Key Points
-
Provides a way for PCTs to use locally available data in order to undertake an equity audit.
-
Demonstrates the impact of practice location and population demographics on uptake and usage of dental care.
-
Practices and services which are located in more deprived areas will facilitate greater uptake from the local population.
-
Undertaking an equity audit will aid PCTs to reduce inequalities in oral health.
Abstract
Aim To use nationally available data sets to undertake an equity audit to support the targeting of resources to meet the needs of patients from deprived communities, in areas where levels of poor oral health remain higher than the rest of the population as a whole.
Methods Postcodes of 224,107 patients in County Durham were matched to Lower Super Output Areas (LSOA) for each practice. Deprivation scores were identified for each LSOA. The postcode of dental practices (59) was matched to the LSOA and the practice population divided into quintiles from the most to the least deprived areas.
Results Results indicated that the more deprived the area in which a dental practice was located, the greater the proportion of the practice population accessing care from the most deprived quintile. The size of the practice alone was not directly related to meeting the needs of a more deprived population.
Conclusions The methodology used in this study can be used to identify inequalities and inequities in oral health in different areas. In the audit area improving access to dental services for those in most need, was best tackled by targeted investment into dental practices located in deprived communities. Audits are recommended to insure a fare distribution of resources to meet local population needs.
Similar content being viewed by others
Introduction
For many years the NHS in England has worked towards reducing inequalities in health and inequities in access to service provision1,2 this specifically includes oral health.3 NHS Oral health service provision had, until the introduction of the new dental contract in 2006, lacked the contractual flexibility to allow primary care organisations to influence the location of general dental service provision by independent contractors.4
For nearly half a century, from 1948 to 2006, independent dental contractors were able to establish NHS dental practices where they wanted to, without any restriction on the location of practices. This often resulted in numbers of practices being located in commercial high street type locations, without any need to take account of the health needs of the local population.
Evidence from national surveys of oral health in England have shown a consistent improvement in the oral health of the population since the first national survey in 1968, when dental disease was almost universally experienced by all of the population.5 Although subsequent surveys have shown that there have been significant improvements in oral health since the 1960s, both national and local studies in the North East have shown that dental disease experience remains highest amongst the poorest sections of society.
There is a clear relationship between increasing levels of deprivation in the population and increasing levels of dental disease experience.6,7,8 To tackle inequalities in oral health and inequity in service provision, dental practices need to be located where they will effectively provide services for patients from deprived populations.
Health equity audits provide a methodology to identify how fairly healthcare resources are deployed within an area to meet the needs of the population; this will then impact upon health inequalities. Resources should not just be deployed evenly across a community, but higher levels of resources and investment should be made in those areas where the populations have the greatest needs.9 Primary care trusts (PCTs) have a key role in undertaking health equity audits, in order to inform their investment programmes. The overall aim of an equity audit is to demonstrate that resources are being deployed appropriately to meet the healthcare needs of their populations and where they are not, inform a redeployment programme to reduce inequities in service provision and hence reduce inequalities in health.10,11
The pre-2006 freedom to establish NHS dental practices in any location based on demand rather than need can be seen as an example of the inverse care law, first described by John Tudor Hart in the early 1970s. It states that 'the availability of good medical care tends to vary inversely with the need for it in the population served'.12 Jones13 in 2001 demonstrated an inverse care law operating in dentistry where registration and lapsed rates for children were significantly associated with social deprivation. Those areas with the highest levels of social deprivation had lower levels of registration. Landes et al.14 in 2004 reported that there was no correlation between increasing dental needs in English health authorities and increased spending on oral health, but there was a correlation between increased registration rates and higher spending in those authorities classified as mixed economy, services and education and as most prosperous. More resources did not necessarily follow population needs.
The latest national guidance expects primary care organisations to meet all the reasonable oral health needs of their populations. Additionally it sets the NHS the challenge of not only improving oral health but moreover addressing health inequalities.15
To undertake an equity audit it is necessary to measure deprivation amongst populations. The method currently in most widespread use in England is the Index of Multiple Deprivation (IMD) 2007.16 The IMD brings together 37 different indicators which cover specific aspects or dimensions of deprivation: income, employment, health and disability, education, skills and training, barriers to housing and services, living environment and crime. These are weighted and combined to create the overall IMD 2007. It identifies levels of deprivation in small areas called lower super output areas (LSOAs). Each area contains on average 1,500 people. In England there are 32,482 LSOAs. The higher the IMD score, the greater the level of deprivation associated with the population living in the LSOA.
This equity audit was undertaken in County Durham which has a population of around 500,000 people living in an area of 862 square miles, 57% of the population live in urban areas, 34% in rural urban fringe and 9% in strictly rural areas.17 County Durham is one of the poorest counties in England; 31% of LSOAs are within the fifth most deprived in England.18 The distribution of the LSOAs divided into national quintiles in Durham is shown in Table 1.
The aim of this equity audit was to identify specific target locations where resources in dental services should be invested to best meet the needs of patients from deprived communities where levels of oral disease remain higher than the rest of the population as a whole, and so aid in ensuring a fare distribution of health care resources.
Methods
The Business Services Agency provided a data set containing the postcodes for all the unique patients seen at each individual dental practice address for independent contractors providing general dental services in County Durham in the North East of England during 2008/09.
The postcode for each individual patient who attended a dental practice during the study period was mapped to a LSOA in the North East of England.
The population attending an individual dental practice acted as the level at which the data was aggregated. The practice populations were divided into quintiles for levels of deprivation based upon IMD scores for all 32,482 LSOAs in England. Quintile 1 had the least deprived populations and Quintile 5 the most deprived populations. The level of deprivation for each dental practice location was identified from the postcode of the practice, identifying the relevant LSOA and the associated IMD score.
A correlation calculation was performed, comparing the proportion of practice populations resident in the most deprived quintile of LSOAs and the deprivation score for each practice location. A further correlation calculation was performed between practice population size and proportion of practice population resident in the most deprived quintile of the population.
Results
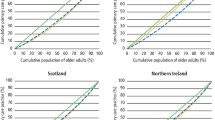
In 2008/09 the BSA identified 224,107 unique patients as having attended a dental practice in County Durham. Of these records, 210,621 (94%) had a postcode which could be mapped to a LSOA in the North East of England. The remaining 6% related to records where the postcode was either missing, incomplete or related to patients who lived outside the North East.
There were 59 practice locations identified as providing routine general dental services in the data set. The range of the number of unique patients seen at each individual practice location was 105 to 13,486. The range of the proportion of practice populations who were resident in LSOAs from the most deprived quintile was 2% to 98%. The distribution of the populations in each quintile for all dental practices in County Durham is shown in Table 1. The IMD score for individual dental practice locations ranged from 3.82 (least deprived) to 64.11 (most deprived). The proportion of practices located in each deprivation quintile is shown in Table 1.
The correlation of practice location against percentage of practice population resident in quintile 5 produced a coefficient of r2 = 0.77, demonstrating a strong relationship between the level of deprivation in the practice area and the proportion of the practice population living in the most deprived quintile. The more deprived the area in which a dental practice is located, the greater the proportion of the practice population accessing care living in the most deprived quintile.
Correlation between practice size and percentage resident in quintile 5 was r2 = 0.03, indicating that the correlation between practice size and the deprivation levels of the attending population was very weak.
The relationship between practice location, the proportion of practice populations from the most deprived quintile of the population and the size of practice, is shown in Figure 1.
Discussion
Our audit shows that practice location has a significant effect on who accesses a service. It suggests that people from the most deprived sections of our North East community will more favourably access services close to where they live. This is most likely to be influenced by the resources they have at their disposal with which to travel. In County Durham 31% of families have no car or van19 and 24% of children live in low income households as defined by the Child and Wellbeing Index 2009.20
The methodology used in this audit did not determine if patients lived in close proximity to the dental practice which they attended. It would be possible for people living in one deprived LSOA to attend a practice at some distance to where they lived, affecting the proportion of patients from deprived areas attending. However, as high levels of deprivation are associated with lower levels of car ownership and lower levels of income, there will be significant barriers to deprived people travelling some distance to access dental services and hence it is more likely that they were attending practices in close proximity to where they lived.
The data suggests that dental practices in the more deprived areas tend to be smaller and that merely increasing the practice size will not necessarily result in higher proportions of patients attending from deprived areas.
Although the IMD score demonstrates deprivation in an area, it is not an individual measure of poverty, so affluent people may live in predominantly poor areas with high IMD scores and conversely people from poor backgrounds may live in affluent areas. However, this study covers the entire NHS dental service in a population of half a million and would give a crude access rate of just under 50% of the population seeing an NHS dentist in a 12 month period, so the likelihood of significant artefacts distorting the figures is small.
Conclusions
Our equity audit suggests that practice location has an effect on the attending practice population in County Durham. Practices located in the poorest areas tended to be accessed by higher proportions of the population from deprived communities.
Results from our area demonstrate that inequalities and inequities in oral health, together with improving access to dental services for those in most need, can be best tackled by targeted investment into existing practices located in deprived communities, and/or commissioning new dental practices located in deprived areas.
It is the responsibility of PCTs to assess the needs of their populations in order to inform the commissioning process.21 By using this methodology PCTs can undertake an equity audit to determine if there is a fair distribution of resources to meet the differing healthcare needs of their local populations. The historical overhang of approximately half a century of freedom in the establishment of dental practices in any location has often led to inequitable development of services in areas of high demand rather than need, reinforcing the inverse care law.
Local commissioning of services now gives PCTs the opportunity to address inequalities in service. The data used in this paper is available for all areas in England and could be used to inform the commissioning processes by using this methodology to inform prioritisation of investments.
References
Department of Health. The NHS plan. London: Department of Health, 2000. http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4002960 (accessed 23 June 2010)
Department of Health. High quality care for all: the NHS next stage review. Final report. London: Department of Health, 2008. http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_085825 (accessed 23 June 2010)
Department of Health. World class commissioning: Improving dental access, quality and oral health. p 21. London: Department of Health, 2009. http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_093831 (accessed 23 June 2020)
Department of Health. NHS dental services in England. London: Department of Health, 2009. http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_096614 (accessed 23 June 2010)
Gray P G, Todd J E, Slack G L, Bulman J S . Adult Dental Health in England and Wales in 1968. pp 40–68. London: HMSO, 1970.
O'Brian M . Children's dental health in the United Kingdom 1993. pp 46–54. London: HMSO, 1994.
Todd J E, Lader D . Adult Dental Health 1988: United Kingdom. pp 73–85. London: HMSO, 1991.
Provart S C, Carmichael C . The relationship between caries, fluoridation and material deprivation in five-year-old children in Country Durham. Community Dent Health 1995; 12: 200–203.
Department of Health. Health equity audit – a guide for the NHS. London: Department of Health, 2003. http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4084138 (accessed 23 June 2010)
National Institute for Health and Clinical Excellence. Health equity audit - learning from practice briefing. London: National Institute for Health and Clinical Excellence, 2006. http://www.nice.org.uk/aboutnice/whoweare/aboutthehda/hdapublications/health_equity_audit__learning_from_practice_briefing.jsp (accessed 23 June 2010)
Health Development Agency. Making the case: health equity qudit. London: Health Development Agency, 2005. http://www.nice.org.uk/nicemedia/docs/Making%20the%20case-13-03.pdf (accessed 23 June 2010)
Hart J T. The inverse care law. Lancet 1971; 1: 405–412.
Jones C M. Capitation, registration and social deprivation in England. An inverse dental care law? Br Dent J 2001; 190: 203–206.
Landes D P, Adams G C, Whiston S . Distribution of NHS resources for children's dental care in general dental practice in England. Community Dent Health 2004; 21: 149–154.
Department of Health. Improving oral health and dental outcomes: Developing the dental public health workforce in England. London: Department of Health, 2010. http://www.dh.gov.uk/en/Publicationsandstatistics/Lettersandcirculars/Dearcolleagueletters/DH_114489 (accessed 23 June 2010)
Noble M, McLennan D, Wilkinson K et al. The English indices of deprivation 2007. Wetherby, Yorkshire, UK: Communities and Local Government Publications, 2008.
NHS County Durham and Darlington. Refreshed five year strategic plan, 2009/10 to 2013/14. pp 14. Durham: NHS County Durham and Darlington, 2010.
Department of Communities and Local Government. Indices of deprivation 2007. http://www.communities.gov.uk/communities/neighbourhoodrenewal/deprivation/deprivation07/ (accessed 1 August 2010).
Office for National Statistics. 2001 census: key statistics. Cars or vans (KS17). http://neighbourhood.statistics.gov.uk/dissemination/Download1.do (accessed 3 August 2010).
Bradshaw J, Bloor k, Huby M et al. Local Index of child well being 2009. London: Communities and Local Government Publications, 2009.
Department of Health. Dental contract management handbook. London: Department of Health, 2010. http://www.pcc.nhs.uk/contract-management-handbook (accessed June 23 2010)
Acknowledgements
We are grateful to staff at the Business Services Agency in Eastbourne for providing the primary data set; to Mr A Hall for his help in analysis of the data; to Mrs L Bennet and Mrs B Bramwell for their help in preparation of the script for the paper; and to NHS County Durham.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Landes, D., Jardine, C. Targeting dental resources to reduce inequalities in oral health in the North East of England – a health equity audit methodology to evaluate the effects of practice location, practice population and deprivation. Br Dent J 209, E3 (2010). https://doi.org/10.1038/sj.bdj.2010.676
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2010.676
This article is cited by
-
Facilitators for increasing dental attendance of people from vulnerable groups: a rapid review of evidence relevant to the UK
British Dental Journal (2023)
-
Unlocking the potential of NHS primary care dental datasets
British Dental Journal (2022)
-
Public transport access to NHS dental care in Great Britain
British Dental Journal (2021)
-
General dental practice and improved oral health: is there a win-win for both the professional establishment and government?
British Dental Journal (2020)
-
Are NHS dental practices socioeconomically distributed in Scotland, Wales and Northern Ireland?
British Dental Journal (2020)