.
Tuomilehto J, Wolf E . Primary prevention of diabetes mellitus. Diabetes Care 1987; 10: 238–248.
Tuomilehto J, Lindström J, Eriksson JG, Valle TT, Hämäläinen H, Ilanne-Parikka P et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 2001; 344: 1343–1350.
Hamman RF . Genetic and environmental determinants of non‐insulin‐dependent diabetes mellitus (NIDDM). Diabetes Metab Rev 1992; 8: 287–338.
Zimmet PZ . Primary prevention of diabetes mellitus. Diabetes Care 1988; 11: 258–262.
Stern MP . Kelly West lecture: primary prevention of type II diabetes mellitus. Diabetes Care 1991; 14: 399–410.
Manson JE, Stampfer M, Colditz G, Willett W, Rosner B, Hennekens C et al. Physical activity and incidence of non-insulin-dependent diabetes mellitus in women. Lancet 1991; 338: 774–778.
Carter P, Gray LJ, Troughton J, Khunti K, Davies MJ . Fruit and vegetable intake and incidence of type 2 diabetes mellitus: systematic review and meta-analysis. BMJ 2010; 341: c4229.
Li M, Fan Y, Zhang X, Hou W, Tang Z . Fruit and vegetable intake and risk of type 2 diabetes mellitus: meta-analysis of prospective cohort studies. BMJ open 2014; 4: e005497.
Wu Y, Zhang D, Jiang X, Jiang W . Fruit and vegetable consumption and risk of type 2 diabetes mellitus: A dose-response meta-analysis of prospective cohort studies. Nutr Metab Cardiovasc Dis 2015; 25: 140–147.
Cooper AJ, Forouhi NG, Ye Z, Buijsse B, Arriola L, Balkau B et al. Fruit and vegetable intake and type 2 diabetes: EPIC-InterAct prospective study and meta-analysis. Eur J Clin Nutr 2012; 66: 1082–1092.
Boffetta P, Bobak M, Borsch-Supan A, Brenner H, Eriksson S, Grodstein F et al. The Consortium on health and ageing: network of cohorts in Europe and the United States (CHANCES) project—design, population and data harmonization of a large-scale, international study. Eur J Epidemiol 2014; 29: 929–936.
Trichopoulou A, Orfanos P, Norat T, Bueno-de-Mesquita B, Ocké MC, Peeters PH et al. Modified Mediterranean diet and survival: EPIC-elderly prospective cohort study. Brit Med J 2005; 330: 991.
Schatzkin A, Subar AF, Thompson FE, Harlan LC, Tangrea J, Hollenbeck AR et al. Design and serendipity in establishing a large cohort with wide dietary intake distributions: the National Institutes of Health-American Association of Retired Persons Diet and Health Study. Am J Epidemiol 2001; 154: 1119–1125.
Riboli E, Kaaks R . The EPIC Project: rationale and study design. European prospective investigation into cancer and nutrition.. Int J Epidemiol 1997; 26, (Suppl 1) S6.
Jankovic N, Geelen A, Streppel MT, de Groot LC, Orfanos P, van den Hooven EH et al. Adherence to a healthy diet according to the world health organization guidelines and all-cause mortality in elderly adults from Europe and the United States. Am J Epidemiol 2014; 180: 978–988.
Center for disease control, National diabetes fact sheet. Retrieved June 30 2005: p. 2007.
DerSimonian R, Laird N . Meta-analysis in clinical trials. Control Clin Trials 1986; 7: 177–188.
Hamer M, Chida Y . Intake of fruit, vegetables, and antioxidants and risk of type 2 diabetes: systematic review and meta-analysis. J Hypertens 2007; 25: 2361–2369.
Ford ES, Mokdad AH . Fruit and vegetable consumption and diabetes mellitus incidence among US adults. Prev Med 2001; 32: 33–39.
Cooper AJ, Sharp StephenJ, Lentjes MarleenAH, Luben RobertN, Khaw Kay-Tee, Wareham NicholasJ et al. Dietary fibre and incidence of type 2 diabetes in eight European countries: the EPIC-InterAct study and a meta-analysis of prospective studies. Diabetologia 2015; 58: 1394–1408.
Yao B, Fang H, Xu W, Yan Y, Xu H, Liu Y et al. Dietary fiber intake and risk of type 2 diabetes: a dose–response analysis of prospective studies. Eur J Epidemiol 2014; 29: 79–88.
Schulze MB, Schulz M, Heidemann C, Schienkiewitz A, Hoffmann K, Boeing H . Fiber and magnesium intake and incidence of type 2 diabetes: a prospective study and meta-analysis. Arch Intern Med 2007; 167: 956–965.
Stanhope KL, Schwarz JM, Havel PJ . Adverse metabolic effects of dietary fructose: results from recent epidemiological, clinical, and mechanistic studies. Curr Opin Lipidol 2013; 24: 198.
Ledoux T, Hingle M, Baranowski T . Relationship of fruit and vegetable intake with adiposity: a systematic review. Obes Rev 2011; 12: e143–e150.
Abdullah A, Peeters A, De Courten M, Stoelwinder J . The magnitude of association between overweight and obesity and the risk of diabetes: a meta-analysis of prospective cohort studies. Diabetes Res Clin Prac 2010; 89: 309–319.
Xi B, Li S, Liu Z, Tian H, Yin X, Huai P et al. Intake of fruit juice and incidence of type 2 diabetes: a systematic review and meta-analysis. PLoS One 2014; 9: e93471.
Agte V, Tarwadi K, Mengale S, Chiplonkar S . Potential of traditionally cooked green leafy vegetables as natural sources for supplementation of eight micronutrients in vegetarian diets. J Food Compos Anal 2000; 13: 885–891.
Tarwadi K, Agte V . Potential of commonly consumed green leafy vegetables for their antioxidant capacity and its linkage with the micronutrient profile. Int J Food Sci Nutr 2003; 54: 417–425.
Dong J-Y, Xun P, He K, Qin L-Q . Magnesium intake and risk of type 2 diabetes meta-analysis of prospective cohort studies. Diabetes Care 2011; 34: 2116–2122.
Lidder S, Webb AJ . Vascular effects of dietary nitrate (as found in green leafy vegetables and beetroot) via the nitrate‐nitrite‐nitric oxide pathway. Br J Clin Pharmacol 2013; 75: 677–696.
Gilchrist M, Winyard PG, Fulford J, Anning C, Shore AC, Benjamin N . Dietary nitrate supplementation improves reaction time in type 2 diabetes: development and application of a novel nitrate-depleted beetroot juice placebo. Nitric Oxide 2014; 40: 67–74.
Robinson S, Syddall H, Jameson K, Batelaan S, Martin H, Dennison EM et al. Current patterns of diet in community-dwelling older men and women: results from the Hertfordshire Cohort Study. Age Ageing 2009; 38: afp121.
Song Y, Manson JE, Buring JE, Liu S . A prospective study of red meat consumption and type 2 diabetes in middle-aged and elderly women: the women's health study. Diabetes Care 2004; 27: 2108–2115.
Severi S, Bedogni G, Manzieri A, Poli M, Battistini N . Effects of cooking and storage methods on the micronutrient content of foods. Eur J Cancer Prev 1997; 6: S21–S24.
Clarke R, Shipley M, Lewington S, Youngman L, Collins R, Marmot M et al. Underestimation of risk associations due to regression dilution in long-term follow-up of prospective studies. Am J Epidemiol 1999; 150: 341–353.
Acknowledgements
This work was supported by funding from the European Community’s Seventh Framework Programme (FP7/2007-2013) (grant number HEALTH –F3-2010-242244). This research was supported (in part) by the Intramural Research Program of the NIH, National Cancer Institute. Cancer incidence data from the Atlanta metropolitan area were collected by the Georgia Center for Cancer Statistics, Department of Epidemiology, Rollins School of Public Health, Emory University, Atlanta, Georgia. Cancer incidence data from California were collected by the California Cancer Registry, California Department of Public Health’s Cancer Surveillance and Research Branch, Sacramento, California. Cancer incidence data from the Detroit metropolitan area were collected by the Michigan Cancer Surveillance Program, Community Health Administration, Lansing, Michigan. The Florida cancer incidence data used in this report were collected by the Florida Cancer Data System (Miami, Florida) under contract with the Florida Department of Health, Tallahassee, Florida. The views expressed herein are solely those of the authors and do not necessarily reflect those of the FCDC or FDOH. Cancer incidence data from Louisiana were collected by the Louisiana Tumor Registry, Louisiana State University Health Sciences Center School of Public Health, New Orleans, Louisiana. Cancer incidence data from New Jersey were collected by the New Jersey State Cancer Registry, Cancer Epidemiology Services, New Jersey State Department of Health, Trenton, New Jersey. Cancer incidence data from North Carolina were collected by the North Carolina Central Cancer Registry, Raleigh, North Carolina. Cancer incidence data from Pennsylvania were supplied by the Division of Health Statistics and Research, Pennsylvania Department of Health, Harrisburg, Pennsylvania. The Pennsylvania Department of Health specifically disclaims responsibility for any analyses, interpretations or conclusions. Cancer incidence data from Arizona were collected by the Arizona Cancer Registry, Division of Public Health Services, Arizona Department of Health Services, Phoenix, Arizona. Cancer incidence data from Texas were collected by the Texas Cancer Registry, Cancer Epidemiology and Surveillance Branch, Texas Department of State Health Services, Austin, Texas. Cancer incidence data from Nevada were collected by the Nevada Central Cancer Registry, Division of Public and Behavioral Health, State of Nevada Department of Health and Human Services, Carson City, NevadaNevada.We are indebted to the participants in the NIH-AARP Diet and Health Study for their outstanding cooperation. We also thank Sigurd Hermansen and Kerry Grace Morrissey from Westat for study outcomes ascertainment and management and Leslie Carroll at Information Management Services for data support and analysis.Ethical standard: All of the cohorts obtained ethical approval and written informed consent was obtained from all participants.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Mamluk, L., O'Doherty, M., Orfanos, P. et al. Fruit and vegetable intake and risk of incident of type 2 diabetes: results from the consortium on health and ageing network of cohorts in Europe and the United States (CHANCES). Eur J Clin Nutr 71, 83–91 (2017). https://doi.org/10.1038/ejcn.2016.143
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2016.143
This article is cited by
-
Prevalence and characteristics of metabolic syndrome and its components among adults living with and without HIV in Nigeria: a single-center study
BMC Endocrine Disorders (2023)
-
EAT-Lancet Healthy Reference Diet score and diabetes incidence in a cohort of Mexican women
European Journal of Clinical Nutrition (2023)
-
Health effects associated with vegetable consumption: a Burden of Proof study
Nature Medicine (2022)
-
Association of fruit and vegetable color with incident diabetes and cardiometabolic risk biomarkers in the United States Hispanic/Latino population
Nutrition & Diabetes (2022)
-
Fruit and vegetable intake and risk of prediabetes and type 2 diabetes: results from a 20-year long prospective cohort study in Swedish men and women
European Journal of Nutrition (2022)