Abstract
Immunotherapy is associated with durable clinical benefit in patients with melanoma. The goal of this article is to provide evidence-based consensus recommendations for the use of immunotherapy in the clinical management of patients with high-risk and advanced-stage melanoma in the USA. To achieve this goal, the Society for Immunotherapy of Cancer sponsored a panel of melanoma experts—including physicians, nurses, and patient advocates—to develop a consensus for the clinical application of tumour immunotherapy for patients with melanoma. The Institute of Medicine clinical practice guidelines were used as a basis for this consensus development. A systematic literature search was performed for high-impact studies in English between 1992 and 2012 and was supplemented as appropriate by the panel. This consensus report focuses on issues related to patient selection, toxicity management, clinical end points and sequencing or combination of therapy. The literature review and consensus panel voting and discussion were used to generate recommendations for the use of immunotherapy in patients with melanoma, and to assess and rate the strength of the supporting evidence. From the peer-reviewed literature the consensus panel identified a role for interferon-α2b, pegylated-interferon-α2b, interleukin-2 (IL-2) and ipilimumab in the clinical management of melanoma. Expert recommendations for how to incorporate these agents into the therapeutic approach to melanoma are provided in this consensus statement. Tumour immunotherapy is a useful therapeutic strategy in the management of patients with melanoma and evidence-based consensus recommendations for clinical integration are provided and will be updated as warranted.
Similar content being viewed by others
Introduction
The incidence of cutaneous melanoma has increased steadily since the 1970s, with over 70,000 new cases of invasive melanoma in the USA each year costing close to US$2 billion annually.1 Early detection and wide excision is associated with 5-year survival rates of >90% and 80% for stage I and II lesions, respectively.2 Survival decreases to 50% for patients with localized lymph-node metastases (stage III), and metastatic disease (stage IV) historically had a median survival of 8–9 months and a 3-year overall survival rate less than 15%.3 Prior to 2011, treatment of melanoma was limited to interferon-α2b for adjuvant therapy and dacarbazine or high-dose interleukin-2 (IL-2) for metastatic disease. Since 2011, three new agents have been approved for the treatment of patients with melanoma: pegylated-interferon-α2b in the adjuvant setting, the anti-CTLA4 monoclonal antibody ipilimumab for metastatic disease and an oral BRAF inhibitor vemurafenib in patients with metastatic melanoma harbouring BRAFV600 mutations.4,5,6
Tumour immunotherapy is the clinical application of pharmacological agents that directly induce or substitute for host antitumour immunity. Melanoma can be highly sensitive to immunotherapy and of the six approved drugs highlighted above only dacarbazine and vemurafenib are not immunotherapies. The mechanism of action for most immunotherapeutic agents remains incompletely understood, but these treatments are notable for their ability to produce a durable benefit in a subset of patients.7,8 Ipilimumab has been associated with significant improvement in overall survival in the metastatic setting.5,9 Immunotherapy requires special attention to several caveats. Although therapeutic benefits can be durable, only a subset of patients respond.7,8 In addition, unique adverse effects of immunotherapy, many of which relate to the induction of autoimmunity and pro-inflammatory-like states,10 might limit eligibility or become challenges in clinical management. Recent studies suggest immunotherapy, particularly with ipilimumab and related agents, might result in tumour regression over a prolonged time, based on the kinetics of establishing an effective host antitumour immune response.10,11 This finding has led to the development of immune-related response criteria to better monitor patients treated with immunotherapy and to determine appropriate clinical end points.12 Availability of non-immunotherapy strategies has also resulted in the opportunity to develop combination treatment regimens for clinical evaluation and the need to better define optimal sequencing of therapy for patients with advanced-stage melanoma.
The Society for Immunotherapy of Cancer (SITC) is a non-profit professional organisation dedicated to the basic understanding and clinical applications of tumour immunotherapy. To provide guidance to practicing clinicians caring for patients with melanoma, SITC established a Melanoma Clinical Immunotherapy Guidelines panel (Supplementary Box 1 online). The panel consisted of melanoma experts, including physicians, nurses and patient advocates and considered issues related to patient selection, toxicity management, treatment cessation guidelines and current recommendations for treatment sequencing with the goal of preparing a consensus statement on clinical use of tumour immunotherapy for patients with melanoma.
Methods
Consensus statement policy
The Institute of Medicine's March 2011 Standards for Developing Trustworthy Clinical Practice Guidelines13 served as a model for organising and preparing this consensus statement. These standards include establishing a transparent process for guideline development and funding, managing and reporting conflicts of interest, inclusion of a multidisciplinary and balanced group composition, establishing an evidence-based foundation and rating system for the strength of the evidence, reporting the results through a peer-reviewed publication and publicly available website, and having a plan for updating the statement as changes in the field warrant revisions. Convening under the umbrella of SITC (June 2011), a steering committee led a panel, which sought to develop clinical treatment guidelines considering four basic issues for each immunotherapy agent in current clinical practice: patient selection, toxicity management, assessment of response, and therapy sequencing and combinations. This consensus statement is not intended to substitute for the individual professional judgement of the treating physician. Full consensus recommendations can be found on the SITC website.14 Owing to disparities in drug approval and availability in some countries, this panel focused solely on drugs approved by the FDA for the treatment of patients in the USA. An advance copy of this manuscript was submitted to the FDA for comment before submission for publication.
Consensus panel and conflicts of interest
Potential panel members were solicited from SITC members and non-member melanoma multidisciplinary experts, clinicians and populations in the USA expected to be affected by the development of any recommendations, including patients, patient advocates and nurses. Panel members were screened for conflicts of interest using the SITC disclosure form, which mandates full financial and other disclosures including relationships with commercial entities that might reasonably be expected to have direct regulatory or commercial impact resulting from the publication of this statement. Disclosures of potential conflicts of interest are noted in this manuscript and in detail online. No commercial funding was used in supporting the consensus panel, literature review or preparation of the manuscript.
The consensus panel convened in June 2011 in accordance with the Institute of Medicine and SITC guidelines to review results from a previously distributed questionnaire collecting information on the participants' role in the care of patients with melanoma, primary clinical focus, experience with FDA-approved agents used for immunotherapy treatments, and current practices in the use or recommendation for use of such agents. Additional questionnaires were distributed after the meeting to collect further information. The final consensus statement was made available to the entire SITC membership for open comment and these comments were considered for the final manuscript and are available in Supplementary Box 2 online.
Literature review
A search of the scientific literature (using the MEDLINE database) was conducted focusing on current therapeutic approaches in humans. The search terms were: “melanoma and interferon”, “melanoma and interleukin-2”, “melanoma and ipilimumab”, “melanoma and vemurafenib”, “melanoma and dacarbazine”, and “melanoma and temozolomide”), which resulted in a 986-item (duplicates removed) bibliography (Supplementary Bibliography online) catalogued using EndNote X5.0.1. The bibliography was supplemented with additional literature identified by the panel, as appropriate. Literature was graded into three levels according to levels of evidence (Box 1). Level A represented strong supporting evidence-based data as derived from appropriately powered prospective, randomized clinical trials and meta-analyses. Level B represented moderate supporting data as derived from uncontrolled, prospective clinical trials. Level C represented weak supporting data as derived from retrospective reviews and case reports.
Consensus recommendations
Immunotherapy for stage II melanoma
Clinical question: What is the appropriate use of immunotherapy in the treatment of stage II melanoma?
Initial assessment
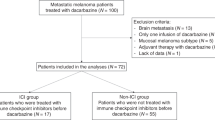
Patients with stage II melanoma have an excellent overall survival of 80% or better provided the tumour is treated by complete resection.2 A subset of tumours characterized as deep (depth of >4 mm), with ulceration or possibly those with a high tumour mitotic rate (≥1 per mm2), are considered high risk for recurrence.15 The panel recommends that all stage II patients have a comprehensive diagnostic workup and be reviewed by a multidisciplinary team (surgical oncologist, medical oncologist and dermatopathologist) to accurately determine tumour stage and risk of melanoma recurrence. This workup should include sentinel-lymph-node biopsy, when appropriate.3,16 There is general agreement that patients with low-risk stage II melanoma can be safely observed and do not warrant treatment (Figure 1).
All treatment options shown may be appropriate, and final selection of therapy should be individualized based on patient eligibility and treatment availability at the physician's discretion. These algorithms represent consensus sequencing suggestions by the panel. (1) High-risk disease is defined as tumours >4 mm in diameter, ulcerated, and/or mitotic rate ≥1 per mm2. There is limited consensus on adjuvant therapy for this group with 43% of the panel recommending interferon-α2b, 38% recommending observation, 14% recommending clinical trial participation and no panellists recommending pegylated-interferon-α2. A minority (5%) recommended individualizing treatment for each patient. (2) There is no evidence that immunotherapy is useful in patients with low-risk stage II melanoma. (3) Patients should have a good performance status without evidence of significant depression, psychiatric history or underlying autoimmune disease to be considered for interferon-α2b. There are limited data available on interferon-α2b as treatment for stage II disease. (4) Clinical trials might be the preferred treatment recommendation for patients with stage II disease if they are available. Protocol-specific eligibility would need to be followed to appropriately select patients.
Consensus management of stage II melanoma
The panel is divided on the role of immunotherapy for patients with high-risk stage II melanoma (Figure 1) and recognizes the limited level A data available to inform clinical decision-making. The majority of the panel recommends that high-risk patients be treated with standard 1-year interferon-α2b, although a minority suggest participation in clinical trials (assuming availability and eligibility to the protocol-specific patient selection criteria of the trial) or observation. A few panellists (5%) individualize treatment of patients with high-risk stage II melanoma based on the particular situation. None of the panel members recommends treatment with pegylated-interferon-α2b for patients with high-risk stage II disease. Patients with high-risk stage II melanoma who are treated with interferon-α2b should have a good performance status without evidence of significant depression or psychiatric history or underlying autoimmune disease. In addition, patients with high-risk disease receiving interferon-α2b should cease treatment when unmanageable adverse effects persist despite dose reduction of 67–75%, at the time of documented disease recurrence or after 1 year of therapy. Patients with high-risk melanoma who are enrolled in a clinical trial follow the course of treatment and treatment cessation dictated by the trial protocol.
Literature review and analysis
Limited data exist on the role of immunotherapy for low-risk stage II melanoma, but there have been several randomized clinical trials focusing on patients with high-risk stage II disease. A prospective study of 499 patients with melanoma depth >1.5 mm and without clinically detectable lymph-node metastases who were randomly assigned to 18 months of subcutaneous interferon-α2b or observation demonstrated a significant improvement in relapse-free survival (P = 0.038) and a clear trend toward improved overall survival (P = 0.059) for patients who received adjuvant interferon-α2b.17 In another trial, 855 patients were randomly assigned to observation or 4 weeks induction interferon-α2b followed by 1 or 2 years of interferon-α2b maintenance therapy.18 That trial reported an improvement in relapse-free survival for patients who received 1 year of maintenance interferon-α2 (hazard ratio [HR] = 0.77, 95% CI 0.63–0.96; P = 0.034), but no benefit in overall survival (HR = 0.91, 95% CI 0.74–1.10; P = 0.642). Several other prospective randomized trials examined interferon-α2b at a variety of doses and treatment schedules in patients with high-risk stage II melanoma, but none has demonstrated a survival benefit.19,20,21,22 These studies are complicated by a lack of a standardized definition of 'high-risk',23 different interferon-α2b doses and schedules, and in some cases include other drugs in combination.
Immunotherapy for stage III melanoma
Clinical question: What is the appropriate use of immunotherapy in the treatment of stage III melanoma?
Initial assessment
Stage III represents a heterogeneous group of patients with 5-year survival rates ranging from 30% to 80%.3 In patients with stage lll melanoma, a diagnostic workup should be performed and reviewed by a multidisciplinary team for patient and tumour characteristics. Complete tumour staging information should be assessed, including pathological features of the primary tumour and any involved lymph nodes, whole-body imaging, serum lactate dehydrogenase (LDH) levels and performance status assessment. Nodal status should be determined based on physical examination, sentinel-lymph-node biopsy and/or lymphadenectomy status. The consensus panel identified two immunotherapy agents with potential clinical benefit in the adjuvant therapy of patients with stage III melanoma: interferon-α2b and pegylated-interferon-α2b.4,24,25,26,27
Consensus management of microscopic nodal disease
The panel recognized that patients with microscopically involved lymph nodes (N1a disease) might represent a different population than those with macroscopic nodal disease (N1b and N2–N3 disease). A majority (52.2%) of the panel recommends a standard 1-year course of interferon-α2b for the adjuvant therapy of microscopic nodal disease. A minority (21.7%) recommends shorter-course interferon-α2b, biochemotherapy generally consisting of cisplatin, vinblastine, dacarbazine, low-dose IL-2 and interferon-α2b (4.3%) or no further treatment (observation; 21.7%). When specifically asked, all panellists recommend that these patients consider enrolling in appropriate clinical trials, but no panellists recommend pegylated-interferon-α2b (Figure 2). There is one prospective randomized clinical trial demonstrating a benefit in relapse-free survival for patients with microscopic nodal disease treated with pegylated-interferon-α2b.4 A post-hoc analysis of that trial also suggested patients with ulcerated primary tumours might derive more clinical benefit from pegylated-interferon-α2b.28 In this analysis, patients with ulceration of their primary melanoma (n = 849) were compared to patients without ulceration of their primary melanoma (n = 1,336), and patients with ulceration demonstrated a significant improvement in relapse-free survival (P = 0.02), distant metastasis-free survival (P <0.001) and overall survival (P <0.001). The analysis also found that the greatest reduction in risk was seen in patients with ulcerated primary melanomas who were classified as stage IIb–III-N1, demonstrating an HR of 0.58 for overall survival benefit (P <0.0001). Thus, patients with ulcerated primary tumours and those with microscopic nodal disease could consider pegylated-interferon-α2b based on level B data.
All treatment options shown may be appropriate and final selection of therapy should be individualized based on patient eligibility and treatment availability at the physician's discretion. These algorithms represent consensus sequencing suggestions by the panel. (1) There are limited data on the role of adjuvant therapy following sentinel lymphadenectomy alone. (2) There are level B data to support a benefit in RFS for pegylated-interferon-α2b in patients with N1a disease and in patients with ulceration of the primary tumour site. The majority of the panel does not consider pegylated-interferon-α2b at all (52.4%), whereas a minority considers it for N1a disease (14.3%) or in the setting of an ulcerated primary lesion (14.3%). Some panel members will consider pegylated-interferon-α2b when patients are not willing or able to tolerate standard interferon-α2b (9.5%). (3) There are level A data that 1 year interferon-α2b is associated with improvement in RFS and it was generally recommended by the consensus panel. Abbreviations: LDH, lactate dehydrogenase; NCCN, National Comprehensive Cancer Network; RFS, recurrence-free survival.
Consensus management of macroscopic nodal disease
Patients with macroscopic nodal disease (N1b and N2–N3 disease) are at increased risk for melanoma recurrence and the panel generally recommends these patients consider 1 year of interferon-α2b treatment (72.7%). A minority of the panel mentioned a shorter course of interferon-α2b (9.1%), observation (9.1%), adjuvant radiation therapy (4.5%) and biochemotherapy (4.5%). No panellists recommend pegylated-interferon-α2b for patients with resected macroscopic nodal disease. Based on the consensus and literature review, which includes several meta-analyses of clinical outcomes for interferon-α2b,29,30,31 the panel considered there was level A data supporting the use of interferon-α2b in these patients (Figure 2). Participation in appropriate clinical trials was considered to be an acceptable alternative.
Other considerations
The panel also suggests that treating physicians consider the presence of underlying depression and autoimmune disease as a potential contraindication to treatment with interferon-α2b and closely monitor such patients if interferon-α2b is used (Box 2). Practical guidelines for clinical management of interferon-α2b-related adverse effects are available.32
Literature review and analysis
The initial ECOG 1684 prospective randomized trial demonstrated a benefit in relapse-free and overall survival for patients with stage III melanoma treated with a 1-year course of interferon-α2b.24 Long-term follow-up studies confirmed a benefit in relapse-free survival, but failed to show an overall survival benefit.26 Subsequent randomized studies confirmed a benefit in relapse-free survival, but results indicating an overall survival benefit were inconsistent.25,33 Several meta-analyses evaluated the clinical benefits of interferon-α2b and indicate a benefit in relapse-free survival and a trend toward improved overall survival.29,30,31 The panel generally considered the data to provide level A evidence for a benefit in relapse-free survival with level B support for an improvement in overall survival from treatment with interferon-α2b. Pegylated-interferon-α2b was approved by the FDA based on improvement in relapse-free survival in patients with microscopic nodal disease.4 A post-hoc analysis also suggested that primary tumours harbouring ulceration were more likely to benefit from pegylated-interferon-α2b.28 The panel considered this to be level B data in support of pegylated-interferon-α2b.
Immunotherapy in stage IV melanoma
Clinical question: What is the appropriate use of immunotherapy in stage IV melanoma?
Initial assessment
In patients with stage lV melanoma, a diagnostic workup that includes a multidisciplinary team review of clinical and tumour data should be conducted. Staging should be confirmed via pathological evaluation, whole-body imaging, and serum LDH analysis. Genetic mutation analysis of the tumour should also be performed. Special emphasis should be placed on central nervous system (CNS) assessment and surgical evaluation by a qualified surgical oncologist for possible metastasectomy. If complete resection of all metastatic disease is possible, patients should consider metastasectomy as first-line treatment; this is supported by level B retrospective outcome studies, especially when a solitary metastasis is present (Figure 3).34,35,36,37 Following immunotherapy, patients who achieve partial or stable disease responses should be re-assessed for resection.38,39 The panel recognizes several systemic treatment options for unresectable stage IV melanoma, including high-dose IL-2 (where available), ipilimumab, vemurafenib, dabrafenib and trametinib for patients with BRAF mutated tumours, clinical trial participation and cytotoxic chemotherapy.
All treatment options shown may be appropriate and final selection of therapy should be individualized based on patient eligibility and treatment availability at the physician's discretion. These algorithms represent consensus sequencing suggestions by the panel. (1) All patients should be evaluated for surgical resection before and after immunotherapy treatment. There was level B data for a clinical benefit with surgical resection of completely resectable lesions and first-line surgical resection was a minority opinion (9%) of the consensus panel. (2) The panel recommended a BRAF inhibitor for patients with BRAF-mutated melanoma with poor PS, who have untreated CNS disease and who are not candidates for clinical trials. (3) The panel recommended that immunotherapy be considered in patients with BRAF-mutated melanoma who have been treated with a BRAF inhibitor if their PS improved with treatment and CNS disease is controlled. IL-2 can be considered in those patients who have a good PS and otherwise qualify for IL-2 administration as per local institutional guidelines. (4) The panel recommended that ipilimumab be considered for patients with BRAF-mutated melanoma with an initial poor PS who respond to a BRAF inhibitor and who are not candidates for IL-2 treatment or clinical trials. (5) The panel recommended that chemotherapy be considered in patients who have disease progression on a BRAF inhibitor and immunotherapy or who are not candidates for immunotherapy or clinical trials. (6) The panel was generally enthusiastic about recommending appropriate clinical trials for patients with melanoma. In most cases individual clinical trials should be considered pending patient eligibility and interest. (7) The panel recommended that IL-2 be considered first, provided that patients have a good PS and otherwise meet local institutional guidelines for IL-2 administration. Patients who are not candidates for IL-2 therapy should consider ipilimumab. (8) The panel recommended that patients with BRAF-mutated melanoma and a good PS with no evidence of CNS disease, or with treated CNS disease, consider immunotherapy first and delay a BRAF inhibitor until there is unequivocal evidence of disease progression. Abbreviations: BRAF+, positive for actionable BRAF mutations; BRAF−, negative for actionable BRAF mutations; CNS, central nervous system; IL, interleukin; KIT+, positive for actionable KIT mutations; LDH, lactate dehydrogenase; PS, performance status.
Consensus management of stage IV melanoma with good clinical performance and BRAF-mutated tumours
The treatment approach for patients with stage IV melanoma who are not surgical candidates should include an assessment of BRAF mutation status (and/or other high priority molecular targets with drugs in development, such as KIT), performance status and complete evaluation for CNS disease before treatment selection. A panel majority recommends patients whose tumours harbour a BRAF mutation with a good performance status and no CNS disease be treated with IL-2 as first-line therapy, provided they meet IL-2 eligibility, and a BRAF inhibitor should be reserved for later treatment stages (Figure 3). Panel members recommend targeted therapy or ipilimumab as second-line or third-line therapy in these patients. There was general consensus that immunotherapy should be used first owing to the durable response rates observed, and a BRAF inhibitor should be considered when the disease is progressing rapidly or when performance status is poor.
Consensus management of stage IV melanoma with poor clinical performance and BRAF-mutated tumours
In patients whose melanoma harbours a BRAF mutation, but who have a poor performance status or uncontrolled CNS disease, vemurafenib, dabrafenib and/or trametinib should be considered to be the first-line therapy. The panel recommends that ipilimumab or chemotherapy be considered as second-line treatment in these patients. The panel recommends several options for third-line therapy in patients with these characteristics, including single-agent chemotherapy, palliative care, combination chemotherapy, clinical trials or IL-2, if performance status improves and/or CNS disease is controlled.
Consensus management of stage IV melanoma with good clinical performance and BRAF wild-type tumours
In patients with wild-type BRAF melanoma who have good performance status and no evidence of CNS disease, the panel recommends IL-2 as first-line therapy with a minority considering ipilimumab, clinical trials, chemotherapy or other regimens. The panel recognized that there is limited to no data on drug sequencing or possible untoward reactions between the available agents. Although the panel accepted that IL-2 and ipilimumab are acceptable agents for these patients, it is often challenging to administer high-dose IL-2 in patients with rapidly progressive disease or a declining performance status and there are no data documenting the safety of IL-2 after treatment with ipilimumab. These reasons led the panel to recommend IL-2 first. The panel generally agrees that patients who did not respond to IL-2 should receive ipilimumab as second-line treatment and then consider clinical trials or chemotherapy as third-line options. The delayed kinetics of antitumour activity with ipilimumab also suggests that patients should have a good performance status and have time to receive and respond to treatment before starting therapy.
Consensus management of stage IV melanoma with poor clinical performance and BRAF wild-type tumours
In patients with a wild-type BRAF melanoma with poor performance status or in the presence of uncontrolled CNS metastasis, the first-line treatment should consist of ipilimumab, clinical trial participation or chemotherapy. These patients often require individualized management with attention given to the control of CNS disease through resection or radiation therapy and careful consideration to the performance status, tempo of disease progression and realistic assessment of life expectancy.
Consensus management of KIT mutated melanoma
In the special situation where a patient has a melanoma with a known KIT mutation, the panel recommends participation in a clinical trial of a KIT inhibitor. Secondary treatment recommendations include IL-2, ipilimumab and chemotherapy.
Consensus management of clinical response
All patients should continue their designated treatment until maximum response is reached or confirmed progression or unacceptable adverse effects occur. The assessment of response might be particularly difficult in patients receiving ipilimumab, because delayed responses have been reported.12,40,41 These patients should be followed after treatment until evidence of clinical deterioration or confirmation of tumour progression by follow-up imaging at least 4 weeks after progression is first noted.
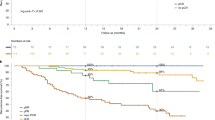
Literature review and analysis
There is data supporting a role for high-dose IL-2, ipilimumab and targeted therapy in the treatment of patients with stage IV melanoma. Early single-institutional and multi-institutional single-arm clinical trials of high-dose IL-2 in patients with metastatic melanoma revealed objective response rates of 16–17%, including a 6–7% complete response rate.42,43 Further follow-up has shown 80–90% of complete responders remain alive 10–15 years later.7 Durability and consistency of responses led to the FDA approval of IL-2 for metastatic melanoma in 1998. Ipilimumab has been evaluated in several phase I and II clinical trials and demonstrated an improvement in overall survival in patients with metastatic melanoma in two large prospective randomized phase III trials.5,9,44,45 In a double-blind, randomized phase III trial, 676 patients with advanced-stage melanoma who expressed the HLA-A2 haplotype were treated with ipilimumab (3 mg/kg), ipilimumab (3 mg/kg) and an HLA-A2-restricted modified gp100 peptide vaccine, or vaccine alone. Patients who received ipilimumab in either treatment arm had improved overall survival compared to patients receiving vaccine alone (10 months versus 6 months; P = 0.0026).5 A second randomized trial assessed 502 patients with previously untreated metastatic melanoma who were randomly assigned to receive ipilimumab (10 mg/kg) and dacarbazine (850 mg/m2 body-surface area) or dacarbazine (850 mg/m2) and placebo.9 In that trial, overall survival was increased in patients who received ipilimumab (11.2 months versus 9.1 months; P <0.001). The 3-year survival was also higher in patients receiving ipilimumab (20.8% versus 12.2%; hazard ratio for death, 0.72; P <0.001). Ipilimumab has also been shown to have activity against CNS metastases in a phase II clinical trial.46
Vemurafenib was evaluated in a prospective, randomized phase III study in 675 previously untreated patients with metastatic melanoma harbouring a BRAFV600E mutation. In that study patients were randomly assigned to vemurafenib (960 mg twice daily) or dacarbazine (1,000 mg/m2 body-surface area every 3 weeks). A significant improvement in overall survival (hazard ratio 0.37, P <0.001) and progression-free survival (5.3 months versus 1.6 months; hazard ratio 0.26, P <0.001) favouring vemurafenib led to FDA approval in late 2011.6 Although combinations of the above agents are planned, there are currently no prospective data on clinical outcomes with concurrent or sequential combinations. The panel concluded there are level A and level B data supporting each drug, but no data are available to promote specific combinations or sequencing of drugs at this time.
Special issues
Clinical question: What are the special issues and clinical management recommendations in the use of immunotherapy for the treatment of melanoma?
There are a number of special issues related to clinical management of patients receiving immunotherapy. Almost all forms of immunotherapy have been associated with the development of autoimmune adverse effects.47,48,49,50,51,52,53,54,55,56,57,58 These effects can range from asymptomatic vitiligo or autoimmune thyroiditis, to symptomatic skin, gastrointestinal, hepatic and endocrine immune-related toxic effects, as seen with ipilimumab.47,48,49,50,51,52,53,54,55,56,57,58 The development of autoimmunity might be associated with clinical response, as a report demonstrated an association between autoimmune thyroid dysfunction and improved relapse-free and overall survival in patients with melanoma who were treated with adjuvant interferon-α2b or IL-2.58,59 Although the panel recognizes published guidelines for the treatment of patients with interferon-α2b,32 IL-260 and ipilimumab,10 four special-issue topics were identified where there are not significant level A or level B data to guide clinical recommendations. These issues include the management of interferon-related depression, frequency of clinical laboratory monitoring and imaging during treatment and how to determine when to stop therapy (Box 2).
Consensus management of interferon-related depression
Depression and related constitutional symptoms, such as fatigue, anorexia and anxiety can be a major treatment management challenge during interferon-α2b therapy. Depression can be profound and has been associated with suicidal ideation and attempts.61 The panel generally recommends a significant history of major depression or related psychiatric conditions be considered to be a relative contraindication to any form of interferon treatment. The majority panel opinion is to selectively use antidepressants in patients who develop depressive symptoms during treatment, which commonly occurs around 5–6 months into treatment.61,62 A panel minority recommends prophylactic use of antidepressants before initiating treatment with interferon-α2b and some panellists suggest early referral to a psychologist or psychiatrist.
Consensus management of autoimmune-related toxic effects
Immunotherapy is associated with a range of cell and metabolic toxic effects that need to be carefully monitored during and after treatment. Special attention to the development of autoimmune-like symptoms is particularly important and these have been reported with interferon-α2b,32,55 IL-257,60 and ipilimumab.10 The panel recommends all patients be routinely assessed with thyroid function studies, complete blood counts, liver function and metabolic panels, and serum LDH tests. The majority opinion is that baseline laboratory data should be obtained on all patients treated with any immunotherapy and then weekly during induction and monthly for patients on standard high-dose interferon-α2b therapy. The panel is divided on recommendations for pegylated-interferon-α2b with two minority opinions: some panellists recommend monthly analysis and others recommend weekly for 1 month and then monthly until stable. Most panellists recommend daily laboratory analysis during IL-2 treatment and some panellists also get tests 1 week after stopping treatment. All panellists agree laboratory reports should be obtained before each ipilimumab infusion, but are divided on long-term follow-up, with some members recommending repeat laboratory analysis every 3 months for 2 years and some recommending the frequency based on individual response and side effects (Box 2).
Consensus management of imaging for patients receiving immunotherapy
The type and frequency of imaging for patients with melanoma is controversial. Since clinical responses can be delayed with some forms of immunotherapy, appropriate imaging becomes increasingly important to assure potential therapeutic benefit is confirmed. All panellists recommend whole-body imaging before all immunotherapy with a majority recommending CT scans of the chest, abdomen and pelvis and MRI of the brain. This brain imaging is particularly important as IL-2 might increase neurological sequelae in patients with CNS lesions and ipilimumab has demonstrated activity in treating CNS disease. A panel minority recommends whole-body PET or PET–CT scans. The false-positive rate for PET and difficulty providing definitive lesion measurements were reasons cited for preferring CT and MRI imaging. The panel recognizes the absence of level A data to support imaging, but the consensus of the panel was to recommend post-treatment imaging in all patients although there was a range of opinion related to frequency. For patients with stage III melanoma, re-imaging is recommended every 3 to 12 months depending on the disease-free period from diagnosis and as clinically indicated (Box 2). For stage IV patients, nearly all panellists recommend re-imaging with the majority recommending every 3 months for a 2-year period and then every 6 months until 5 years post-treatment unless there is evidence of disease progression. A minority opinion suggests imaging should be individualized to each patient.
Consensus management of clinical end points for patients receiving immunotherapy
The kinetics of response with immunotherapy might be such that delayed clinical responses can occur after treatment, and this has been documented for ipilimumab in particular.40,63 Some patients can demonstrate tumour growth or even the appearance of new lesions before the onset of tumour regression; therefore, some immunotherapists have suggested new clinical outcome guidelines.11,12 These guidelines are generally endorsed by the panel; they recommend treatment with immunotherapy be stopped only after significant toxic effects occur or unequivocal evidence of disease progression. The appearance of new lesions or significant increase in tumour burden should be indicators to stop treatment with interferon or IL-2, but more caution is needed when evaluating clinical response to ipilimumab. Most panellists agree re-imaging within 1–2 months is indicated for patients with asymptomatic apparent disease progression 3 months following initiation of therapy with ipilimumab. The panel also suggests patients be considered for resection in situations where responses are mixed or incomplete following immunotherapy with some members further recommending biopsy in ambiguous cases.
Literature review and analysis
Although depression is a recognized side effect of interferon and IL-2 treatment, there are few level A data addressing the role of either pharmacological or psychoanalytical management of this condition.3,61,62 Depressive symptoms can be dose-dependent and various mechanisms have been proposed, including decreased tryptophan levels (a precursor of 5-hydroxytryptamine), alterations in corticotropin-releasing factors, release of soluble ICAM-1, and secondary increase in permeability of the blood–brain barrier.64,65,66 These hypotheses have not been confirmed.67 A small randomized trial evaluated the non-steroidal anti-inflammatory drug indomethacin and reported no difference in depression frequency between patients who received indomethacin and placebo.68 In a double-blind, randomized phase II trial of 40 patients undergoing interferon-α2b treatment for melanoma, the selective 5-hydroxytryptamine reuptake inhibitor paroxetine significantly decreased depression and increased the likelihood that patients completed the course of treatment as compared to patients receiving placebo.69 The panel considers there to be level B data supporting prophylactic anti-depressant use.
There are no prospective randomized trials evaluating the role of routine laboratory monitoring or clinical imaging in patients with melanoma. Thus, only level C data are available and this has been cited as an important area for increased evidence-based research in oncology.70 The delayed kinetics of clinical response has been documented in patients with metastatic melanoma treated with ipilimumab.40,63 New immune-related response criteria have been developed, but require further validation.11,12 Thus, limited level C data were considered to be available for clinical monitoring and end point assessment.
Future perspectives
The success of immunotherapy in the treatment of melanoma is expected to result in the approval and development of additional agents over the next several years. There is considerable excitement in the field for T-cell checkpoint inhibitors for cancer therapy. Programmed death 1 (PD-1) is a T-cell checkpoint molecule that is expressed on activated T cells in a manner similar to CTLA-4, the major target of ipilimumab.71 PD-1 binds to several ligands, including the programmed death ligand 1 (PD-L1) and PD-L2. When PD-1 is engaged by its receptors, T-cell activity is suppressed and blockade of both PD-1 and PD-L1 seems to be promising for cancer immunotherapy. Early phase clinical trials of two distinct monoclonal antibodies targeting PD-1 have shown impressive clinical responses in melanoma and other cancer types, including renal cell, non-small-cell lung and ovarian cancers.71,72 An antibody targeting PD-L1 has also shown therapeutic benefit in early clinical trials.73 These early phase clinical studies also suggested that local PD-L1 expressed on tumour cells and on other cells within the tumour microenvironment might be part of a more-general mechanism through which PD-1-positive T cells are eliminated by established tumours; therefore, PD-L1 expression might be a potential biomarker of immunotherapy response, although this requires further prospective validation.74 Results from a clinical trial also demonstrate that the combination of immunotherapy using an anti-CTLA-4 and anti-PD-1 antibody together resulted in a 53% objective response rate in patients with melanoma, suggesting that combinations of immunotherapy may be an important area for future investigation.75
In addition, there are several reports of a potent abscopal effect when ipilimumab and IL-2 were used after localized radiotherapy, suggesting that combinations of immunotherapy and standard radiation treatment might also be a possible therapeutic strategy.76,77 Another immunotherapeutic strategy demonstrating promise is the use of an oncolytic herpes virus encoding granulocyte-macrophage colony-stimulating factor for the treatment of melanoma, and results of a randomized phase III clinical trial are awaited.78 Another approach is to use T cells expressing modified T-cell receptors capable of recognizing tumour-associated antigens while providing T-cell activation signals upon antigen recognition. Chimeric antigen receptor T cells targeting CD19 have been tested in patients with leukaemia with promising initial results and similar trials are anticipated in melanoma.79,80 There are other agents in clinical development and it is anticipated that more such immunotherapy strategies will be entering clinical trials in the near future.
Conclusions
Immunotherapy is an established modality for treating patients with melanoma with selected patients achieving durable therapeutic responses. These agents have unique mechanisms of action and toxicity profiles that require careful patient selection and clinical management. SITC has provided a consensus statement by a panel of immunotherapy experts and patient advocates for integrating immunotherapy into the clinical management of melanoma. The appropriate use of tumour immunotherapy can provide meaningful benefit to patients with melanoma.
Change history
12 September 2013
In the version of this article initially published online, under the subheading ‘Consensus management of stage IV melanoma with good clinical performance and BRAF wild-type tumours’ the third sentence in the paragraph should have read “Although the panel accepted that IL-2 and ipilimumab are acceptable agents for these patients, it is often challenging…”. On page 3, under the subheading ‘Consensus management of stage II melanoma”, the third sentence in the paragraph should have read ‘A few panelists (5%)...”. Under the subheading, ‘Literature review and analysis’ the fourth sentence should have read “but no benefit in overall survival (HR = 0.91, 95% CI 0.74–1.10; P = 0.642).” In Figure 3 and the text under the ‘Consensus management of stage IV melanoma with good clinical performance and BRAF-mutated tumours’ the term vermurafenib in several places should have read ‘a BRAF inhibitor’. The order of references 74 and 75 should have been reverted. These errors have been corrected for the HTML and PDF versions of the article.
References
National Cancer Institute. Cancer Trends Progress Report--2011/2012 Update [online], (2012).
Garbe, C., Eigentler, T. K., Keilholz, U., Hauschild, A. & Kirkwood, J. M. Systematic review of medical treatment in melanoma: current status and future prospects. Oncologist 16, 5–24 (2011).
Balch, C. M. et al. Final version of 2009 AJCC melanoma staging and classification. J. Clin. Oncol. 27, 6199–6206 (2009).
Eggermont, A. M. et al. Adjuvant therapy with pegylated interferon alfa-2b versus observation alone in resected stage III melanoma: final results of EORTC 18991, a randomised phase III trial. Lancet 372, 117–126 (2008).
Hodi, F. S. et al. Improved survival with ipilimumab in patients with metastatic melanoma. N. Engl. J. Med. 363, 711–723 (2010).
Chapman, P. B. et al. Improved survival with vemurafenib in melanoma with BRAF V600E mutation. N. Engl. J. Med. 364, 2507–2516 (2011).
Atkins, M. B., Kunkel, L., Sznol, M. & Rosenberg, S. A. High-dose recombinant interleukin-2 therapy in patients with metastatic melanoma: long-term survival update. Cancer J. Sci. Am. 6 (Suppl. 1), S11–S14 (2000).
Prieto, P. A. et al. CTLA-4 blockade with ipilimumab: long-term follow-up of 177 patients with metastatic melanoma. Clin. Cancer Res. 18, 2039–2047 (2012).
Robert, C. et al. Ipilimumab plus dacarbazine for previously untreated metastatic melanoma. N. Engl. J. Med. 364, 2517–2526 (2011).
Weber, J. S., Kahler, K. C. & Hauschild, A. Management of immune-related adverse events and kinetics of response with ipilimumab. J. Clin. Oncol. 30, 2691–2697 (2012).
Hoos, A. et al. Improved endpoints for cancer immunotherapy trials. J. Natl Cancer Inst. 102, 1388–1397 (2010).
Wolchok, J. D. et al. Guidelines for the evaluation of immune therapy activity in solid tumors: immune-related response criteria. Clin. Cancer Res. 15, 7412–7420 (2009).
Graham, R., Mancher, M., Miller Wolman, D., Greenfield, S. & Steinberg, E. (Eds) Clinical practice guidelines we can trust (Institute of Medicine of the National Academies, Washington D. C., 2011).
SITC. Cancer Immunotherapy Guidelines [online], (2013).
Soong, S. J. et al. Predicting survival outcome of localized melanoma: an electronic prediction tool based on the AJCC melanoma database. Ann. Surg. Oncol. 17, 2006–2014 (2010).
Wong, S. L. et al. Sentinel lymph node biopsy for melanoma: American Society of Clinical Oncology and Society of Surgical Oncology joint clinical practice guideline. J. Clin. Oncol. 30, 2912–2918 (2012).
Grob, J. J. et al. Randomised trial of interferon alpha-2a as adjuvant therapy in resected primary melanoma thicker than 1.5 mm without clinically detectable node metastases. French Cooperative Group on Melanoma. Lancet 351, 1905–1910 (1998).
Hansson, J. et al. Two different durations of adjuvant therapy with intermediate-dose interferon alfa-2b in patients with high-risk melanoma (Nordic IFN trial): a randomised phase 3 trial. Lancet Oncol. 12, 144–152 (2011).
Hauschild, A. et al. Prospective randomized trial of interferon alfa-2b and interleukin-2 as adjuvant treatment for resected intermediate- and high-risk primary melanoma without clinically detectable node metastasis. J. Clin. Oncol. 21, 2883–2888 (2003).
Hancock, B. W. et al. Adjuvant interferon in high-risk melanoma: the AIM HIGH Study--United Kingdom Coordinating Committee on Cancer Research randomized study of adjuvant low-dose extended-duration interferon Alfa-2a in high-risk resected malignant melanoma. J. Clin. Oncol. 22, 53–61 (2004).
Hauschild, A. et al. Prospective randomized multicenter adjuvant dermatologic cooperative oncology group trial of low-dose interferon alfa-2b with or without a modified high-dose interferon alfa-2b induction phase in patients with lymph node-negative melanoma. J. Clin. Oncol. 27, 3496–3502 (2009).
Hauschild, A. et al. Efficacy of low-dose interferon {alpha}2a 18 versus 60 months of treatment in patients with primary melanoma of >= 1.5 mm tumor thickness: results of a randomized phase III DeCOG trial. J. Clin. Oncol. 28, 841–846 (2010).
Tarhini, A. A., Gogas, H. & Kirkwood, J. M. INF-α in the treatment of melanoma. J. Immunol. 89, 3789–3793 (2012).
Kirkwood, J. M. et al. Interferon alfa-2b adjuvant therapy of high-risk resected cutaneous melanoma: the Eastern Cooperative Oncology Group Trial EST 1684. J. Clin. Oncol. 14, 7–17 (1996).
Kirkwood, J. M. et al. High- and low-dose interferon alfa-2b in high-risk melanoma: first analysis of intergroup trial E1690/S9111/C9190. J. Clin. Oncol. 18, 2444–2458 (2000).
Kirkwood, J. M. et al. A pooled analysis of eastern cooperative oncology group and intergroup trials of adjuvant high-dose interferon for melanoma. Clin. Cancer Res. 10, 1670–1677 (2004).
Bottomley, A. et al. Adjuvant therapy with pegylated interferon alfa-2b versus observation in resected stage III melanoma: a phase III randomized controlled trial of health-related quality of life and symptoms by the European Organisation for Research and Treatment of Cancer Melanoma Group. J. Clin. Oncol. 27, 2916–2923 (2009).
Eggermont, A. M. et al. Ulceration and stage are predictive of interferon efficacy in melanoma: results of the phase III adjuvant trials EORTC 18952 and EORTC 18991. Eur. J. Cancer 48, 218–225 (2012).
Hernberg, M., Pyrhonen, S. & Muhonen, T. Regimens with or without interferon-alpha as treatment for metastatic melanoma and renal cell carcinoma: an overview of randomized trials. J. Immunother. 22, 145–154 (1999).
Pirard, D., Heenen, M., Melot, C. & Vereecken, P. Interferon alpha as adjuvant postsurgical treatment of melanoma: a meta-analysis. Dermatology 208, 43–48 (2004).
Mocellin, S., Pasquali, S., Rossi, C. R. & Nitti, D. Interferon alpha adjuvant therapy in patients with high-risk melanoma: a systematic review and meta-analysis. J. Natl Cancer Inst. 102, 493–501 (2010).
Hauschild, A. et al. Practical guidelines for the management of interferon-alpha-2b side effects in patients receiving adjuvant treatment for melanoma: expert opinion. Cancer 112, 982–994 (2008).
Kirkwood, J. M. et al. High-dose interferon alfa-2b significantly prolongs relapse-free and overall survival compared with the GM2-KLH/QS-21 vaccine in patients with resected stage IIB-III melanoma: results of intergroup trial E1694/S9512/C509801. J. Clin. Oncol. 19, 2370–2380 (2001).
Schuhan, C., Muley, T., Dienemann, H. & Pfannschmidt, J. Survival after pulmonary metastasectomy in patients with malignant melanoma. Thorac. Cardiovasc. Surg. 59, 158–162 (2011).
Wasif, N., Bagaria, S. P., Ray, P. & Morton, D. L. Does metastasectomy improve survival in patients with Stage IV melanoma? A cancer registry analysis of outcomes. J. Surg. Oncol. 104, 111–115 (2011).
Chua, T. C. et al. Surgical management of melanoma lung metastasis: an analysis of survival outcomes in 292 consecutive patients. Ann. Surg. Oncol. 19, 1774–1781 (2012).
Howard, J. H. et al. Metastasectomy for distant metastatic melanoma: analysis of data from the first multicenter selective lymphadenectomy trial (MSLT-I). Ann. Surg. Oncol. 19, 2547–2555 (2012).
Lee, D. S., White, D. E., Hurst, R., Rosenberg, S. A. & Yang, J. C. Patterns of relapse and response to retreatment in patients with metastatic melanoma or renal cell carcinoma who responded to interleukin-2-based immunotherapy. Cancer J. Sci. Am. 4, 86–93 (1998).
Verdecchia, G. M. et al. Adjuvant adoptive immunotherapy in patients with stage III and resected stage IV melanoma: a pilot study [Italian]. Tumori 89, 298–300 (2003).
Saenger, Y. M. & Wolchok, J. D. The heterogeneity of the kinetics of response to ipilimumab in metastatic melanoma: patient cases. Cancer Immun. 8, 1 (2008).
Pennock, G. K., Waterfield, W. & Wolchok, J. D. Patient responses to ipilimumab, a novel immunopotentiator for metastatic melanoma: How different are these from conventional treatment responses? Am. J. Clin. Oncol. 35, 606–611 (2012).
Rosenberg, S. A. et al. Treatment of 283 consecutive patients with metastatic melanoma or renal cell cancer using high-dose bolus interleukin 2. JAMA 271, 907–913 (1994).
Atkins, M. B. et al. High-dose recombinant interleukin 2 therapy for patients with metastatic melanoma: analysis of 270 patients treated between 1985 and 1993. J. Clin. Oncol. 17, 2105–2116 (1999).
Wolchok, J. D. et al. Ipilimumab monotherapy in patients with pretreated advanced melanoma: a randomised, double-blind, multicentre, phase 2, dose-ranging study. Lancet Oncol. 11, 155–164 (2010).
Trinh, V. A. & Hwu, W. J. Ipilimumab in the treatment of melanoma. Expert Opin. Biol. Ther. 12, 773–782 (2012).
Margolin, K. et al. Ipilimumab in patients with melanoma and brain metastases: an open-label, phase 2 trial. Lancet Oncol. 13, 459–465 (2012).
Pichert, G., Jost, L. M., Fierz, W. & Stahel, R. A. Clinical and immune modulatory effects of alternative weekly interleukin-2 and interferon alfa-2a in patients with advanced renal cell carcinoma and melanoma. Br. J. Cancer 63, 287–292 (1991).
Dorval, T., Fridman, W. H., Mathiot, C., Sastre, X. & Pouillart, P. Treatment of metastatic malignant melanoma with interleukin-2 [French]. Bull. Cancer 79, 781–787 (1992).
Monig, H., Hauschild, A., Lange, S. & Folsch, U. R. Suppressed thyroid-stimulating hormone secretion in patients treated with interleukin-2 and interferon-alpha 2b for metastatic melanoma. Clin. Investig. 72, 975–978 (1994).
Vlasveld, L. T. et al. Phase II study of intermittent continuous infusion of low-dose recombinant interleukin-2 in advanced melanoma and renal cell cancer. Ann. Oncol. 5, 179–181 (1994).
Farace, F. et al. Low-dose IL-2 treatment: activation of discrete T- and NK-cell sub-populations in vivo. Int. J. Cancer 62, 523–528 (1995).
Fleischmann, M., Celerier, P., Bernard, P., Litoux, P. & Dreno, B. Long-term interferon-alpha therapy induces autoantibodies against epidermis. Dermatology 192, 50–55 (1996).
Trehu, E. G. et al. Phase I trial of interleukin 2 in combination with the soluble tumor necrosis factor receptor p75 IgG chimera. Clin. Cancer Res. 2, 1341–1351 (1996).
McDermott, D. F. et al. A two-part phase I trial of high-dose interleukin 2 in combination with soluble (Chinese hamster ovary) interleukin 1 receptor. Clin. Cancer Res. 4, 1203–1213 (1998).
Schachter, J. et al. Toxicity of adjuvant high-dose interferon-alpha-2b in patients with cutaneous melanoma at high risk of recurrence. Oncol. Rep. 6, 1389–1393 (1999).
Fraenkel, P. G. et al. Induction of myasthenia gravis, myositis, and insulin-dependent diabetes mellitus by high-dose interleukin-2 in a patient with renal cell cancer. J. Immunother. 25, 373–378 (2002).
Chianese-Bullock, K. A. et al. Autoimmune toxicities associated with the administration of antitumor vaccines and low-dose interleukin-2. J. Immunother. 28, 412–419 (2005).
Gogas, H. et al. Prognostic significance of autoimmunity during treatment of melanoma with interferon. N. Engl. J. Med. 354, 709–718 (2006).
Koon, H. & Atkins, M. Autoimmunity and immunotherapy for cancer. N. Engl. J. Med. 354, 758–760 (2006).
Schwartzentruber, D. J. Guidelines for the safe administration of high-dose interleukin-2. J. Immunother. 24, 287–293 (2001).
Friebe, A. et al. Dose-dependent development of depressive symptoms during adjuvant interferon-{alpha} treatment of patients with malignant melanoma. Psychosomatics 51, 466–473 (2010).
Pizzi, C. et al. Low-dose recombinant IL-2 induces psychological changes: monitoring by Minnesota Multiphasic Personality Inventory (MMPI). Anticancer Res. 22, 727–732 (2002).
Weber, J. Review: anti-CTLA-4 antibody ipilimumab: case studies of clinical response and immune-related adverse events. Oncologist 12, 864–872 (2007).
Capuron, L. et al. Association of exaggerated HPA axis response to the initial injection of interferon-alpha with development of depression during interferon-alpha therapy. Am. J. Psychiatry 160, 1342–1345 (2003).
Van Gool, A. R. et al. Serum amino acids, biopterin and neopterin during long-term immunotherapy with interferon-alpha in high-risk melanoma patients. Psychiatry Res. 119, 125–132 (2003).
Schaefer, M. et al. Correlation between sICAM-1 and depressive symptoms during adjuvant treatment of melanoma with interferon-alpha. Brain Behav. Immun. 18, 555–562 (2004).
Bannink, M. et al. Interferon-alpha influences tryptophan metabolism without inducing psychiatric side effects. Neuropsychobiology 55, 225–231 (2007).
Miller, R. L. et al. Randomized trial of recombinant alpha 2b-interferon with or without indomethacin in patients with metastatic malignant melanoma. Cancer Res. 49, 1871–1876 (1989).
Musselman, D. L. et al. Paroxetine for the prevention of depression induced by high-dose interferon alfa. N. Engl. J. Med. 344, 961–966 (2001).
Poonacha, T. K. & Go, R. S. Level of scientific evidence underlying recommendations arising from the National Comprehensive Cancer Network clinical practice guidelines. J. Clin. Oncol. 29, 186–191 (2011).
Topalian, S. L. et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N. Engl. J. Med. 366, 2443–2454 (2012).
Hamid, O. et al. Safety and tumor responses with lambrolizumab (anti-PD-1) in melanoma. N. Engl. J. Med. 369, 134–144 (2013).
Brahmer, J. R. et al. Safety and activity of anti-PD-L1 antibody in patients with advanced cancer. N. Engl. J. Med. 366, 2455–2465 (2012).
Topalian, S. L., Drake, C. G. & Pardoll, D. M. Targeting the PD-1/b7-H1 (PD-L1) pathway to activate anti-tumor immunity. Curr. Opin. Immunol. 24, 207–212 (2012).
Wolchok, J. D. et al. Nivolumab plus ipilimumab in advanced melanoma. N. Engl. J. Med. 369, 122–133 (2013).
Postow, M. A. et al. Immunologic correlates of the abscopal effect in a patient with melanoma. N. Engl. J. Med. 366, 925–931 (2012).
Seung, S. K. et al. Phase 1 study of stereotactic body radiotherapy and interleukin-2-tumor and immunologic responses. Sci. Transl. Med. 4, 137–174 (2012).
Kaufman, H. L. & Bines, S. D. OPTIM trial: a phase III trial of an oncolytic herpes virus encoding GM-CSF for unresectable stage III or IV melanoma. Future Oncol. 6, 941–949 (2010).
Grupp, S. A. et al. Chimeric antigen receptor-modified T cells for acute lymphosis leukemia. N. Engl. J. Med. 368, 1509–1518 (2013).
Burns, W. R. et al. A high molecular-weight melanoma-associated antigen-specific chimeric antigen receptor redirects lymphocytes to target human melanomas. Cancer Res. 70, 3027–3033 (2010).
Author information
Authors and Affiliations
Contributions
H. L. Kaufman, J. M. Kirkwood, F. S. Hodi and M. B. Atkins researched the data for the article and wrote the manuscript. All authors made a substantial contribution to the discussion of the content and reviewed the article prior to submission.
Corresponding author
Ethics declarations
Competing interests
H. L. Kaufman acts in a compensated consultant or advisory role at Amgen, EMD Serono and Prometheus. J. M. Kirkwood acts in a compensated consultant or advisory role for, and receives honouraria from Bristol-Myers Squibb, GlaxoSmithKline, Merck and Novartis, and receives research funding from Prometheus. F. S. Hodi is an uncompensated consultant or has an advisory role and receives research funding from Bristol-Myers Squibb and Genentech. S. Agarwala acts in an compensated consultant or advisory role for, and receives honouraria from Bristol-Myers Squibb and Genentech. J. I. Clark receives research funding from Bristol-Myers Squibb and honouraria and research funding from Prometheus. B. Curti acts in a compensated consultant or advisory role for, and receives honouraria and research funding from Bristol-Myers Squibb and Prometheus. M. S. Ernstoff has stock or other ownership interests in, and receives research funding from Bristol-Myers Squibb, and receives research funding from CureTech and Merck. T. Gajewski acts in a compensated consultant or advisory role for, and receives research funding from Bristol-Myers Squibb and GlaxoSmithKline, and receives honouraria from Genentech. R. Gonzalez receives research funding from Incyte and Merck, acts in a compensated consultant or advisory role for, and receives honouraria and research funding from Roche/Genentech, acts in a compensated consultant or advisory role for, and receives research funding from Bristol-Myers Squibb, acts in a compensated consultant or advisory role for, and receives honouraria from GlaxoSmithKline, and receives honouraria and research funding from Prometheus. D. Lawson acts in a compensated consultant or advisory role for Bristol-Myers Squibb, GlaxoSmithKline, Merck and Prometheus. M. Lotze acts in a compensated consultant or advisory role for, and receives honouraria from Celgene. J. Lutzky acts in a compensated consultant or advisory role for, and receives honouraria from Bristol-Myers Squibb and Prometheus, and receives honouraria from Genentech/Roche. K. Margolin acts in a compensated consultant or advisory role for, and receives research funding from Bristol-Myers Squibb and Genentech, and receives research funding from Merck. D. McDermott acts in a compensated consultant or advisory role for Bristol-Myers Squibb, Genentech and Prometheus. J. M. Richards has stock or other ownership interests in, and receives honouraria from Bristol-Myers Squibb. W. Sharfman acts in a compensated consultant or advisory role for, and receives honouraria from Merck and acts in a compensated consultant or advisory role for Genentech. V. K. Sondak acts in a compensated consultant or advisory role for, and receives honouraria from Merck. J. Sosman acts in a compensated consultant or advisory role for Roche, acts in a compensated consultant or advisory role for, and receives research funding from Millennium, and receives research funding from Bristol-Myers Squibb and GlaxoSmithKline. A. Tarhini acts in a compensated consultant or advisory role for Genentech, acts in a compensated consultant or advisory role for, and receives research funding from Merck and Prometheus, and receives research funding from Bristol-Myers Squibb. J. A. Thompson receives research funding from Bristol-Myers Squibb and Genentech. J. Titze acts in a compensated consultant or advisory role for, and receives honouraria from Bristol-Myers Squibb, and receives honouraria from Prometheus. W. Urba acts in a compensated consultant or advisory role for, and receives honouraria and research funding from Bristol-Myers Squibb, acts in an uncompensated consultant or advisory role for Genentech/Roche, and receives research funding from Prometheus. R. White receives honouraria from Merck. M. B. Atkins acts in a compensated consultant or advisory role for Bristol-Myers Squibb, Genentech and Prometheus. T. Amatruda, S. D. Bines, L. Jane Hyde, D. Morton, A. Pavlick and S. Steel declare no competing interests.
Supplementary information
Supplementary Bibliography
Cancer Immunotherapy Guidelines (Melanoma) (PDF 9919 kb)
Supplementary Box 1
Participant List (PDF 54 kb)
Supplementary Box 2
Comments from public review of this consensus statement (PDF 115 kb)
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/.
About this article
Cite this article
Kaufman, H., Kirkwood, J., Hodi, F. et al. The Society for Immunotherapy of Cancer consensus statement on tumour immunotherapy for the treatment of cutaneous melanoma. Nat Rev Clin Oncol 10, 588–598 (2013). https://doi.org/10.1038/nrclinonc.2013.153
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrclinonc.2013.153
This article is cited by
-
Sequencing Targeted and Immune Therapy in BRAF-Mutant Melanoma: Lessons Learned
Current Oncology Reports (2023)
-
Clinical characteristics and treatment outcomes of primary malignant melanoma of esophagus: a single center experience
BMC Gastroenterology (2022)
-
Associating sleep problems with advanced cancer diagnosis, and immune checkpoint treatment outcomes: a pilot study
Supportive Care in Cancer (2022)
-
Current Trends of Immunotherapy in the Treatment of Cutaneous Melanoma: A Review
Dermatology and Therapy (2021)
-
Abdominal CT manifestations of adverse events to immunotherapy: a primer for radiologists
Abdominal Radiology (2020)