Abstract
Normative body composition during the first 2 y of life was derived from a prospective study of 76 children. We present 1) fat free mass (FFM) and its components, and fat mass (FM), 2) incremental growth rates partitioned into chemical components, and 3) age-specific and gender-specific constants for converting chemical and physical components into FFM for children during the first 2 y of life. A multicomponent model based on measurements of total body water (TBW), total body potassium (TBK) and bone mineral content (BMC) was used to estimate FFM and FM at 0.5, 3, 6, 9, 12, 18, and 24 mo of age. TBW was determined by deuterium dilution, TBK by whole body counting, and BMC by dual energy x-ray absorptiometry. FFM was higher in boys than girls between 0.5–18 mo of age (p ≤ 0.05). Percent FM increased on average from 13 to 31% between 0.5 and 3–6 mo, and then gradually declined. Percent FM was significantly higher in girls than in boys at 6 and 9 mo of age (p ≤ 0.02). The components of FFM on a percentage basis changed with age (p = 0.001), but not gender. The protein content of FFM increased gradually with age, while TBW declined (p = 0.001). As a percentage of FFM, osseous mineral increased from 2.0 to 3.4% in boys and from 2.1 to 3.3% in girls between 0.5 and 24 mo (p = 0.001). Density and potassium content of FFM increased gradually with age (p = 0.001). These normative body composition data provide an updated reference upon which to assess normal growth and nutritional status of pediatric populations representative of mixed feeding groups during the first 2 y of life.
Similar content being viewed by others
Main
Human growth during the first 2 y of life involves not only quantitative changes in body size, but also qualitative changes in composition. Clinical assessment of growth and nutritional status is enhanced by accurate measurement of body composition whether one is assessing undernutrition or overnutrition, or monitoring the natural course of chronic disease or the response to diet or drug interventions. However, body composition methods used in adults are not always directly applicable to pediatric populations. Throughout infancy, childhood, and adolescence, there is a gradual change in the chemical composition of fat free mass (FFM). Two-compartment models, which partition the body into FFM and fat mass (FM), are influenced by age and maturation. The use of age-specific and gender-specific constants for converting chemical components such as total body water (TBW) and total body potassium (TBK), and body density into FFM can eliminate systematic errors in body composition methods. The classic body composition model by Fomon et al. published in 1982 (1) provides age-specific and gender-specific constants for children from birth to 10 y of age. However, the authors stated, “Although we believe that these constants are more suitable than constants based on composition of the adult reference man, the constants and the other estimates of body composition presented here must be considered preliminary and crude because of uncertainties about the data and because of the large number of assumptions that have been required.” The major limitations as outlined by the authors were 1) the absence of data on TBW, TBK, and/or total body calcium at most ages;2) the necessity to use data from different laboratories;3) the difficulty of relating 40K counts to TBK; and 4) the difficulty of translating results from two-dimensional photon absorptiometry into total body calcium. Using these age-specific and gender-specific factors, we compared two-compartment models based on TBW, TBK, total body electrical conductivity (TOBEC), and dual energy x-ray absorptiometry (DXA) measurements in infants and toddlers and concluded that the methods were not interchangeable (2). In part, discrepancies between methods might have been due to the limitations associated with two-compartment models (3) or the use of conversion constants based on the infant and children reference model (1).
To circumvent errors arising from two-compartment models, we estimated body composition from a multicomponent model based on TBW, TBK, and bone mineral content (BMC) measurements of 76 children studied longitudinally during the first 2 years of life. These longitudinal data along with improved technology and application of a multicomponent model should provide a more accurate assessment of body composition of children during the first 2 y of life.
MATERIALS AND METHODS
Study design and subjects.
Repeated anthropometric and body composition measurements of TBW and TBK were performed on 76 healthy, normally growing term infants at 0.5, 3, 6, 9, 12, 18, and 24 mo of age at the Children's Nutrition Research Center. BMC was measured at 0.5, 12, and 24 mo only. Seventy-two children completed the 24-mo study. Mean ± SD birth weight and length of the 76 infants were 3.42 ± 0.44 kg and 50.56 ± 2.24 cm, respectively. Mean gestational age was 39.1 ± 1.3 wk. By study design, the infants were either exclusively breast-fed (n = 40) or formula-fed (n = 36) from birth to 4 mo of age; thereafter, feeding preference was at the discretion of the parents. Ethnic distribution by maternal lineage consisted of 55 Caucasian, 7 African-American, 11 Hispanic and 3 Asian children. This study was approved by the Baylor Affiliates Review Boards for Human Subject Research, and informed written consent was obtained from each child's mother.
Infants were admitted to the Children's Nutrition Research Center (CNRC) Metabolic Research Unit from approximately 1000 to 1700 h for the series of anthropometric and body composition measurements. First, anthropometric measurements were performed at least 1 h after feeding. The infant was dressed and cotton balls were placed into the infant's diaper to collect the baseline urine sample before 2H2O dosing. The 2H2O dose was administered orally using a syringe, at least 30 min after eating to avoid regurgitation of the dose. The 15-min whole body counting of 40K and the DXA measurement were usually performed on the younger infants while sleeping. By 18–24 mo, measurements could be done in the awake state, while the children were entertained with a video inside the counter or nearby the DXA.
Anthropometry.
Infants were weighed naked on an electronic integrating scale at least 30 min after feeding (Sartorius MC1, LC34 , Gottingen, Germany; precision ±1.0 g). Crown-to-heel length was measured on a recumbent infant board to the nearest 1 mm by two trained persons (Holtain Limited, Crymych, UK).
Total body water.
TBW was determined by dilution of an orally administered dose of 99.8 atom percent deuterium oxide (50 or 100 mg of 2H2O/kg body weight). Urine samples were collected before dosing, and 3–5 h after dosing or daily for 10 d. Before analysis, hydrogen gas was generated from undistilled urine samples by zinc reduction in quartz vessels (4, 5). 2H abundance in the urine samples was measured by gas-isotope-ratio mass spectrometry (Delta-E, Finnigan MAT, San Jose, CA). Deuterium dilution space was calculated from the average of two post-dose urine samples by the plateau method at 0.5 mo of age, and from 10 daily urine samples by the extrapolation method at all other ages. The deuterium dilution space (NH) was calculated using. MATH 1 where D is the dose of 2H2O in grams;A is the amount of laboratory water, in grams, used in the dose dilution; α is the amount of 2H2O, in grams, added to the laboratory water in the dose dilution;Eα is the rise in 2H abundance, per mil, in the laboratory water after the addition of the isotopic water;Ed is the rise in 2H abundance, per mil, in the post-dose urine sample. Deuterium dilution space was converted to TBW by dividing by 1.04.
Total body potassium.
TBK was estimated from the 40K naturally present in the child's body using a whole body counter (6). 40K emits high-energy gamma rays at the constant rate of 200.4 photons/min per g potassium. Photons are detected by 12 photon-sensitive NaI(Tl) detectors arranged in two arrays above and below the child's body in the low-background whole body counter. For the 15-min counting, the younger children were swaddled and placed in a plastic bassinet. The older children were secured on a hammock with straps. A custom set of four phantoms was used for routine quality control of the instrument. The in vivo precision for TBK measurements of infants and toddlers is less than 2.5% (6).
Dual-energy x-ray absorptiometry.
DXA was used to estimate total body BMC at 0.5, 12, and 24 mo only. The body was scanned in the single-beam mode with an aluminum table pad designed to improve instrument linearity and reduce radiation dose (QDR-2000, Infant Whole Body, analysis version 5.56–5.71P; Hologic, Inc., Waltham, MA). For the DXA scan, the child, diapered and lightly dressed, was placed supine on the pad with an interposing paper sheet. No sedation was used. The DXA scan was usually performed on the younger infants while sleeping. If significant movement of the head or limbs was encountered, the scan was stopped and repeated. A step phantom was placed beside the child for soft tissue calibration. The precision of the DXA measurement was determined for BMC (1.2 - 4.1%) based on repeated measurements on pigs weighing 4.6–15.7 kg (7).
To predict BMC when measurements were not available, a prediction equation was developed using linear regression of BMC on TBK, heel-crown length, age and gender at 0.5, 12, and 24 mo. Heel-crown length and gender were not significant, and therefore, were eliminated from the model. The final prediction equation was as follows: math
Multicomponent body composition model.
The multicomponent body composition model entailed the following assumptions. Intracellular and extracellular water were estimated using only the TBW and TBK data and the known concentrations of potassium in these compartments (4 and 150 mEq/kg water, respectively) (1). Body protein mass was based on the ratio of nitrogen to potassium (461 mg/mEq), and that nitrogen is 16% of protein (1). The concentrations of minerals in extracellular water (ECW) and intracellular water (ICW) were assumed to be 9.4 and 9.0 g/kg water, and glycogen was assumed to be equal to 0.45% of body weight (1). At ages 0.5, 12, and 24 mo, measured values of BMC were used in the model. At ages 3, 6, 9, and 18 mo, BMC was derived from the prediction equation (Eq. 2).
Computations were performed on an individual basis and averaged for each gender-age interval. The incremental gains in TBW, protein, FFM, and FM were calculated for individuals at each age interval and then averaged for each gender. The computations performed are summarized in the following equations: MATH 3 MATH 4 MATH 5 MATH 6 MATH 7 MATH 8 MATH 9 MATH 10 MATH 11 The volumes of the body and FFM used to calculate their respective densities were based on the following equations (8): MATH 12 MATH 13 MATH 14 MATH 15
Statistics.
Values are reported as means ± SD. Microsoft Access for Windows 95 (version 7, Microsoft Corp., Redmond, Washington, U.S.A.) was used for database management. Minitab (release 12, Minitab Inc., 1998) and BMDP (release 7, BMDP Statistics Software, Inc., 1992) were used for data description and statistical analysis. Repeated measures analysis of variance (BMDP5V) was used to test for the effects of age and gender on body composition. The model included a grouping factor (gender), a time factor (age at 0.5, 3, 6, 9, 12, 18, 24 mo), and interaction between gender and time. Significant interactions were tested further by making comparisons between boys and girls using one-way ANOVA.
RESULTS
Length, weight, and the chemical components used to estimate body composition are presented in Table 1. Length (p = 0.06) and weight (p = 0.22) did not differ statistically between the boys and girls. TBK increased with age (p = 0.001) and displayed a significant gender effect (M > F;p = 0.045). BMC averaged 68 ± 13, 221 ± 33, and 321 ± 38 g in boys, and 68 ± 12, 208 ± 31, and 298 ± 48 g in girls at 0.5, 12, and 24 mo of age, respectively. Differences in TBW and measured BMC were dependent on age*gender interactions (p = 0.02, 0.006). Overall, TBW and BMC were higher in boys than girls, with the difference generally increasing with age.
FFM and FM derived from the multicomponent model are presented in Table 2. FFM increased with age (p = 0.001). Gender differences in FFM were age dependent (p = 0.014). FFM was higher at 0.5 mo (p = 0.056) and between 3–18 mo of age (p ≤ 0.03) for boys compared with girls. FM also increased with age (p = 0.001), whereas FM, expressed as a percent of body weight (%FM), increased initially between 0.5 and 3–6 mo, and then gradually declined. Although FM did not differ by gender, %FM was significantly higher in girls than boys at 6 and 9 mo of age (p ≤ 0.02).
The composition of FFM expressed as a percentage of weight is presented in Table 3. The percentage of protein decreased in the first 6 mo, and increased thereafter. A significant gender effect was seen (M > F;p = 0.03), reflective of the gender effect on TBK, TBW, and ECW, as a percentage of weight, decreased between 0.5–3 mo, and were relatively stable thereafter. As a percentage of weight, osseous mineral increased from 1.8 to 2.6% in boys and from 1.9 to 2.5% in girls between 0.5 and 24 mo (p = 0.001).
The components of FFM on a percentage basis (%FFM) are displayed in Table 4. All components displayed significant age (p = 0.001), but not gender effects. The protein content of FFM increased gradually with age, while TBW and ECW declined (p = 0.001). As a percentage of FFM, osseous mineral increased from 2.0 to 3.4% in boys and from 2.1 to 3.3% in girls between 0.5 and 24 mo (p = 0.001).
In addition to the hydration of FFM (Table 4), other parameters commonly used to estimate body composition are summarized in Table 5. TBK differed significantly by age (p = 0.001) and gender (p = 0.04). The potassium content of FFM increased gradually with age (p = 0.001), but no gender effects were seen. Body density showed significant age (p = 0.03) and gender effects (p = 0.01). The density of FFM increased with age (p = 0.001), but showed no significant gender differences. The hydration, potassium content, and density of FFM did not differ by infant feeding mode.
Incremental growth rates partitioned into chemical components are summarized in Table 6. All incremental rates decreased significantly with age (p = 0.001). Overall gender effects were seen for incremental growth rates of FFM, protein, TBW, and minerals (p = 0.02–0.04).
DISCUSSION
This is the first longitudinal study on body composition during the first 2 y of life. We present 1) normative data on FFM and its components, and FM;2) incremental growth rates partitioned into body composition components; and 3) age-specific and gender-specific constants for converting body constituents into FFM for children during the first 2 y of life.
We compared our data with the model published by Fomon et al. (1). Although there are some important differences, the two databases are remarkably similar, considering the paucity of data, the number of assumptions and interpolations used by Fomon et al. We did adopt the same assumptions used by Fomon et al. (1) for the derivation of protein from body potassium, the partitioning of TBW into ICW and ECW based on the potassium concentration of each, and the assumed fixed percentage glycogen content of the body. It is the longitudinal data on TBW, TBK, and BMC for the same population that distinguish our data and allowed us to calculate incremental rates for various body composition compartments.
Birth weight and length of the boys and girls in our CNRC data were similar with those of the Fomon model. Length from 3 mo onwards and weight between 3–12 mo were higher by 1.5% and 4%, respectively, in our CNRC data than for the Fomon model. TBW, on the other hand, was higher by an average of 4% in the Fomon model at 3, 6, 12, 18, and 24 mo in the boys and at 3, 18, and 24 mo in the girls. These discrepancies may be due to the falling drop method used for deuterium measurements, the interpolation of TBW data from 6 mo (68 infants) to age 9 y (11 boys), or an underestimation of deuterium exchange with the exchangeable hydrogen of organic molecules in the Fomon data. Errors in the implementation of the deuterium dilution technique include analytical precision, isotope equilibration within the body, and corrections for exchange of label with nonaqueous hydrogen. The precision of the mass spectrometric determinations of 2H is between 1–2% (9). Theoretical and experimental evidence indicates that deuterium exchange is slightly less than 4% of TBW (9). Fomon used a value of 1.3% to adjust for the exchange of deuterium with the exchangeable hydrogen of organic molecules which would result in 5–6% lower values for FM. TBW may be calculated by the plateau or back-extrapolation approach. Because of the rapidly changing state of the infant at 0.5 mo, we chose to use the plateau approach; thereafter, we used back-extrapolation. In theory, the plateau approach overestimates TBW because only urinary loss of label is accounted for in the equilibration phase, and the back-extrapolation approach underestimates TBW because mixing of the label is not instantaneous. In practice, the two approaches yield similar results in adults (9) and infants (10); measurement errors probably override these theoretical considerations. The discrepancies in TBW are probably not attributable to the use of urine versus plasma specimens. Trowbridge et al. found that urine samples collected 5–7 h post-dose averaged 98.8 ± 2% and 100.7 ± 3.1% of plasma-based TBW values in premature and older infants 6–36 mo (11).
TBK was also, on average, 4% higher in the Fomon model than the CNRC data. In the Fomon model, TBK of 40 6-mo-old infants from the laboratory of Burmeister (12) and of 64 8- to 10-y-old boys from the laboratory of Forbes (13) were used to extrapolate TBK values from birth to 10 y of age. At 6 mo of age, the mean values of TBK were 40.4 and 40.3 mEq/kg body weight compared with our CNRC values of 37.9 and 36.0 mEq/kg body weight for boys and girls, respectively. The Burmeister laboratory used liquid scintillation detectors, whereas we used NaI(Tl) detectors. Liquid scintillation detectors could not completely resolve the background interference photopeak of 137Cs (0.66 MeV) from that of 40K (1.46 MeV). Furthermore, at the time of Burmeister's study, background 137Cs levels were significantly (∼100-fold) higher than present day levels.
BMC values used in the Fomon model exceeded CNRC values by 16% (range −4 to 53%). Approximations of the body content of calcium were based on chemical analysis of the newborn, the calcium content of the femur in older infants (14) and on the ratio of calcium to height in the 9-y-old reference boy (15) in the Fomon model. Our data, of course, depend on the validity of BMC determinations by DXA. The precision and accuracy of our DXA instrument was evaluated using total carcass chemical analysis in piglets (7). DXA-derived BMC was highly correlated with total carcass ash contents (r = 0.982). The mean BMC/ash ratios were 0.73 and 0.64 for software versions 5.56 and 5.57; thus, it appears that the current DXA-derived measure of BMC is within physiologic limits. By weight, BMC contributes minimally to FFM, on the order of 2 to 4%. Therefore, errors in the estimation of BMC contribute less than those of TBW and TBK to the multicomponent model.
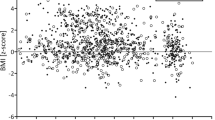
As a result of these differences in the basic components used to predict body composition, our values for FFM were 5% lower than those of the Fomon model. Our values for FM and %FM were 9% higher on average; however, the mean difference can mask the strikingly different patterns of %FM deposition (Fig. 1). Initially at 0.5 mo, %FM is higher in the Fomon model; between 0.5 mo and 3–6 mo we observed an increase in %FM. Thereafter, %FM declines slightly in both databases, but the CNRC values remained significantly higher than those in the Fomon model, except at 9 mo. The different patterns at the younger ages may be attributed to the curve smoothing technique used in the Fomon model. Also, Fomon et al. assumed that percent body fat was proportional to the truncal (flank plus subscapular) skinfold thicknesses reported by McGowan et al. (16) and Karlberg and Taranger (17). A linear relationship between percent body fat and truncal skinfold thickness therefore was assumed and used to derive body fat by interpolation between birth, 6 mo, and 10 y. Others (18) also have reported FM values for infants measured by TOBEC, which were higher than the Fomon model estimates.
It is generally thought that gender differences in FFM are evident from birth throughout childhood, with boys having slightly higher values (19). Between 0.5–18 mo, FFM of the boys was greater than that of the girls, consistent with higher TBW, TBK, and BMC in boys. Gender differences in %FM were seen at 6 and 9 mo, with girls having higher values.
When multiple body composition measurements are not possible or practical, age-specific and gender-specific constants used to convert measured body constituents into FFM in two-compartment models provide a viable alternative. Body composition methods based on TBW by isotope dilution, TBK by whole body counting, and body density by plethysmography require such constants to estimate FFM and FM.
We have provided age-specific and gender-specific constants for converting TBW, TBK, and body density values into FFM. We found that these constants did not differ significantly by gender or feeding mode (data not provided). Using the multicomponent model we did detect significantly lower FFM and higher FM and %FM in breast-fed than formula-fed infants at 3 mo, and higher FM and %FM in breast-fed than formula-fed boys at 6 mo (data to be published elsewhere). It would not be appropriate to present the data segregated by sex-feeding mode because the sample is not sufficient for that purpose. Nonetheless, the sample was equally represented by the two feeding groups and there was significant overlap between feeding groups. The body composition of an individual breast-fed or formula-fed infant would be expected to fall within ± 2 SD from the mean value, since the mean was equally representative of both feeding groups. More important to this application is the observation that the potassium content, hydration, and density of FFM did not differ by feeding mode; therefore, common conversion factors can be used for the two feeding groups in two compartment body composition models. Compared with the Fomon model, our hydration constants of FFM were higher at 0.5 to 9 mo, and thereafter similar (Fig. 2). Our higher hydration values of 82.7 in boys and 83.1% in girls at age 0.5 mo seem more consistent with the value of 83.3% for the reference fetus at 40 wk of gestation (measured by carcass analysis) (20). Our conversion factors for TBK to FFM were lower at 0.5 to 9 mo, and higher at 12 to 24 mo compared with the Fomon model (Fig. 3). Our values for the density of FFM were slightly higher than the Fomon model (Fig. 4). Although these differences are numerically small, propagation of errors through the computation to FFM and FM can result in relevant differences.
These normative body composition data provide an updated reference upon which to assess normal growth and nutritional status of pediatric populations representative of mixed feeding groups during the first 2 y of life. In addition, application of the age-specific and gender-specific constants for converting chemical and physical components into FFM should improve the accuracy of pediatric body composition methodology.
The authors thank the women who participated in this study, and acknowledge the contributions of Carolyn Heinz for study coordination; Marilyn Navarrete for subject recruitment; Sopar Seributra, Sandra Kattner for nursing and dietary support; Maurice Puyau, Firoz Vohra, Roman Shypailo, Judy Joo Posada, JoAnn Pratt, Nitesh Mehta, Zahira Colon, Kiyoko Usuki, Shide Zhang, Deborah Roose for technical assistance; Anne Adolph for data management; Leslie Loddeke for editorial review; and Idelle Tapper for secretarial assistance.















Abbreviations
- FFM:
-
fat free mass
- FM:
-
fat mass
- %FM:
-
percent fat mass
- TBW:
-
total body water
- TBK:
-
total body potassium
- TOBEC:
-
total body electrical conductivity
- DXA:
-
dual energy x-ray absorptiometry
- BMC:
-
bone mineral content
- ECW:
-
extracellular water
- ICW:
-
intracellular water
References
Fomon SJ, Haschke F, Ziegler EE, Nelson SE 1982 Body composition of reference children from birth to age 10 years. Am J Clin Nutr 35: 1169–1175.
Butte NF, Heinz C, Hopkinson JM, Wong WW, Shypailo R, Ellis KJ 1999 Fat mass in infants and toddlers: comparability of total body water, total body potassium, total body electrical conductivity and dual-energy x-ray absorptiometry. J Pediatr Gastroenterol Nutr 29: 184–189.
Wang ZM, Heshka S, Pierson RN, Heymsfield SB 1995 Systematic organization of body-composition methodology: an overview with emphasis on component-based methods. Am J Clin Nutr 61: 457–465.
Wong WW, Lee LS, Klein PD 1987 Deuterium and oxygen-18 measurements on microliter samples of urine, plasma, saliva, and human milk. Am J Clin Nutr 45: 905–913.
Wong WW, Cochran WJ, Klish WJ, Smith EO, Lee LS, Klein PD 1988 In vivo isotope-fractionation factors and the measurement of deuterium- and oxygen-18-dilution spaces from plasma, urine, saliva, respiratory water vapor, and carbon dioxide. Am J Clin Nutr 47: 1–6.
Ellis KJ, Shypailo RJ 1993 Whole-body potassium measurements independent of body size. In: Human Body Composition: In Vivo Methods, Models, and Assessment. Plenum Press, New York, 371–375.
Ellis KJ, Shypailo RJ, Pratt JA, Pond WG 1994 Accuracy of dual energy x-ray absorptiometry for body composition measurements in children. Am J Clin Nutr 60: 660–665.
Heymsfield SB, Wang ZM, Withers RT 1996 Multicomponent molecular level models of body composition analysis. In: Roche AF, Heymsfield SB, Lohman TG (eds) Human Body Composition. Human Kinetics, Champaign, 129–148.
Schoeller DA 1996 Hydrometry. In: Roche AF, Heymsfield SB, Lohman TG (eds) Human Body Composition. Human Kinetics, Champaign, 25–44.
Salazar G, Infante C, Vio F 1994 Deuterium equilibration time in infant's body water. Eur J Clin Nutr 48: 475–481.
Trowbridge FL, Graham GG, Wong WW, Mellits ED, Rabold JD, Lee LS, Cabrera MP, Klein PD 1984 Body water measurements in premature and older infants using H218O isotopic determinations. Pediatr Res 18: 524–527.
Romahn A, Burmeister W 1977 Die Körperzusammensetzung während der ersten zwei Lebensjahre Bestimmungen mit der Kalium-40-Methode. Klin Pädiat 189: 321–327.
Forbes GB 1962 Methods for determining composition of the human body. Pediatrics 29: 477
Christiansen C, Rödbro P, Thöger NC 1975 Bone mineral content and estimated total body calcium in normal children and adolescents. Scand J Clin Lab 35: 507–510.
Christiansen C, Rödbro P 1975 Estimation of total body calcium from the bone mineral content of the forearm. Scand J Clin Lab Invest 35: 425–431.
McGowan A, Jordan M, MacGregor J 1975 Skinfold thickness in neonates. Biol Neonate 25: 66–84.
Karlberg P, Taranger J 1976 The somatic development of children in a Swedish urban community. Acta Paediatr Scand Suppl 258: 1–148.
de Bruin NC, van Velthoven KAM, de Ridder M, Stijnen T, Juttmann RE, Degenhart HJ, Visser HKA 1996 Standards for total body fat and fat-free mass in infants. Arch Dis Child 74: 386–399.
Forbes GB 1987 Human Body Composition. Growth, Aging, Nutrition, and Activity. Springer-Verlag, New York, 1–350.
Ziegler EE, O'Donnell AM, Nelson SE, Fomon SJ 1976 Body composition of the reference fetus. Growth 40: 329–341.
Author information
Authors and Affiliations
Additional information
This work is a publication of the US Department of Agriculture/Agricultural Research Service (USDA/ARS) Children's Nutrition Research Center, Department of Pediatrics, Baylor College of Medicine and Texas Children's Hospital, Houston, Texas.
This project was funded in part with federal funds from the USDA/ARS under Cooperative Agreement 58–6250-6001.
The contents of this publication do not necessarily reflect the views or policies of the USDA, nor does mention of trade names, commercial products, or organizations imply endorsement by the US Government.
Rights and permissions
About this article
Cite this article
Butte, N., Hopkinson, J., Wong, W. et al. Body Composition during the First 2 Years of Life: An Updated Reference. Pediatr Res 47, 578–585 (2000). https://doi.org/10.1203/00006450-200005000-00004
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200005000-00004
This article is cited by
-
Infant growth and body composition from birth to 24 months: are infants developing the same?
European Journal of Clinical Nutrition (2024)
-
Adiposity and feeding practices in the first two years of life among toddlers in Guadalajara, Mexico
BMC Pediatrics (2023)
-
Body composition from birth to 2 years
European Journal of Clinical Nutrition (2023)
-
Differential associations between body composition indices and neurodevelopment during early life in term-born infants: findings from the Pakistan cohort: Multi-Center Body Composition Reference Study
European Journal of Clinical Nutrition (2023)
-
Body composition of infants at 6 months of age using a 3-compartment model
European Journal of Clinical Nutrition (2023)