Abstract
Data sources
Cochrane Oral Health Group's Trials Register, Central, Medline, Embase, PsycINFO.
Study selection
Randomised controlled trials of psychosocial interventions for chronic orofacial pain were included. Psychosocial interventions targeted towards changing thoughts, behaviours and/or feelings that may exacerbate pain symptoms through a vicious cycle were eligible. Primary outcomes were pain intensity/severity, satisfaction with pain relief and quality of life.
Data extraction and synthesis
Two reviewers independently screened studies, extracted data and assessed risk of bias. Dichotomous outcomes, were expressed as risk ratios with 95% confidence intervals, continuous outcomes as mean differences with 95% confidence intervals. Heterogeneity was assessed using the Cochrane test for heterogeneity and the I2 test. Meta-analyses were conducted using the random-effect or the fixed-effect models.
Results
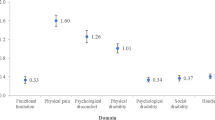
Fifteen of the 17 eligible studies were on temporomandibular disorders (TMDs), two on burning mouth syndrome. Psychosocial interventions improved long-term pain intensity (standardised mean difference (SMD) -0.34, 95% confidence interval (CI) -0.50 to -0.18) and depression (SMD -0.35, 95% CI -0.54 to -0.16). However, the risk of bias in these studies was high.
Conclusions
There is weak evidence to support the use of psychosocial interventions for chronic orofacial pain.
Similar content being viewed by others
Commentary
The prevalence of TMDs ranges between 5-12% of the population, with a relatively higher rate among younger cohorts.1 Apart from the commonality of orofacial pain, patients afflicted by chronic pain are likely to have experienced a complex and multi-staged journey through the health care system.2 At some stage, often after patients have endured multiple tests and treatments, the possibility of psychosocial determinants or contributors to the pain is entertained. By this time, as Aggarwal et al. point out, the ‘anxiety-pain-tension’ cycle is likely to have led to an increased perception of pain or to the presence of debilitating avoidance behaviours.
While this synthesis of the relevant evidence base is original, the efficacy of a range of psychosocial interventions has been widely established. Cognitive behaviour therapy (CBT), for example, has accumulated a considerable body of evidence with respect to its efficacy across a range of mental and physical disorders, illnesses and diseases.3,4 The evidence base for CBT, in particular, includes effective support for patients with medically unexplained symptoms.5
Due to clinical need and the presence of sound treatment options, this review is a welcome and timely exploration of non-invasive psychosocial treatments for patients suffering from orofacial pain.
The authors start the presentation of their findings by stating that with respect to short-term outcomes, usual care performed better than psychosocial interventions in reducing pain intensity. However, in the long-term and after follow up, Dworkin self-care interventions, habit reversal, and particularly CBT approaches (either with or without biofeedback) are significantly more effective in reducing pain intensity than usual care (or no care in the case of habit reversal). CBT and Dworkin self-care interventions were also outperforming usual care in reducing the impact of pain on daily living activities. In terms of reducing symptoms of depression, CBT alone or in combination with biofeedback and hypnosis were significantly more effective than usual care.
This endorsement of psychosocial interventions is moderated by the fact that the research designs have a high risk of bias and the study populations were exclusively from tertiary care settings. Thus, they conclude that non-invasive psychosocial interventions are supported by only weak evidence. However, they also note that although weak, this still constitutes a stronger evidence base than is available for the usual and more invasive procedures.
References
National Institute of Dental and Craniofacial Research. Prevalence of TMJD and Its Signs and Symptoms. 2012 [cited 2012 17.2.12]; Available from: http://www.nidcr.nih.gov/datastatistics/finddatabytopic/facialpain/prevalencetmjd.htm.
Allcock N, Elkan R, Williams J . Patients referred to a pain management clinic: beliefs, expectations and priorities. J Adv Nurs 2007; 60: 248–256.
Gaudiano BA . Cognitive-behavioural therapies: achievements and challenges. Evid Based Ment Health 2008; 11: 5–7.
Butler AC, Chapman JE, Forman EM, Beck AT . The empirical status of cognitive–behavioral therapy: A review of meta-analyses. Clin Psychol Rev. 2006; 26: 17–31.
Allen LA, Woolfolk RL, Escobar JI, Gara MA, Hamer RM . Cognitive–behavioral therapy for somatization disorder: a randomized controlled trial. Arch Intern Med. 2006; 166: 1512–1518.
Author information
Authors and Affiliations
Additional information
Address for correspondence: Vishal R Aggarwal, Oral Health Unit, National Primary Care Research and Development Centre, School of Dentistry, The University of Manchester, Higher Cambridge Street, Manchester, M15 6FH, UK. E-mail: vishal.r.aggarwal@manchester.ac.uk
Aggarwal VR, Lovell K, Peters S, Javidi H, Joughin A, Goldthorpe J. Psychosocial interventions for the management of chronic orofacial pain. Cochrane Database Syst Rev 2011 Nov 9; 11: CD008456
This paper is based on a Cochrane Review published in the Cochrane Library 2011, issue 11 (see www.thecochranelibrary.com for information). Cochrane Reviews are regularly updated as new evidence emerges and in response to feedback, and the Cochrane Library should be consulted for the most recent version of the review.
Rights and permissions
About this article
Cite this article
Themessl-Huber, M. Weak evidence supports the use of psychosocial interventions for chronic orofacial pain. Evid Based Dent 13, 58 (2012). https://doi.org/10.1038/sj.ebd.6400865
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ebd.6400865