Abstract
Background
Associations among body composition measures have been limited to cross-sectional analyses of different subjects. We identified cross-sectional relationships between body mass index (BMI) and other body composition measures and predicted body composition measures from BMI throughout childhood and adolescence.
Methods
BMI was calculated and % body fat (%BF), fat mass index (FMI), and fat-free mass index (FFMI) were measured using dual-energy x-ray absorptiometry at ages 5, 9, 11, 13, 15, and 17 years in a birth cohort (n = 629). Sex-specific body composition measures were calculated for BMI-for-age percentiles; associations between BMI and body composition measures were characterized; and body composition measures were predicted from BMI.
Results
%BF, FMI, and FFMI generally increased with BMI-for-age percentiles at each age. Correlations between BMI and %BF or FMI were generally higher at BMI-for-age percentiles ≥95% than for lower BMI-for-age percentiles. Correlations between BMI and FFMI were generally higher for participants at very low and very high BMI-for-age percentiles than at moderate BMI-for-age percentiles. Age- and sex-specific predictions from BMI are provided for %BF, FM, and FFMI.
Conclusions
Sex-specific body composition measures throughout childhood and adolescence are presented. BMI is a better indicator of adiposity at higher than at lower BMI values.
Impact
-
Sex-specific body composition measures throughout childhood and adolescence are described.
-
% BF, FMI, and FFMI generally increased with BMI-for-age percentiles for both sexes throughout childhood and adolescence.
-
BMI is a better indicator of adiposity at higher BMI levels than at lower BMI values throughout childhood and adolescence.
Similar content being viewed by others
Introduction
Obesity is a disease characterized by “abnormal or excessive fat accumulation that presents a risk to health” according to the World Health Organization (WHO),1 and is defined as “having a body mass index (BMI) at or above the 95th percentile” according to the Centers for Disease Control and Prevention (CDC).2 Childhood obesity is a significant risk factor for adult obesity with ~60% of obese children becoming obese adults, although most obese adults were not obese children.3 Both childhood and adult obesity are associated with significant social and economic disadvantages in addition to premature morbidity and mortality.4,5,6
Childhood obesity is typically identified and monitored using either the WHO’s or CDC’s growth standards for weight-for-age or BMI-for-age.7,8 BMI (weight/height2) is an indirect measure of body fat previously associated with direct measures of body fat assessed by skinfold thicknesses, bioelectrical impedance, and dual-energy x-ray absorptiometry (DXA). Direct measures of body fat include % body fat (%BF) and the fat mass index (FMI). Neither weight nor BMI can distinguish between fat and fat-free mass, leading to misclassification of individuals having a high proportion of either fat or fat-free mass. While the %BF enables identification of relative body fat, it does not account for variation in lean mass or adjust for body height. Van Itallie et al.9 proposed normalizing both fat mass and fat-free mass for height2 (FMI and FFMI, respectively) to better identify body composition and classify obesity.10 Freedman et al.11 identified FMI and FFMI values, and investigated relationships among FMI and FFMI according to BMI-for-age percentiles in youth aged 5–18 years, clearly indicating that BMI is a more sensitive indicator of obesity at higher BMI levels. Subsequently, sex-specific reference percentiles for %BF, FMI, and FFMI for children and adolescents using data from the 1999–2004 National Health and Nutrition Examination Study were developed for all children and specific racial and ethnic groups.12,13,14
Regardless of its limitations, BMI is used in clinic and research due to its relative simplicity, low cost, and feasibility. Understanding associations between BMI and other body composition measures of adiposity throughout childhood and adolescence is necessary to improve clinical identification of childhood obesity and facilitate research investigating the development of obesity. Previous investigation of associations between BMI and other body composition measures of adiposity have been cross-sectional, with different subjects investigated at different ages. Our objectives were to describe sex-specific relationships between BMI and %BF, FMI, and FFMI at approximate ages 5, 9, 11, 13, 15, and 17 years in a birth cohort (i.e., repeated measures on the same participants, instead of measures on different groups of participants at different ages), and to fit models to predict sex-specific %BF, FMI, and FFMI from BMI at each age.
Methods
Design
Cross-sectional analyses were conducted on data collected as part of the Iowa Fluoride Study (IFS) and Iowa Bone Development Study (IBDS), a sub-study of the IFS.15,16,17,18,19 The IFS and IBDS investigated relationships among fluoride exposures, dietary intakes, oral health, and bone health. The IFS/IBDS is registered at Clinical Trials.gov: NCT03547128; https://clinicaltrials.gov/ct2/show/NCT03547128. Data obtained from anthropometric measures and DXA scans completed at clinic visits when children were approximately age 5, 9, 11, 13, 15, and 17 years were used in the current analyses. Subjects were invited to participate in clinic exams shortly before the target birthday; actual exams were scheduled at the subject’s convenience considering parent availability for travel, school conflicts, vacations, extracurricular activities, etc.; DXA machine availability; and staffing availability. The mean (25th, 75th) ages at scan are presented in Table 1. Family demographic information was obtained at birth (1992–1995) by questionnaire. Household income and mother’s education at baseline were used to define three tiers of socioeconomic status (SES). Low SES was defined by a baseline household income <$30,000 and maternal education below a 4-year college degree. Moderate SES was defined by a household income <$30,000 and a maternal education equivalent to a 4-year college degree or higher, or a household income of $30,000–$49,999 and a maternal education below a graduate or professional degree. High SES was defined by a household income of $30,000–$49,999 and a maternal education equivalent to a graduate or professional degree or a household income of $50,000 or more.18
Participants
Mothers (n = 1882) were recruited at the time of their child’s birth for participation in the IFS, and IFS participants active at age 5 years (~800 participants) were invited to participate in the IBDS. Inclusion in the current analyses (n = 629) required participation in at least one of six possible DXA scans. All components of the IFS and IBDS were approved by the Institutional Review Board at the University of Iowa. Written informed consent was obtained from mothers at the time of their child’s birth and from parents at clinic visits. Written assent was obtained from children beginning at age 13 years.
Anthropometric measures
Weight (Continental scale, Bridgeview, IL, USA) and height (Harpenden stadiometer, Holtain, UK) were measured by trained and calibrated research nurses during clinic visits.18,19 BMI, an indirect measure of body fat, was calculated as weight/height2 (kg/m2).20
DXA scans
DXA, which directly measures body fat, was used to estimate fat mass. Scans were completed by one of three experienced research technicians to minimize operator-related variability in the General Clinical Research Center at the University of Iowa using standard positioning.16,17 Whole-body scans at ages 5 and 9 years were completed using a Hologic QDR 2000 model with software version 7.20B and fan-beam mode. Whole-body scans at ages 11, 13, 15, and 17 years were completed using Hologic QDR 4500 with software version 12.3 or 12.4 and fan-beam mode (Hologic, Waltham, MA). Because the Hologic QDR 4500 underestimates fat mass and overestimates lean mass, age 11, 13, 15, and 17 scans were re-analyzed using the NHANES assessment algorithms.21
Percent body fat (%BF) was calculated as total fat mass/body mass × 100. FMI was calculated as total fat mass/height2 (kg/m2). FFMI was calculated as (total mass − fat mass)/height2 (kg/m2).
Statistical analyses
Descriptive statistics were calculated for sex-specific anthropometric measures (weight and height) and body composition measures (BMI, %BF, FMI, and FFMI) at each scan age.
Sex-specific means for other body composition measures were calculated for participants grouped by BMI-for-age percentiles at each scan age using standards published by the CDC.22 Spearman’s correlation coefficients were used to characterize associations between BMI and other body composition measures for participants grouped by BMI-for-age percentiles at each scan age.
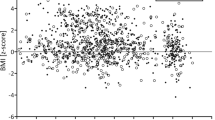
Sex-specific, generalized additive models were fit using BMI to predict %BF, FMI, or FFMI at each target scan age. Instead of using linear regression models, which describe the association between predictor variables (BMI) and an outcome variable (%BF, FMI, or FFMI) assuming a linear relationship, generalized additive models allow the mean of the outcome variable to depend on a smooth, curvilinear function of the predictor variable. This modeling framework was necessary to accommodate the non-linear associations between BMI and each of the other body composition measures.
A spline-based smoothed function with a basis dimension of 3 was used to characterize the relationship between the mean outcome and BMI in each generalized additive model. Adjusted for the mean, each outcome variable was assumed to be approximately normally distributed. These models were fit using the mgcv package in R version 4.0.0.23,24 After fitting the generalized additive models, the expected value of the outcome variable over the range of observed BMI values was plotted and the raw data were overlaid on this curve.
In addition, 95% prediction intervals at select BMI values of interest were plotted. Prediction intervals provide an uncertainty range for future observations, unlike confidence intervals that provide an uncertainty range for the expected value of the outcome variable. These prediction intervals were calculated using a bootstrap procedure.25 The bootstrap is a flexible resampling technique that can be used to produce prediction and confidence intervals with minimal distributional or sample-size assumptions.
Results
The majority of participants were female (51%) and non-Hispanic white (94%). Considering household income and maternal education at birth, 26%, 36%, and 38% of participants belonged to low, middle, and high SES categories, respectively. Anthropometric and body composition measures are summarized in Table 1. As expected, weight, height, and BMI increased with age. Both %BF and FMI generally increased with age in females, while they increased during childhood and then decreased during adolescence in males. FFMI generally increased with age for both males and females, although the increase was more pronounced in males than in females.
Body composition measures according to BMI-for-age percentiles are provided in Table 2. Mean %BF, FMI, and FFMI generally increased with BMI-for-age percentiles for both males and females at each scan age, and for a given BMI-for-age percentile, both %BF and FMI were notably higher in females than males, especially at older ages. Associations between BMI and other body composition measures after grouping participants according to BMI-for-age percentiles are provided in Table 3. Correlation coefficients between BMI and %BF or FMI were generally higher at BMI-for-age percentiles ≥95% for males (%BF r = 0.52–0.87 and FMI r = 0.80–0.95) and ≥75% for females (%BF r = 0.53–0.76 and FMI r = 0.70–0.93) compared to lower BMI-for-age percentiles. BMI generally had higher correlation coefficients with FFMI for participants at very low and very high BMI-for-age percentiles (<25% and ≥95%) relative to participants with more moderate BMI-for-age percentiles.
Sex-specific body composition measures estimated for select BMIs at each scan age with accompanying 95% prediction intervals are presented in Table 4. Figs. 1–6 present sex-specific plots visually displaying the results from the fitted generalized additive regression models (i.e., the expected value of the outcome variable across the range of observed BMI values) and corresponding prediction intervals at relevant ages for BMI predicting %BF, FMI, and FFMI. These figures allow for visual inspection of how the expected value of each body composition measure changes with BMI. Prediction intervals demonstrate the predicted range of values for new observations relative to the regression curve. While the models adequately track the mean %BF, FMI, or FFMI values over the BMI values, the predictions are characterized by considerable uncertainty, as reflected in the wide prediction intervals presented in Table 4 and the online figures.
Discussion
Herein, we report age 5- to 17-year body composition measures and associations between BMI and %BF, FMI, and FFMI in a cohort followed longitudinally from birth. The results complement previous cross-sectional investigations of body composition measures in similar aged populations.11,12
The mean BMI, FMI, and FFMI of IFS/IBDS participants were similar to those reported for white participants of the Pediatric Rosetta Body Composition Project aged 5–11 and 12–18 years.11 However, the median FMI of IFS/IBDS participants was slightly lower and the FFMI slightly higher than the age- and sex-specific FMI and lean (i.e., fat-free tissue excluding bone) mass index reference percentiles developed by Weber et al.12 using 1999–2004 NHANES data.
Sex-specific overall associations between BMI and FMI (r = 0.93–0.97) reported by Freedman et al.11 are similar to those observed in IFS/IBDS participants; however, associations between BMI and FFMI (r = 0.64–0.76) in both male and female subjects are lower than those observed in IFS/IBDS subjects. Consistent with results reported herein, associations between BMI and FMI were higher at ≥85% BMI for age than at <85% BMI for age.11 Weber et al.12 reported a stronger positive predictive value using BMI to identify obese (98%) than to identify overweight (62%) children as defined by FMI in non-Hispanic whites. Furthermore, the positive predictive value of BMI to identify either overweight or obesity was higher when using FMI to define definitive obesity compared to %BF.12 These reports are consistent with the results reported herein; associations between BMI and FMI had a higher Spearman correlation coefficient both overall and for participants whose BMI exceeded the ≥95% BMI for age than associations between BMI and %BF.
Weight and height measurements are relatively noninvasive and simplistic, and often are used to track growth throughout childhood.26 Weight includes both fat and fat-free mass. However, weight for age and BMI for age will always have limited abilities to distinguish between excessive adipose tissue and excessive lean mass in overweight and obese individuals. Understanding associations between BMI and other body composition measures of adiposity is relevant for clinical practice. Estimating patient’s potential risk of obesity based on BMI combined with knowledge of the patient’s behavioral risk factors will enable clinicians to offer more individualized behavioral recommendations and anticipatory guidance to reduce the risk of obesity for the patient.
The longitudinal IFS and IBDS offer a unique opportunity to develop sex- and age-specific models to predict body composition from BMI using a single cohort, thus enabling a better understanding of adipose (%BF or FMI) and lean (FFMI) tissue distributions at a given BMI. Regardless of apparent limitations, the fitted models appear to provide reasonable estimates of mean %BF, FMI, and FFMI from BMI during childhood and adolescence, but are probably not sufficient to predict individual values due to the inherent variability in the outcomes. Incorporating additional information about participant lifestyle or other factors into the generalized additive models might help narrow the prediction intervals and reduce prediction uncertainty in our models.
Participants in the IFS and IBDS are primarily Caucasian, which limits the generalizability of the results to other racial and ethnic populations. Furthermore, the subjects are from reasonably wealthy and well-educated households that likely provided adequate nutrition and housing throughout childhood. Thus, the results are not generalizable to subjects raised in food-insecure households with limited or inconsistent access to adequate nutrition. Strengths of the study include repeated measures of participants from early childhood throughout adolescence. Although our study benefits from having a long period of follow-up, this long follow-up was accompanied by changes in technology. The changes in DXA machines between ages 9 and 11 is another limitation of our study.
Conclusions
Sex-specific body composition measures throughout childhood and adolescence are described. Evaluation of associations between BMI and body composition measures confirm that BMI is a better indicator of adiposity at higher BMI levels than at lower BMI values. Age- and sex-specific estimates and corresponding prediction intervals are provided for the prediction of %BF, FM, and FFMI from BMI.
References
World Health Organization. Obesity (accessed 18 December 2019); https://www.who.int/topics/obesity/en/.
Centers for Disease Control and Prevention. Defining Childhood Obesity (accessed 18 December 2019); https://www.cdc.gov/obesity/childhood/defining.html.
Simmonds, M., Llewellyn, A., Owen, C. G. & Woolacott, N. Predicting adult obesity from childhood obesity: a systematic review and meta-analysis. Obes. Rev. 17, 95–107 (2016).
Kelly, A. S. et al. on behalf of the American Heart Association Atherosclerosis, Hypertension, and Obesity in the Young Committee of the Council on Cardiovascular Disease in the Young, Council on Nutrition, Physical Activity and Metabolism, and Council on Clinical Cardiology. Severe obesity in children and adolescents: identification, associated health risks, and treatment approaches. A Scientific Statement from the American Heart Association. Circulation 2128, 1689–1712 (2013).
Schvey, N. A. et al. Weight-based teasing is associated with gain in BMI and fat mass among children and adolescents at-risk for obesity; a longitudinal study. Pediatr. Obes. 14, e12538 (2019).
Pearl, R. L. et al. Everyday discrimination in a racially diverse sample of patients with obesity. Clin. Obes. 8, 140–146 (2018).
World Health Organization. Obesity and Overweight (accessed 18 December 2019); https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight.
Centers for Disease Control and Prevention. CDC Growth Charts (accessed 18 December 2019); https://www.cdc.gov/growthcharts/cdc_charts.htm.
VanItallie, T. B., Yang, M. U., Heymsfield, S. B., Funk, R. C. & Boileau, R. A. Height-normalized indices of the body’s fat-free mass and fat mass: potentially useful indicators of nutritional status. Am. J. Clin. Nutr. 52, 953–959 (1990).
Wells, J. C. K. A critique of the expression of paediatric body composition data. Arch. Dis. Child. 85, 67–72 (2001).
Freedman, D. S. et al. Relation of BMI to fat and fat-free mass among children and adolescents. Int. J. Obes. 29, 1–8 (2005).
Weber, D. R., Moore, R. H., Leonard, M. B. & Zemel, B. S. Fat and lean BMI reference curves in children and adolescents and their utility in identifying excess adiposity compared with BMI and percentage body fat. Am. J. Clin. Nutr. 98, 49–56 (2013).
Duran, I. et al. Reference centiles for the evaluation of nutritional status in children using body fat percentage, fat mass and lean bod mass index. J. Clin. Densitom. 23, 349–363 (2020).
Ogden, C. L., Li, Y., Freedman, D. S., Borrud, L. G. & Flegal, K. M. Smoothed percentage body fat percentiles for US children and adolescents, 1999-2004. Natl Health Stat. Rep. 9, 1–7 (2011).
Warren, J. J., Levy, S. A. & Kanellis, M. J. Dental caries in the primary dentition: assessing prevalence of cavitated and noncavitated lesions. J. Public Health Dent. 62, 109–114 (2002).
Janz, K. F. et al. Physical activity augments bone mineral accrual in young children: the Iowa Bone Development study. J. Pediatr. 148, 793–799 (2006).
Janz, K. F. et al. Physical activity, not sedentary time, predicts DXA-measured adiposity age 5-19 years. Med. Sci. Sports Exerc. 49, 2071–2077 (2017).
Marshall, T. A., Curtis, A. M., Cavanaugh, J. E., Warren, J. J. & Levy, S. M. Child and adolescent sugar-sweetened beverage intakes are longitudinally associated with higher body mass index z scores in a birth cohort followed 17 years. J. Acad. Nutr. Diet. 119, 425–434 (2019).
Marshall, T. A. et al. Description of child and adolescent beverage and anthropometric measures according to adolescent beverage patterns. Nutrients 25, https://doi.org/10.3390/nu10080958 (2018).
Centers for Disease Control and Prevention. Body Mass Index (BMI) (accessed 18 December 2019); https://www.cdc.gov/healthyweight/assessing/bmi/index.html.
National Center for Health Statistics. National Health and Nutrition Examination Survey: NHANES 1999-2000 Documentation, Codebook, and Frequencies: Dual-Energy X-Ray Absorptiometry 2008 (accessed 18 December 2019); https://wwwn.cdc.gov/nchs/data/nhanes/dxa/dxx.pdf.
Centers for Disease Control and Prevention. Growth Chart Training: A SAS Program for the 2000 CDC Growth Charts (ages 0-<20 years) (US Department of Health and Human Services, accessed 1 April 2020); https://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm.
R Core Team. R: A Language and Environment for Statistical Computing (R Foundation for Statistical Computing, 2020).
Wood, S. N. Generalized Additive Models: An Introduction with R 2nd edn. (Chapman & Hall/CRC, 2017).
Efron, B. & Tibshirani, R. An Introduction to the Bootstrap (Chapman & Hall/CRC, 1993).
Cole, T. J., Faith, M. S., Pietrobelli, A. & Heo, M. What is the best measure of adiposity change in growing children: BMI, BMI%, BMI z-score or BMI centile? Eur. J. Clin. Nutr. 59, 419–425 (2005).
Acknowledgements
The study was supported by the National Institutes of Health (R03-DE023784, R01-DE12101, R01-DE09551, UL1-RR024979, UL1-TR000442, UL1-TR001013, M01-RR00059), The Roy J. Carver Charitable Trust, and Delta Dental of Iowa Foundation.
Author information
Authors and Affiliations
Contributions
T.A.M. conceptualized and designed the study, interpreted the results, drafted the initial manuscript, and reviewed and revised the manuscript. A.M.C. designed and conducted the data analyses, interpreted the results, drafted the initial manuscript, and reviewed and revised the manuscript. J.E.C. designed the data analyses, interpreted the results, and reviewed and revised the manuscript. J.J.W. and S.M.L. designed the data collection instruments, collected data, and critically reviewed the manuscript. All authors approved the final manuscript as submitted and agree to be held accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent statement
All components of the IFS and IBDS were approved by the Institutional Review Board at the University of Iowa. Written informed consent was obtained from mothers at the time of their child’s birth and from parents at clinic visits. Written assent was obtained from children beginning at age 13 years.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Marshall, T.A., Curtis, A.M., Cavanaugh, J.E. et al. Associations between body mass index and body composition measures in a birth cohort. Pediatr Res 91, 1606–1615 (2022). https://doi.org/10.1038/s41390-021-01562-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-021-01562-y