Abstract
Objective: The aim of the present study was to investigate whether adult patients with coeliac disease in remission could include large amounts of oats in their daily gluten-free diet for an extended period of time without adverse effects.
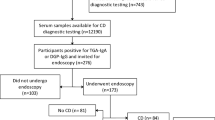
Design, subjects and methods: Twenty adult coeliac patients in remission included large amounts of uncontaminated rolled oats in their daily diet for a prolonged period. The examinations, performed four times during the study period, included small bowel endoscopy with biopsies, blood samples (nutritional status, serological analysis), height and body weight, gastrointestinal symptoms and dietary records. Gastrointestinal symptoms and diet were also investigated through unannounced telephone interviews once a month during the study period.
Results: No adverse effects of a large intake of oats were seen in small bowel histology, serology nor in nutritional status in the 15 subjects who completed the whole study period. Two of the subjects dropped out because of gastrointestinal symptoms and three for non-medical reasons. The median intake of oats was 93 g/day and the compliance to the oat diet was found to be good. Examinations of the patients after drop-out did not show any deterioration in small bowel histology or nutritional status nor raised levels of antibodies.
Conclusion: Results from this study indicate that adult patients with coeliac disease in remission can include large amounts of controlled wheat-free rolled oats for an extended period of time without adverse effects.
Sponsorship: This study was supported by Vårdalstiftelsen, Kommunalförbundet Västra Götaland, Stiftelsen Cerealia FoU, and the Swedish Nutrition Foundation. Kungsörnen AB supported the study with rolled oats.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Ascher, H, Hahn-Zoric, M, Hanson, LÅ, Kilander, AF, Nilsson, LÅ & Tlaskalova, H (1996). Value of serologic markers for clinical diagnosis and population studies of coeliac disease. Scand. J. Gastroenterol., 31, 61–67.
Baker, PG & Read, AE (1976). Oats and barley toxicity in coeliac patients. Postgrad. Med. J., 52, 264–268.
Brohult, S & Sandegren, E (1954). Proteins: Chemistry, Biological Activity, and Methods: Part B, New York: Academic Press
Buzzard, M (1998). 24-Hour Dietary Recall and Food Record Methods, 2nd ed Oxford: Oxford University Press
Catassi, C, Rossini, M, Ratsch, IM, Bearzi, I, Santinelli, A, Castagnani, R, Pisani, E, Coppa, GV & Giorgi, PL (1993). Dose dependent effects of protracted ingestion of small amounts of gliadin in coeliac disease children: a clinical and jejunal morphometric study. Gut, 34, 1515–1519.
Chartrand, L, Russo, P, Duhaime, A & Seidman, E (1997). Wheat starch intolerance in patients with coeliac disease. Am. J. Diet. Assoc., 97, 612–618.
Cornell, H, Wieser, H & Belitz, HD (1992). Characterization of the gliadin-derived peptides which are biologically active in coeliac disease. Clin. Chim. Acta, 213, 37–50.
De Vincenzi, M, Luchetti, R, Peruffo, AD, Curioni, A, Pogna, NE & Gasbarrini, G (1996). In vitro assessment of acetic-acid-soluble proteins (glutenin) toxicity in coeliac disease. J. Biochem. Toxicol., 11, 205–210.
Dicke, W (1950). En onderzoek naar de nadlige invloed van sommige graansoorten op de lijder aan coeliakie. Dissertation. University of Utrecht
Dicke, W, Weijers, H & van der Kamer, J (1953). Coeliac disease. II. The presence in wheat of a factor having a deleterious effect in causes of coeliac disease. Acta. Paediatr., 42, 34–42.
Hardman, CM, Garioch, JJ, Leonard, JN, Thomas, HJ, Walker, MM, Lortan, JE, Lister, A & Fry, L (1997). Absence of toxicity of oats in patients with dermatitis herpetiformis. New Engl. J. Med., 337, 1884–1887.
Holmes, GK, Prior, P, Lane, MR, Pope, D & Allan, RN (1989). Malignancy in coeliac disease—effect of a gluten free diet. Gut, 30, 333–338.
Janatuinen, EK, Pikkarainen, PH, Kemppainen, TA, Kosma, VM, Jarvinen, RM, Uusitupa, MI & Julkunen, RJ (1995). A comparison of diets with and without oats in adults with coeliac disease. New Engl. J. Med., 333, 1033–1037.
Janatuinen, EK, Kemppainen, TA, Pikkarainen, PH, Holm, KIT, Kosma, VM, Uusitupa, MI, Maki, M & Julkunen, RJ (2000). Lack of cellular and humoral immunological responses to oats in adults with coeliac disease. Gut, 46, 327–331.
Janatuinen, EK, Kemppainen, TA, Julkunen, RJ, Kosma, VM, Maki, M, Heikkinen, M & Uusitupa, MI (2002). No harm from five year ingestion of oats in coeliac disease. Gut, 50, 332–335.
Kaukinen, K, Collin, P, Holm, K, Rantala, I, Vuolteenaho, N, Reunala, T & Maki, M (1999). Wheat starch-containing gluten-free flour products in the treatment of coeliac disease and dermatitis herpetiformis. A long-term follow-up study. Scand. J. Gastroenterol., 34, 163–169.
Kilander, AF, Dotevall, G, Fallstrom, SP, Gillberg, RE, Nilsson, LA & Tarkowski, A (1983). Evaluation of gliadin antibodies for detection of coeliac disease. Scand. J. Gastroenterol., 18, 377–383.
Kluge, F, Koch, HK, Grosse-Wilde, H, Lesch, R & Gerok, W (1982). Follow-up of treated adult coeliac disease: clinical and morphological studies. Hepatogastroenterology, 29, 17–23.
Kumar, PJ, Walker-Smith, J, Milla, P, Harris, G, Colyer, J & Halliday, R (1988). The teenage celiac: follow up study of 102 patients. Arch. Dis. Child., 63, 916–920.
Lindberg, T, Nilsson, LA, Borulf, S, Cavell, B, Fallstrom, SP, Jansson, U, Stenhammar, L & Stintzing, G (1985). Serum IgA and IgG gliadin antibodies and small intestinal mucosal damage in children. J. Pediatr. Gastroenterol. Nutr., 4, 917–922.
Lohiniemi, S, Maki, M, Kaukinen, K, Laippala, P & Collin, P (2000). Gastrointestinal symptoms rating scale in coeliac disease patients on wheat starch-based gluten-free diets. Scand J. Gastroenterol., 35, 947–949.
Mayer, M, Greco, L, Troncone, R, Auricchio, S & Marsh, MN (1991). Compliance of adolescents with coeliac disease with a gluten free diet. Gut, 32, 881–885.
Moulton, A (1959). The place of oats in coeliac diet. Arch. Dis. Child., 34, 51–55.
Picarelli, A, Di Tola, M, Sabbatella, L, Gabrielli, F, Di Cello, T, Anania, MC, Mastracchio, A, Silano, M & De Vincenzi, M (2001). Immunologic evidence of no harmful effect of oats in celiac disease. Am. J. Clin. Nutr., 74, 137–140.
Reunala, T, Collin, P, Holm, K, Pikkarainen, P, Miettinen, A, Vuolteenaho, N & Mäki, M (1998). Tolerance to oats in dermatitis herpetiformis. Gut, 43, 490–493.
Ripsin, CM, Keenan, JM, Jacobs, DR, Elmer, PJ, Welch, RR & Van Horn, L et al (1992). Oat products and lipid lowering. A meta-analysis. JAMA, 267, 3317–3325.
Schmitz, J (1997). Lack of oats toxicity in coeliac disease. Toxic fractions makes up less of total protein than in other cereals. Br. Med. J., 314, 159–160.
Selby, WS, Painter, D, Collins, A, Faulkner-Hogg, KB & Loblay, RH (1999). Persistent mucosal abnormalities in coeliac disease are not related to the ingestion of trace amounts of gluten. Scand. J. Gastroenterol., 34, 909–914.
Skerrit, JH & Hill, AS (1991). Enzyme immunoassay for determination of gluten in foods. Collaborative study. J. Assoc. Off. Anal. Chem., 72, 257–264.
Srinivasan, U, Leonard, N, Jones, F, Kasarda, DD, Weir, DG, O'Farrelly, C & Feighery, C (1996). Absence of oats toxicity in adult coeliac disease. Br. Med. J., 313, 1300–1301.
Swedish National Food Administration (1993). Food Composition Table—Energy and Nutrients, Uppsala: Norstedts Press
Thompson, T (1997). Do oats belong to a gluten-free diet?. J. Am. Diet. Assoc., 97, 1413–1416.
Trier, JS (1991). Coeliac sprue. New Engl. J. Med., 325, 1709–1719.
Valdimarsson, T, Löfman, O, Toss, G & Ström, M (1996). Reversal of osteopenia with diet in adult coeliac disease. Gut, 38, 322–327.
Wieser, H (1995). The precipitating factor in coeliac disease. Baillieres Clin. Gastroenterol., 9, 191–207.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Størsrud, S., Olsson, M., Arvidsson Lenner, R. et al. Adult coeliac patients do tolerate large amounts of oats. Eur J Clin Nutr 57, 163–169 (2003). https://doi.org/10.1038/sj.ejcn.1601525
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ejcn.1601525
Keywords
This article is cited by
-
Gastrointestinal Effects of Eating Quinoa ( Chenopodium quinoa Willd.) in Celiac Patients
American Journal of Gastroenterology (2014)
-
Nutrient intakes during diets including unkilned and large amounts of oats in celiac disease
European Journal of Clinical Nutrition (2010)
-
Generation and analysis of 9792 EST sequences from cold acclimated oat, Avena sativa
BMC Plant Biology (2005)