Abstract
Background:
Peptide receptor radionuclide therapy (PRRT) is an established treatment for patients with metastatic neuroendocrine tumours (NETs), although which factors are associated with an improved overall survival (OS) remains unclear. The primary aim of this study is to determine to what extent a radiological response to 90Y-DOTATOC/90Y-DOTATATE PRRT is associated with an improved OS. The association of biochemical and clinical response to OS were assessed as secondary outcome measures.
Methods:
A retrospective analysis was conducted on 57 patients: radiological response was classified using RECIST criteria, biochemical response was classified using WHO criteria and clinical response was assessed subjectively. Responses were recorded as positive response (PR), stable disease (SD) or progressive disease (PD), and survival analysed.
Results:
Radiological response was achieved in 71.5% (24.5% PR, 47% SD) and was associated with a greater OS (51 and 56 months, respectively), compared with PD (18 months). A biochemical or clinical response post PRRT were not associated with a statistically significant improvement in OS. However, when combined with radiological response a survival benefit was observed according to the number of outcomes (radiological, biochemical, clinical), in which a response was observed. Mild haematological toxicity was common, renal toxicity was rare.
Conclusion:
In patients with progressive metastatic NETs receiving 90Y-DOTATOC/90Y-DOTATATE PRRT, a radiological response with either a PR or a SD post therapy confers a significant OS benefit.
Similar content being viewed by others
Main
Neuroendocrine tumours (NETs), occurring with a prevalence of 2–4 per 100 000 people, are usually slow growing tumours although many patients present with evidence of metastatic spread to lymph nodes or liver. These tumours not only produce a variety of hormones, giving rise to the characteristic carcinoid syndrome symptoms, but also express cell-surface peptide receptors, which may be useful for diagnostic and therapeutic purposes (Kulke and Mayer, 1999; Baudin 2007).
As curative surgical resection is an option in only a minority of patients, the main goals of the treatment are to provide symptom relief, retard tumour progression and improve overall survival (OS). A number of therapeutic modalities are available, including somatostatin analogues (SSA), interferon-α, hepatic artery embolisation, cytoreductive surgery or chemotherapy (Modlin et al, 2008). For patients with inoperable metastatic NETs, who have progressive disease (PD) or symptoms refractory to conventional medical therapy, peptide receptor radionuclide therapy (PRRT) is available, a treatment endorsed by the European Neuroendocrine Tumour Society (ENETS; Otte et al, 1998; Kwekkeboom et al, 2009).
PRRT primarily utilises one of two radioisotopes, 90Yttrium (90Y) or 177Lutetium (177Lu), attached to a SSA via the chelating agent DOTA. 90Yttrium may be delivered as [90Y-DOTA0,Tyr3] Octreotide (90Y-DOTATOC) or as the newer [90Y-DOTA0,Tyr3] Octreotate (90Y-DOTATATE).
Although no randomised, placebo-controlled trials using PRRT exist, PPRT with 90Yttrium-labelled SSAs has been shown to cause tumour regression and symptomatic benefit in the vast majority of patients (Waldherr et al, 2001, 2002; Kwekkeboom et al, 2005b; Imhof et al, 2011). Significant haematological toxicity occurs in only 10–20% of cases, although many patients have evidence of milder bone marrow suppression that may delay further treatment cycles. With use of reno-protective amino acid infusions, renal toxicity is uncommon.
We have previously demonstrated an improved OS in patients with metastatic NETs who derived a clinical (i.e., symptomatic) or radiological benefit from 131I-MIBG therapy (Nwosu et al, 2008). Thus, we sought to evaluate the efficacy, safety and toxicity of 90Yttrium-PRRT in patients with metastatic NETs and determine to what extent the radiological response to PRRT, as the primary outcome measure, was associated with OS. Furthermore, we noted the association of biochemical and clinical response to survival as secondary outcome measures, and determined the time course of bone marrow suppression/toxicity post PRRT.
Materials and Methods
Patients and study design
A retrospective review was performed on 67 patients (45 male, 22 female) with metastatic NETs who had received therapeutic 90Y-DOTATOC or 90Y-DOTATATE at the Department of Nuclear Medicine in the Royal Liverpool University Hospital between December 2003 and November 2012. The study was registered at the hospital audit department.
Case notes were retrieved for all 67 patients. Using these, along with the patient management systems, at both the Royal Liverpool University Hospital and University Hospital Aintree, Liverpool, the following information was recorded: patient demographics; date of diagnosis; time between diagnosis and first 90Yttrium-PRRT; number of 90Yttrium-PRRT treatments; primary tumour site; site of metastasis; previous treatments administered; symptoms pre- and post therapy; serum chromogranin A and 24 h urinary 5HIAA pre- and post therapy; imaging (CT/MRI) scans pre- and post therapy; and full blood count (FBC) and urea and electrolyte (U&E) results pre- and post therapy. Only those patients confirmed as having gastroenteropancreatic (GEP) or pulmonary NETs were included in the subsequent analysis.
Neuroendocrine tumours were confirmed in these patients by histological diagnosis; where this information was not available, the diagnosis was based upon elevated biochemical markers (including chromogranin A and/or 24 h urinary 5HIAA) plus cross-sectional (CT/MRI) and functional imaging supportive of a NET (positive uptake on OctreoScan/DOTATATE scans) (Covidien; Petten, The Netherlands).
Selection of patients for targeted therapy
All patients were selected for 90Yttrium-PRRT following a consensus decision made at the supra-regional Neuroendocrine Tumour Multi Disciplinary Team meeting; an ENETS-accredited service delivered by the University Hospital Aintree and Royal Liverpool University Hospital.
All those selected for 90Yttrium-PRRT had evidence of PD in 6–12 months before receiving therapy. Of those selected for treatment, 45% were referred for clinically PD refractory to optimal medical treatment, 33% demonstrated radiological progression and 22% had mixed symptomatic and radiological progression. Each patient was scheduled to receive three individual 90Y-DOTAOC or 90Y-DOTATATE treatments as part of a complete therapy cycle.
Administration protocol
Before therapy, baseline haematology (FBC) and renal function (U&Es) were assessed. Therapeutic long- and short-acting octreotide was stopped at least 4 weeks and 48 h, respectively, before delivery of radionuclide therapy and was not resumed until at least 7 days after. To reduce the renal uptake of the radiolabelled octreotide, an amino acid infusion (25 g lysine and 25 g arginine; Rolleman et al, 2003) and Gelofusin (Vegt et al, 2006) were co-administered alongside the 5 GBq (100–200 μg) of 90Y-DOTATATE or 90Y-DOTATOC. Patients were admitted overnight after receiving the treatment. The usual therapeutic cycle consisted of three individual dose of 90Y-DOTATATE or 90Y-DOTATOC being administered to each patient at 10–12 weekly intervals.
Patients were administered 90Y-DOTATOC before April 2008; from this date onwards patients were treated with 90Y-DOTATATE. This meant that those patients whose therapy cycle crossed this date would have received treatment with both analogues. The change in treatment analogue was not a clinical decision but an issue with supply of the drug.
Assessing response and toxicity
Radiological, biochemical and clinical responses to therapy were assessed between 3 and 12 months following completion of the final 90Yttrium treatment. Where multiple results for these outcomes were available due to serial investigations, those closest to the last treatment date were used. Because of the progressive nature of the patients’ disease before 90Yttrium-PRRT, a response to therapy for each outcome (radiological, biochemical and clinical) was deemed to have occurred if the patient exhibited disease regression (positive response, PR) or disease stabilisation (stable disease, SD), that is, ‘disease control’.
Radiological response
Radiological response was assessed using the RECIST criteria (Eisenhauer et al, 2009). A PR to therapy was deemed to have occurred if patients demonstrated either a complete or partial response to therapy (>30% decrease in the sum of the longest diameter for all target lesions) as determined by RECIST criteria.
Progressive disease was taken as at least a 20% increase in the sum of the longest diameter of target lesions or the appearance of one or more new lesions. Stable disease was when there was neither sufficient tumour shrinkage to qualify for PR, nor sufficient increase to qualify for PD.
Biochemical response
Biochemical response was assessed, in accordance with WHO criteria, by analysing changes in serum chromogranin A or 24 h urinary 5HIAA concentrations pre- and post-therapy as follows: PR, complete normalisation of, or a >50% reduction in previously elevated serum chromogranin A or 24 h urinary 5HIAA levels; PD, a 25% increase in previously elevated serum chromogranin A or 24 h urinary 5HIAAs; SD, neither sufficient reduction to qualify for a PR nor a sufficient increase to qualify for PD. Fasting serum chromogranin A concentration has been shown to be an independent prognostic factor in patients with metastatic NETs (Arnold et al, 2008).
Clinical (symptomatic) response
A positive clinical response was defined as patients reporting either complete resolution or a decrease in the intensity of symptoms. These symptoms included: abdominal pain, flushing, bloating, diarrhoea, weight loss, fatigue, sweats, breathlessness, vomiting, haemoptysis and anorexia. Progressive Disease was reported if an increase in symptom intensity/frequency occurred. Stable Disease was recorded following no change in symptoms.
Toxicity
Toxicity was assessed using the National Cancer Institute Common Terminology of Adverse Events v 4.0 (CTCAE). These criteria were applied to results from FBCs and renal function tests (U&Es) taken every 2 weeks over a 10-week period following each individual 90Yttrium treatment.
Statistical analysis
Survival outcomes were plotted using the Kaplan–Meier method. In addition, we recorded the survival probabilities at 6, 12, 24 and 48 months. Log-rank tests were applied to test for evidence of a difference in survival curves between response groups. OS is quoted as median (months) with accompanying 95% confidence interval. Multivariable Cox regression modelling was used to compare response groups adjusting for baseline differences in age and serum chromogranin A concentration. We limited the number of variables examined in a multivariable model to 3 in order to satisfy the 10 events per variable rule of thumb for stable parameter estimates (Van Belle, 2002). As a result, we did not adjust for other variables that may have prognostic relevance such as proliferative (Ki67) index. Fisher’s exact tests were used to assess the association between the observed clinical, biochemical and radiological responses. All results were considered statistically significant at the 5% level; no corrections were made for multiple comparisons. Statistical analysis was undertaken using Stata version 12.0 (StataCorp. 2011. Stata Statistical Software: Release 12. StataCorp LP, College Station, TX, USA).
Results
Patient characteristics
Of the 67 patients, 61 patients were confirmed as having GEP or pulmonary NETs and were included in the subsequent analysis. Those excluded had diagnoses including phaeochromocytomas, paragangliomas and medullary thyroid cancers. Of those identified as having a GEP or pulmonary NET, a further four patients were excluded due to a lack of sufficiently completed records giving a total 57 patients.
The mean age at the time of diagnosis was 53.7 years and therapy 57.4 years. The median time between diagnosis and treatment was 27 months (range 4–237).
The most common presenting symptoms were flushing, diarrhoea and abdominal pain (54%, 47% and 30%, respectively).
Primary disease sites included the small bowel (35%), pancreas (26%) appendix (7%) and lung (3.5%). The primary site could not be identified in 23% (Table 1). A histological diagnosis was available in 40 out of 57 patients: 35 patients had confirmed carcinoid disease and five had pancreatic NETs (three insulinomas, one glucagonoma and one somatostatinoma). The proliferative index, Ki67s, was available in 24out of 40 patients (13 Grade 1, 11 Grade 2, 0 Grade 3).
All patients had metastatic disease, with the most common location being the liver (93%), followed by regional lymph nodes (28%) and bone (19%). The vast majority of patients had already received other treatments for their condition including surgical intervention (44%), chemotherapy (17.5%) and interferon-α (10.5%; Table 1).
Of these 57 patients, 15 were treated solely with 90Y-DOTATOC and 33 were treated solely with 90Y-DOTATATE. Nine patients’ therapy cycle crossed the date at which the treatment analogue was changed and as a result had 1 or 2 treatments with 90Y-DOTATOC; 90Y-DOTATATE was used to complete the therapy cycle.
All patients were due to have three individual treatments with 90Y-DOTATOC or 90Y-DOTATATE as part of a therapy cycle: 36 patients received all three treatments, 12 received two treatments and 9 received only one treatment. The reasons for not completing the therapy cycle included: patient choice; treatment side effects; patient fitness and death.
Response to therapy
In all, 57 patients received a total of 141 treatments of 90Y-DOTATOC/DOTATATE (median 3, range 1–3). Information on radiological response was available for 49 out of 57 patients, on biochemical response for 35 out of 57 patients and on clinical response for all patients. A radiological response was observed in 71.5% of patients post therapy (PR 24.5%, SD 47%) with the remaining 28.5% having evidence of PD. A biochemical response was observed in 69% of patients (PR 23%, SD 46%) with 31% having PD and a clinical response was observed in 86% (PR 49%, SD 37%) with PD in 14%. The Fisher’s exact tests were unable to demonstrate an association between any response types (P>0.1), for example, a positive radiological response was not necessarily associated with a positive clinical response.
Overall Survival
During a median follow up of 32 months (range 4–104), 31 (54.3%) patients died with a median survival time of 46 months (95% CI: 34, 56) from the date of first 90Yttrium PRRT and 95 months (95% CI: 70,120) from date of diagnosis.
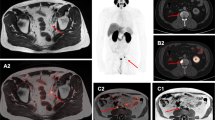
The Kaplan–Meier curves demonstrate that those who had a radiological response to therapy (PR or SD), thereby achieving ‘disease control’, had a significantly improved survival compared to those with disease progression (51 (34, −) and 56 (34, −) months vs 18 (10, −) months; P=0.0020; Table 2 and Figure 1). We also examined the probability of survival according to the radiological response at fixed time points (6, 12, 24 and 48 months) post therapy (Table 3). Interestingly, no additional survival benefit was demonstrated in those patients who had a PR vs SD radiologically post therapy (Figure 1).
Similarly, there was no statistically significant survival benefit between patients who reported a PR or SD clinically post therapy (Figure 2). Although it would appear that individuals with a clinical response post therapy (PR or SD) have a clear survival advantage over those demonstrating PD clinically, the actual difference in OS times were not statistically significant (Table 2 and Figure 2), P=0.2208, possibly owing to the few patients (n=8) in the PD category.
Biochemical response to therapy also appeared not to have a significant impact upon OS. However, when biochemical and clinical responses were combined with radiological response, an improved OS was observed according to the number of outcomes (radiological, biochemical, clinical) in which ‘disease control’ (PR or SD) was achieved (Table 2 and Figure 3).
Hazard ratios of survival
For the purposes of regression analysis, patients classified as PR or SD were pooled in order to limit the number of parameters estimated. In the univariate Cox regression analysis, higher baseline serum chromogranin A concentration was found to be associated with an increased hazard of death (for a 100 pmol l−1 change: HR 1.18, 95% CI 1.06, 1.30; P=0.0020; Table 4). Being a radiological responder was demonstrated to considerably reduce the hazard of death (HR 0.24, 95% CI 0.10, 0.57; P=0.0010). Age, biochemical or clinical response group were not found to affect survival in univariate analysis (P>0.05).
When we included both baseline serum chromogranin A concentration and age in a multivariable Cox regression model alongside radiological response group, the hazard ratios were virtually unchanged compared with those in the univariate analyses (Table 4). Neither clinical nor biochemical response group added sufficient information for inclusion in this multivariable model, as measured by Akaike’s Information Criteria. In other attempted multivariable models, after adjusting for baseline serum chromogranin A concentration and age, neither clinical or biochemical response group were found to affect survival (not shown).
Effect of primary tumour site on survival
The effect of primary disease site on OS was also assessed. Tumours were sub-grouped into those arising from the small and large bowel, pancreas and unknown primary site. There was no correlation between tumour site and patient survival post 90Yttium PRRT. However, trends are visible with individuals whose primary disease site could not be identified typically having a shorter survival.
Effect of number of treatments of PRRT on survival
An additional analysis into the effect of the number of 90Yttrium PRRT treatments administered showed a trend of increasing OS with each additional 90Yttrium treatment (16 vs 20 vs 51 months for treatment 1, 2 and 3, respectively), however, this was not statistically significant (P=0.081). Similarly, the number of 90Yttrium treatments administered did not have a statistically significant effect on whether patients recorded PD, SD or PR post therapy.
Toxicity
Haematological/renal toxicity
Overall, a total of 51 individuals had at least one episode of anaemia during the 10-week period following one of their treatments. In all, 43 individuals experienced at least one episode of leucoponaeia and 38 developed thrombocytopaenia. Only six patients developed renal impairment after treatment (5 Grade 1, 1 Grade 2). Table 5 shows the number of patients experiencing haematological toxicity after each individual treatment and the grade of that toxicity reflecting its severity (graded using the NCI CTCAE criteria). This table shows that the proportion of people experiencing anaemia, leucopoenia or thrombocytopaenia increased with each subsequent treatment. The proportion of those with severe G3/4 toxicities increased between treatments 1 and 2 but decreased after treatment 3. Furthermore, the proportion of patients with multiple (⩾2) haematological toxicities increased over the course of the therapy cycle (55.3%, 58.2% and 86%, following treatments 1, 2 and 3, respectively). Following the final treatment, >50% of all patients had developed anaemia, leucopoenia and thrombocytopaenia (pancytopaenia). Figure 4 shows the temporal relationship of the haematological toxicities to the point at which treatment was administered. No patient died as a result of haematological or renal toxicity.
General
Patients experienced a number of other side effects including: lethargy (18.6%) nausea and vomiting (14%), weight loss (7%) and pain (7%). No patient had a carcinoid crisis following treatment or any acute reactions during infusion of the radionuclide therapy.
Discussion
We observed positive radiological, biochemical and clinical responses in 24.5%, 23% and 49% of patients, respectively, although if SD was included, an overall response to therapy resulting in ‘disease control’ was achieved in 71.5%, 69% and 86% of patients, respectively. The results of this study clearly demonstrate that patients who have a radiological response to PRRT with 90Y-DOTATOC or 90Y-DOTATATE have a significant improvement in OS. This OS benefit is still observed after adjustment for baseline differences between individuals for age and serum chromogranin A concentrations. We also demonstrate a predictable time course for myelosuppresion following administration of therapy and with the use of reno-protective amino acid administration renal toxicity was observed only rarely.
Differences in various factors including study design, therapy dosage, criteria used to determine response and follow-up intervals make direct comparisons between studies difficult. In an early phase II study of 41 patients treated with 90Y-DOTATOC, Waldherr et al (2001) found that 85% had ‘disease control’ with only 15% of patients with PD and that 83% of patients had significant clinical benefit. Similarly, Forrer et al (2006) previously reported the response in 116 patients treated with 90Y-DOTATOC and noted disease control in 89% of patients (27% PR; 62% SD), whereas 83% had a reduction in clinical symptoms . In an early phase I study of 58 patients with advanced GEP-NETs, Valkema et al (2006) reported that 57% of patients demonstrated some improvement in their disease status. Imhof et al (2011) reported outcome in 1109 patients after a phase II study involving Y90-DOTATOC and showed clinical, biochemical and radiological responses in 30%, 15% and 35%, respectively. More recently, it has been suggested that DOTATATE therapy may be more effective, as DOTATATE has a nine-fold higher affinity for somatostatin subtype 2 receptors than DOTATOC. Cwikla et al (2010) examined response of Y90-DOTATATE therapy in 60 patients and demonstrated clear efficacy with high rates of clinical or radiological response. Our small sample size precluded a comparison between those patients treated with 90Y-DOTATATE or 90Y-DOTATOC.
We did not necessarily observe that responses were consistent across each outcome, for example, a radiological response did not correlate with a clinical response. This may be due to the inadequacies of the current criteria used to classify response of NETs to targeted therapy. Neuroendocrine tumours, particularly when cystic, may enlarge post therapy due to tumour necrosis and inflammatory change. Thus, current criteria may classify a PR as PD. Alternative criteria may be more appropriate in the specific context of NETs (Benjamin et al, 2007). It has also been proposed that cross-sectional imaging using CT/MRI scans may not be the best imaging modality to assess treatment response and that functional PET/OctreoScans may be more informative (Haug et al, 2010).
As with the findings of Imhof et al (2011), we demonstrate that a radiological response to therapy was associated with a longer survival. Importantly, when comparing the survival using the three individual responses of PR, SD and PD there were no significant differences in survival between those with a PR or SD radiologically (Figure 1 and Table 2). This phenomenon was also reported by Cwikla et al (2010).
Significantly, however, we observed that the benefit in OS was clearly related to the number of outcomes in which a response to therapy was observed, such that the greatest benefit was seen in those patients who had multiple responses achieving ‘disease control’ in two or three of clinical, biochemical and radiological outcomes (Figure 3).
The number of treatments administered appeared to positively influence OS with those receiving three treatments demonstrating a longer OS compared with those receiving two or one, although this was not statistically significant. Caution should also be taken when interpreting these results as confounding factors, such as baseline health, disease progression and death, which lead to patient withdrawal from the treatment cycle, are not accounted for. To fully ascertain the effect of the number of radionuclide therapies administered on survival, further randomised studies are required.
An important variation that affects response rates and survival is the point during the course of disease at which therapy is administered. An objective tumour response after PRRT is more likely to be observed in patients with PD, hence, our inclusion in this study of patients with PD or refractory disease at the time of therapy. However, Kwekkeboom et al (2008) demonstrated a shorter median OS in those patients with a poor performance score and those with extensive liver involvement, suggesting that targeted therapy should be administered at an earlier point in the evolution of disease. The relatively late introduction of PRRT during the clinical course of disease in our patients may also explain why primary disease site had no effect on response to therapy and OS post PRRT. However, it should also be noted that the relatively low number of subjects within this study may have precluded any meaningful comparison.
Overall, renal toxicity was rare, reflecting the benefits of using a reno-protective infusion of amino acids, whereas the development of mild G1 and G2 haematological toxicity was almost universal. The mean number of patients experiencing severe G3/4 haematological toxicity over the course of the therapy cycle (16%) was comparable to results obtained in other studies (Cwikla et al, 2010).
An important point to note in this study is that a relatively large proportion of individuals demonstrated a normocytic anaemia before commencing treatment (42% pre-treatment 1, 50% pre-treatment 2, 55% pre-treatment 3); presumably secondary to chronic disease. All of these patients developed a worsening of their anaemia following treatment, although the grade of the anaemia did not alter in severity according to the NCI CTCAE criteria. The peak of the acute toxic effects of treatment tended to occur 6–10 weeks post therapy. In addition, a cumulative toxic effect occurred such that the number of patients developing multiple (⩾2) haematological toxicities increased over the course of the therapy cycle (55.8%, 58.2% and 86%, following treatment 1, 2 and 3, respectively). Most cases of myelosuppression resolved spontaneously and no patients died as a result of renal or haematological toxicity.
There remain many questions regarding the application of targeted therapy to patients with metastatic NETs. First, we are unable to draw firm conclusions on the effect of our therapy on OS from this, or indeed from any other published study, because randomised, controlled trials with radiolabelled SSAs have not been performed (Kwekkeboom et al, 2005a, 2005b). The optimal timing of the intervention with targeted therapy is uncertain with some advocating its use earlier in the course of disease (Kwekkeboom et al, 2005b; Kwekkeboom et al, 2008). Combination PRRT using 90Yttrium- and 177Lutetium- labelled SSAs is also a potential therapeutic consideration with the few studies conducted thus far showing increased response rates and survival times (Villard et al, 2012).
The retrospective nature of our analysis led to incomplete data availability and heterogeneity in the data set. We chose radiological response as the primary outcome measure, as it can be measured most objectively using well-validated criteria. For biochemical response, one of the two secondary outcome measures, incomplete biochemical data (available on 35 out of 57 patients), and the interference of various drugs (e.g., proton pump inhibitors; Mosli et al, 2012) and renal function (Bech et al, 2012) on serum chromogranin A concentrations, makes serial changes less reliable as an objective measure of response.
Structured clinical questionnaires such as the European Organisation for Research and Treatment of Cancer questionnaire (EORTC QLQ-C30) are not used as a component of clinical data collection during our follow-up clinics, because of their lack of specificity for NETs. As a result, clinical response was assessed subjectively with its inherent limitations. It should also be noted that the only validated disease-specific quality-of-life score questionnaire for patients with NETs, EORTC QLQ-NET21, was not available at the time clinical data were recorded for the majority patients (Davies et al, 2006). In the absence of such clinical questionnaires, this information regarding symptoms intensity/frequency reported at follow-up clinic represents the most reliable from data available to us to assess clinical response to therapy. Despite these limitations, data on clinical and biochemical response, when analysed in conjunction with radiological response to determine the total number of positive outcomes (one, two or three) to PRRT, were able to provide useful prognostic information regarding differences in survival (Figure 3).
The need for improved standardisation and validated end points of clinical trials for NETs has been recognised (Kulke et al, 2011) and the results of further studies should include a prospective detailed quality-of-life assessment, which can inform patients’ treatment selection, determine resource allocation and influence healthcare policy (Ramage et al, 2011).
Nonetheless, on the basis of this analysis, we demonstrate that 90Y-DOTATOC and 90Y-DOTATATE are effective treatments that can improve survival in patients with progressive or symptomatic metastatic NETS and this benefit appears to be similar in those whose disease is stabilised to those whose disease regresses.
Change history
16 April 2013
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Arnold R, Wilke A, Rinke A, Mayer C, Kann PH, Klose KJ, Scherag A, Hahmann M, Müller HH, Barth P (2008) Plasma chromogranin A as marker for survival in patients with metastatic endocrine gastroenteropancreatic tumors. Clin Gastroenterol Hepatol 6: 820–827
Baudin E (2007) Gastroenteropancreatic endocrine tumors: clinical characterization before therapy. Nat Clin Pract Endocrinol Metab 3: 228–239
Bech PR, Ramachandran R, Dhillo WS, Martin NM, Bloom SR (2012) Quantifying the effects of renal impairment on plasma concentrations of the neuroendocrine neoplasia biomarkers chromogranin A, chromogranin B, and cocaine- and amphetamine-regulated transcript. Clin Chem 58: 941–943
Benjamin RS, Choi H, Macapinlac HA, Burgess MA, Patel SR, Chen LL, Podoloff DA, Charnsangavej C (2007) We should desist using RECIST, at least in GIST. J Clin Oncol 25: 1760–1764
Cwikla JB, Sankowski A, Seklecka N, Buscombe JR, Nasierowska-Guttmejer A, Jeziorski KG, Mikolajczak R, Pawlak D, Stepien K, Walecki J (2010) Efficacy of radionuclide treatment DOTATATE Y-90 in patients with progressive metastatic gastroenteropancreatic neuroendocrine carcinomas (GEP-NETs): a phase II study. Ann Oncol 21: 787–794
Davies AH, Larsson G, Ardill J, Friend E, Jones L, Falconi M, Bettini R, Koller M, Sezer O, Fleissner C, Taal B, Blazeby JM, Ramage JK EORTC Quality of Life Group (2006) Development of a disease-specific quality of life questionnaire module for patients with gastrointestinal neuroendocrine tumours. Eur J Cancer 42: 477–484
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S, Mooney M, Rubinstein L, Shankar L, Dodd L, Kaplan R, Lacombe D, Verweij J (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 45: 228–247
Forrer F, Waldherr C, Maecke HR, Mueller-Brand J (2006) Targeted radionuclide therapy with 90Y-DOTATOC in patients with neuroendocrine tumors. Anticancer Res 26: 703–707
Haug AR, Auernhammer CJ, Wängler B, Schmidt GP, Uebleis C, Göke B, Cumming P, Bartenstein P, Tiling R, Hacker M (2010) 68Ga-DOTATATE PET/CT for the early prediction of response to somatostatin receptor-mediated radionuclide therapy in patients with well-differentiated neuroendocrine tumors. J Nucl Med 51 (9): 1349–1356
Imhof A, Brunner P, Marincek N, Briel M, Schindler C, Rasch H, Macke H, Rochlitz C, Muller-Brand J, Walter M (2011) Response, survival, and long-term toxicity after therapy with the radiolabeled somatostatin analogue [90Y-DOTA]-TOC in metastasized neuroendocrine cancers. J Clin Oncol 29: 2416–2423
Kulke MH, Mayer RJ (1999) Carcinoid tumors. N Engl J Med 340: 858–868
Kulke MH, Siu LL, Tepper JE, Fisher G, Jaffe D, Haller DG, Ellis LM, Benedetti JK, Bergsland EK, Hobday TJ, Van Cutsem E, Pingpank J, Oberg K, Cohen SJ, Posner MC, Yao JC (2011) Future directions in the treatment of neuroendocrine tumors: consensus report of the national cancer institute neuroendocrine tumor clinical trials planning meeting. J Clin Oncol 29: 934–943
Kwekkeboom DJ, de Herder WW, Kam BL, van Eijck CH, van Essen M, Kooij PP, Feelders RA, van Aken MO, Krenning EP (2008) Treatment with the radiolabeled somatostatin analog [177Lu-DOTA0,Tyr3]octreotate: toxicity, efficacy, and survival. J Clin Oncol 26: 2124–2130
Kwekkeboom DJ, Krenning EP, Lebtahi R, Komminoth P, Kos-Kudła B, de Herder WW, Plöckinger U and the Mallorca Consensus Conference participants (2009) ENETS Consensus Guidelines for the Standards of Care in Neuroendocrine Tumors: Peptide Receptor Radionuclide Therapy with Radiolabeled Somatostatin Analogs. Neuroendocrinology 90: 220–226
Kwekkeboom DJ, Mueller-Brand J, Paganelli G, Anthony LB, Pauwels S, Kvols LK, O’Dorisio TM, Valkema R, Bodei L, Chinol M, Maecke HR, Krenning EP (2005a) Overview of results of peptide receptor radionuclide therapy with 3 radiolabeled somatostatin analogs. J Nucl Med 46 (Suppl 1): 62S–66SS
Kwekkeboom DJ, Teunissen JJ, Bakker WH, Kooij PP, de Herder WW, Feelders AA, van Eijck CH, Esser J, Kam BL, Krenning EP (2005b) Radiolabelled somatostatin analog [177Lu-DOTA0, Tyr3]octreotate in patients with endocrine gastroenteropancreatic tumors. J Clin Oncol 23: 2754–2762
Modlin IM, Oberg K, Chung DC, Jensen RT, de Herder WW, Thakker RV, Caplin M, Delle Fave G, Kaltsas GA, Krenning EP, Moss SF, Nilsson O, Rindi G, Salazar R, Ruszniewski P, Sundin A (2008) Gastroenteropancreatic neuroendocrine tumours. Lancet Oncol 9: 61–72
Mosli HH, Dennis A, Kocha W, Asher LJ, Van Uum SH (2012) Effect of short-term proton pump inhibitor treatment and its discontinuation on chromogranin A in healthy subjects. J Clin Endocrinol Metab 97: E1731–E1735
Nwosu AC, Jones L, Vora J, Poston GJ, Vinjamuri S, Pritchard DM (2008) Assessment of the efficacy and toxicity of (131)I-metaiodobenzylguanidine therapy for metastatic neuroendocrine tumours. Br J Cancer 98: 1053–1058
Otte A, Mueller-Brand J, Dellas S, Nitzsche EU, Herrmann R, Maecke HR (1998) Yttrium-90-labelled somatostatin-analogue for cancer. Lancet 351: 417–418
Ramage JK, Ahmed A, Ardill J, Bax N, Breen DJ, Caplin ME, Corrie P, Davar J, Davies AH, Lewington V, Meyer T, Newell-Price J, Poston G, Reed N, Rockall A, Steward W, Thakker RV, Toubanakis C, Valle J, Verbeke C, Grossman AB UK and Ireland Neuroendocrine Tumour Society (2011) Guidelines for the management of gastroenteropancreatic neuroendocrine (including carcinoid) tumours (NETs). Gut 61: 6–32
Rolleman E, Valkema R, de Jong M, Kooij P, Krenning E (2003) Safe and effective inhibition of renal uptake of radiolabelled octreotide by a combination of lysine and arginine. Eur J Nucl Med Mol Imaging 30: 9–15
Valkema R, Pauwels S, Kvols LK, Barone R, Jamar F, Bakker WH, Kwekkeboom DJ, Bouterfa H, Krenning EP (2006) Survival and response after peptide receptor radionuclide therapy with [90Y-DOTA0,Tyr3]octreotide in patients with advanced gastroenteropancreatic neuroendocrine tumors. Semin Nucl Med 36: 147–156
Van Belle Gerald (2002) Statistical rules of thumb. John Wiley and Sons: New Jersey
Vegt E, Wetzels JF, Russel FG, Masereeuw R, Boerman OC, van Eerd JE, Corstens FH, Oyen WJ (2006) Renal uptake of radiolabeled octreotide in human subjects is efficiently inhibited by succinylated gelatin. J Nucl Med 47: 432–436
Villard L, Romer A, Marincek N, Brunner P, Koller MT, Schindler C, Ng QK, Mäcke HR, Müller-Brand J, Rochlitz C, Briel M, Walter MA (2012) Cohort study of somatostatin-based radiopeptide therapy with [(90)Y-DOTA]-TOC versus [(90)Y-DOTA]-TOC plus [(177)Lu-DOTA]-TOC in neuroendocrine cancers. J Clin Oncol 30: 1100–1106
Waldherr C, Pless M, Maecke HR, Haldemann A, Mueller-Brand J (2001) The clinical value of [90Y-DOTA]-D-Phe1-Tyr3-octreotide (90Y-DOTATOC) in the treatment of neuroendocrine tumours: a clinical phase II study. Ann Oncol 12: 941–945
Waldherr C, Pless M, Maecke HR, Schumacher T, Crazzolara A, Nitzsche EU, Haldemann A, Mueller-Brand J (2002) Tumor response and clinical benefit in neuroendocrine tumors after 7.4 GBq (90)Y-DOTATOC. J Nucl Med 43: 610–616
Acknowledgements
We thank Daniel Lythgoe for his statistical support.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Vinjamuri, S., Gilbert, T., Banks, M. et al. Peptide receptor radionuclide therapy with 90Y-DOTATATE/90Y-DOTATOC in patients with progressive metastatic neuroendocrine tumours: assessment of response, survival and toxicity. Br J Cancer 108, 1440–1448 (2013). https://doi.org/10.1038/bjc.2013.103
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2013.103
Keywords
This article is cited by
-
Prediction of [177Lu]Lu-DOTA-TATE therapy response using the absorbed dose estimated from [177Lu]Lu-DOTA-TATE SPECT/CT in patients with metastatic neuroendocrine tumour
EJNMMI Physics (2024)
-
Active bone marrow S-values for the low-energy electron emitter terbium-161 compared to S-values for lutetium-177 and yttrium-90
EJNMMI Physics (2022)
-
Peptide receptor radionuclide therapy for GEP-NET: consolidated knowledge and innovative applications
Clinical and Translational Imaging (2021)
-
PRRT: identikit of the perfect patient
Reviews in Endocrine and Metabolic Disorders (2021)
-
Availability of both [177Lu]Lu-DOTA-TATE and [90Y]Y-DOTATATE as PRRT agents for neuroendocrine tumors: can we evolve a rational sequential duo-PRRT protocol for large volume resistant tumors?
European Journal of Nuclear Medicine and Molecular Imaging (2020)