Summary:
The purpose of this study was to evaluate the estimated incidence of secondary malignancies post-allogeneic bone marrow transplantation (BMT) in a cohort of adult patients previously reported now with an additional 8.5 years of follow-up. A cohort of 557 patients older than age 16 years underwent allogeneic BMT between June 1970 and November 1993. Histologic reports confirmed the diagnosis of a secondary malignancy. Multivariate Cox proportional hazards method was utilized to investigate predictors for the development of secondary malignancies. In all, 31 patients in this cohort developed a secondary malignancy a median of 6.79 years after their transplant. The estimated cumulative incidence rate of secondary malignancy was 4.2% at 10 years post transplant. When compared to the general population, the estimated observed/expected ratio of new cancer diagnoses was 5.13. On multivariate analysis, older age at the time of transplant was the only significant predictor for development of secondary cancer (P=0.01). The most common malignancies observed were nonmelanomatous skin cancers and squamous cell cancers of the buccal cavity. The risk of developing a secondary malignancy after allogeneic BMT is significant, particularly in older patients. Long-term survivors of transplant require regular monitoring for early signs of cancer, particularly of the skin and oral cavity.
Similar content being viewed by others
Main
One of the long-term complications associated with allogeneic hematopoietic stem cell transplantation is the development of secondary malignancies.1,2,3,4,5,6,7,8 Several factors contribute to the development of secondary neoplasm: the radiation and chemotherapy used for conditioning and for treatment of the primary malignancy, and the profound immunosuppression that occurs post transplant.1,5,6,9,10 Two large cohort studies published by the IBMTR and EBMT have confirmed the increased risk of secondary malignancy post transplant.1,2 When transplant patients are compared to an age-matched, sex-matched normal population, as in the SEER database and the Danish Cancer Registry/Cancer Registry of the Saarland/Germany, respectively, the observed to expected incidence ratios of new cancer diagnosis range from 2.7 to 3.5. These studies found that older age of female recipients or female donors, the number of immunosuppressive agents used for treatment of chronic graft-versus-host disease (GVHD), total-body irradiation (TBI) with overall doses of 1000 cGy or higher, and the presence of chronic GVHD were significant risk factors for the development of secondary malignancy.
Although older age is associated with development of secondary malignancies, most cohort studies have not looked specifically at adult transplant patients. In a previous study, we reported on 10 new malignancies which had developed in nine patients in a cohort of 557 adult transplant patients from a single institution.3 The primary aim of this study was to report on our updated experience of secondary malignancies post transplant and to evaluate the estimated incidence of secondary malignancies in this same cohort of adult patients. Their follow-up has been extended to another 8.5 years, during which an additional 31 new malignancies have developed in 22 patients.
Patients and methods
Patients
A total of 557 consecutive patients underwent allogeneic bone marrow transplantation (BMT) at Princess Margaret Hospital between June 27, 1970 and November 1, 1993 and were originally reported by Lowsky et al.3 They were also reported as part of an IBMTR study by Curtis et al.2 Data on the cohort were collected from a BMT computer database. The length of follow-up of this cohort varied between 8 and 32 years. Over 75% of patients alive at the last known follow-up were seen within 2 years of the last data update and these patients were in active follow-up. A chart review was performed on patients who developed a secondary malignancy. All histological reports were reviewed to confirm the diagnosis of secondary malignancy. Data were last updated on May 3, 2002. Follow-up for patients continued until death or last known follow-up.
Conditioning regimens
Details of the preparative regimens and GVHD prophylaxis used in these patients were previously reported in Lowsky et al.3 In all, 77% of patients received a TBI-containing regimen. The TBI-containing protocols included either a single dose of radiation (300 or 500 cGy) or 1200 cGy of radiation given in 6 fractions over 3 days. A single cobalt-60 radiation source, which was delivered at a median dose rate of 58 cGy/min, was used for all TBI-containing regimens. Cyclosporine was used for GVHD prophylaxis in 65% of patients. Patients in this cohort did not receive manipulated (T-cell-depleted) stem cell products. There was also very little use of antithymocyte globulin or OKT3 either during or following transplantation.
Statistical analysis
Descriptive statistics such as the mean, median, standard deviation and frequency were used to describe the cohort. Univariate Cox proportional hazards regression analysis was used to determine statistically significant predictor variables for the development of a secondary malignancy. A multivariate analysis was performed using univariately significant variables, which were potentially associated with the development of a secondary malignancy. The Kaplan–Meier method was used to estimate the survival post BMT. Cumulative incidence rates of developing a secondary malignancy were estimated after adjusting for the competing risk of patient death. While post-BMT survival was described by grouping patients on whether they developed a secondary malignancy, no statistical comparison was made between groups due to bias in group selection. All tests were two-sided and a P-value of 0.05 or less was considered statistically significant.
Results
Patient characteristics
Characteristics of patients are shown in Table 1. There were 31 patients (5.6%) who later developed a secondary malignancy. Only 10 of these patients have since died; eight died of their secondary malignancy and two died after relapse of their original malignancy. Patients who developed a secondary malignancy were older (age 36 vs 33 years at BMT, P=0.004). They were also more often male (68 vs 55%, P=0.18) and more likely to have chronic myeloid leukemia as their primary diagnosis (52 vs 34%, P=0.18) than patients who did not develop such malignancies, although this did not reach statistical significance. The median follow-up was greater for patients who developed a secondary malignancy (11.2 vs 2.5 years). This reflects the fact that secondary malignancies develop mainly in long-term BMT survivors.11
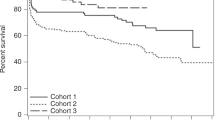
Survival
A plot of the overall survival of this cohort is depicted in Figure 1. The median survival was estimated to be 3.70 years (95% CI 2.20–6.78) following BMT. In all, 47% (95% CI 43.0–51.3%) of patients were estimated to be alive at 5 years post BMT. The number at risk at 3, 5, and 10 years was 288, 259, and 163, respectively.
Incidence of secondary malignancies after BMT
In total, 31 patients developed a secondary malignancy in this cohort of 557 BMT patients. Clinical characteristics of these 31 patients are listed in Table 2. The cumulative incidence rates of a secondary malignancy in this cohort at 10 years is 4.2% (95% CI 2.66–6.26%) and at 15 years is 6.17% (95% CI 3.56–8.76%) (Figure 2). The median time to diagnosis of second malignancy following BMT for the 31 patients was 6.79 years (range 0.5–21.9) and the patients were a median age of 42.4 years at the time of diagnosis of the secondary malignancy. Median survival following diagnosis of a second malignancy has not been reached. Out of these 31 patients, 10 have died and the median follow-up after diagnosis of secondary malignancy is 2.39 years.
There were 3200.01 patient-years of follow-up in this cohort at the time of analysis. The expected number of malignancies calculated using the Ontario Cancer Registry Incidence file of the SEER*Stat software database12 in the same period in the general population is 6.04, giving an estimated observed/expected ratio of 5.13 (95% CI 3.49–7.29).
Univariate and multivariate analyses
Univariate Cox proportional hazards regression was used to investigate potential predictors of the development of a secondary malignancy. Results from the univariate analyses are presented in Table 3. Older age at BMT was the only statistically significant predictor of later development of a secondary malignancy (P=0.004). The use of TBI as part of the preparative regimen and the development of acute or chronic GVHD were not significant predictors for secondary malignancy, unlike the previous study which showed that acute GVHD and the use of TBI were factors significantly associated with the development of secondary neoplasms.3 No variable, including TBI (P=0.26) or acute GVHD (P=0.96), was significantly associated with development of a secondary malignancy after adjusting for age. With only 31 events of interest, there is limited statistical power available to perform a thorough multivariate analysis. However, a multivariate model was constructed using all variables with univariate P-values that were of borderline significance, and the results from this analysis are shown at the bottom of Table 3. Age was the only significant predictor for development of a secondary malignancy. Patients were divided into four groups of roughly equal numbers based on age at the time of transplant in order to assess the association between age and the risk of developing a secondary malignancy (see Table 4). There was a trend towards an increased number of secondary malignancies in older patients and accounted for age being a significant predictor in the multivariate analysis. The standardized incidence ratios, however, were highest in the younger patients, indicating that age is inversely associated with excess risk of developing another malignancy compared to a normal population.
Discussion
This study demonstrates that adult recipients of allogeneic hematopoietic stem cell transplant are at increased risk of developing a secondary malignancy compared with the general population. This cohort developed 5.13 times more malignancies than would be expected in a comparable group from the general population. The actuarial risk of developing a secondary malignancy at 10 years after transplantation is 4.2%. The actuarial risks found in the EBMT and IBMTR studies at 10 years are lower (3.5 and 2.2%, respectively).1,2 The IBMTR study excluded skin cancers and hematologic malignancies. The high incidence of secondary malignancies in our adult cohort may reflect the increased prevalence of malignancies generally seen in an older population (both the EBMT and IBMTR studies contained a significant pediatric population). An association between older age at BMT and secondary malignancy was found on multivariate analysis, in contrast to the previous report.3 Kolb et al1 found a similar association between age and secondary malignancy in female patients surviving more than 5 years following BMT. In the IBMTR study, the risk of cancer was highest in children under age 10, with an observed/expected case ratio of 36.6. The ratios for patients 10–29 and 30 years or older were 4.6 and 1.2–1.4, respectively.2 The present study showed a similar inverse association between the risk of secondary malignancy and age. Unlike the IBMTR study, there was an increased risk of developing a second malignancy of four times the normal in patients older than 30 years. Overall, the absolute number of secondary malignancies was still highest in the older patient groups and accounted for older age being a significant predictor for secondary malignancy in the multivariate analysis (cancer is still a rare event in young people).
It is interesting to note that, although the peak annual occurrence of new malignancies occurred at 7 years post BMT, they continue to be identified many years after transplantation. Also of note is that more than half of the patients developing secondary malignancies are alive and well at the last follow-up. Despite their previous exposure to transplant and chemotherapy, many are able to tolerate further therapy with good response to treatment of their new malignancy. Favre-Schmuziger et al13 reported similar findings.
The original analysis of our cohort of adult patients found that the presence of acute GVHD greater than grade II and TBI-containing conditioning regimens were significant risk factors for developing any type of secondary malignancy.3 The possible associations of acute GVHD with the development of secondary malignancy have not been confirmed with additional follow-up. The use of TBI-containing conditioning regimens was also not associated with later development of a secondary malignancy. This is in contrast with the previous findings of Curtis et al and others.2,3,14 The higher doses of radiation associated with increased risk of developing a new cancer in the above-mentioned studies (single dose of at least 1000 cGy or fractionated disease totaling 1300 cGy or more) were not seen by our study patients and may explain this discrepancy.
Basal cell skin cancer and squamous cell cancer (SCC) of the skin and oral cavity were common, comprising 45.7% (16/31) of the malignancies seen. In all, 14 of these 16 patients had prior chronic GVHD, compared to 9/15 who had chronic GVHD and developed another type of malignancy. While this difference is not statistically significant, the trend is in agreement with other studies indicating that chronic GVHD may be a factor in SCC and other skin cancers.2 The use of immunosuppressive agents for chronic GVHD has been associated with an increased risk of cutaneous and mucosal neoplasms in other studies.1,2,5,15 The prevalence of skin cancer has also been noted in other studies.1,2,15
The present study demonstrated fewer thyroid and brain malignancies than other cohort studies. Studies looking specifically at children have noted increased risk of brain, thyroid, and midline cancers, possibly reflecting greater use of cranial or craniospinal radiotherapy in pediatric patients prior to transplantation.5 The small numbers of brain tumors and thyroid cancers is consistent with the exclusion of children from this study. There was also very little polymorphic post-transplantation lymphoproliferative disorder (PTLD) seen in this cohort. These patients did not receive manipulated stem cell product, and few had alternative donors, both known risk factors for PTLD.
This report confirms the increased risk of secondary malignancies in adult bone marrow transplant recipients. Skin cancers and SCC of the buccal cavity are most commonly seen. This risk does not seem to diminish with time, remaining significant even after a median follow-up of 11 years. Long-term survivors of allogeneic BMT thus require close observation and regular screening exams, since they can potentially do well with early diagnosis and treatment of their secondary malignancy.
References
Kolb HJ, Socie G, Duell T et al. Malignant neoplasms in long-term survivors of bone marrow transplantation. Ann Intern Med 1999; 131: 738–744.
Curtis RE, Rowlings PA, Deeg HJ et al. Solid cancers after bone marrow transplantation. N Engl J Med 1997; 336: 897–904.
Lowsky R, Lipton J, Fyles G et al. Secondary malignancies after bone marrow transplantation in adults. J Clin Oncol 1994; 12: 2187–2192.
Socie G, Curtis RE, Deeg HJ et al. New malignant disease after allogeneic marrow transplantation for childhood acute leukemia. J Clin Oncol 2000; 18: 348–357.
Deeg HJ, Socie G, Schoch G et al. Malignancies after marrow transplantation for aplastic anemia and fanconi anemia: a joint Seattle and Paris analysis of results in 700 patients. Blood 1996; 87: 386–392.
Deeg HJ, Socie G . Malignancies after hematopoietic stem cell transplantation: many questions, some answers. Blood 1998; 91: 1833–1844.
Witherspoon RP, Fisher LD, Schoch G et al. Secondary cancers after bone marrow transplantation for leukemia or aplastic anemia. N Engl J Med 1989; 321: 784–789.
Bhatia S, Ramsay NKC, Steinbuch M et al. Malignant neoplasms following bone marrow transplantation. Blood 1996; 87: 3633–3639.
Kolb HJ, Bender-Gotze C . Late complications after allogeneic bone marrow transplantation for leukaemia. Bone Marrow Transplant 1990; 6: 61–72.
Deeg HJ, Witherspoon RP . Risk factors for the development of secondary malignancies after marrow transplantation. Hematol Oncol Clin North Am 1993; 7: 417–429.
Kolb HJ, Poetscher C . Late effects after allogeneic bone marrow transplantation. Curr Opin Hematol 1997; 4: 401–407.
Ontario Cancer Registry. Cancer Care Ontario. 2002.
Favre-Schmuziger G, Hofer S, Passweg J et al. Treatment of solid tumors following allogeneic bone marrow transplantation. Bone Marrow Transplant 2000; 25: 895–898.
Kulkarni S, Powles R, Treleaven J et al. Melphalan/TBI is not more carcinogeneic than cyclophosphamide/TBI for transplant conditioning: follow-up of 725 patients from a single centre over a period of 26 years. Bone Marrow Transplant 2000; 25: 365–370.
Lishner M, Patterson B, Kandel R et al. Cutaneous and mucosal neoplasms in bone marrow transplant recipients. Cancer 1990; 65: 473–476.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hasegawa, W., Pond, G., Rifkind, J. et al. Long-term follow-up of secondary malignancies in adults after allogeneic bone marrow transplantation. Bone Marrow Transplant 35, 51–55 (2005). https://doi.org/10.1038/sj.bmt.1704706
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bmt.1704706
Keywords
This article is cited by
-
Twenty years of experience of a tertiary cancer center in total body irradiation with focus on oncological outcome and secondary malignancies
Strahlentherapie und Onkologie (2022)
-
Technology-enabled activation of skin cancer screening for hematopoietic cell transplantation survivors and their primary care providers (TEACH)
BMC Cancer (2020)
-
Reproductive issues in patients undergoing Hematopoietic Stem Cell Transplantation: an update
Journal of Ovarian Research (2016)
-
Frequent induction of chromosomal aberrations in in vivo skin fibroblasts after allogeneic stem cell transplantation: hints to chromosomal instability after irradiation
Radiation Oncology (2015)
-
Use of azathioprine for graft-vs-host disease is the major risk for development of secondary malignancies after haematopoietic stem cell transplantation: a nationwide population-based study
British Journal of Cancer (2015)