Key Points
-
Understand the concepts of minimally invasive dentistry.
-
Understand the materials, equipment and clinical techniques available for MI direct restorative procedures.
-
Enhance patient care by optimising all clinical stages of MI direct restorations.
Abstract
The primary objectives of minimum intervention dentistry (MID) are to prevent or arrest active disease using non-operative management techniques. However, patients commonly present with cavitated caries lesions or failed restorations that are in need of operative intervention. Although much of clinical practice is devoted to preventing and managing the effects of caries and subsequent failure of the tooth-restoration complex, the clinical survival of restorations is often poor and becomes significantly worse as they increase in size and complexity. Minimally invasive (MI) restorative techniques present a range of well-documented advantages over more tissue-destructive traditional restorations by minimising unnecessary tooth tissue loss, insult to the dentine-pulp complex and reducing the risk of iatrogenic damage to adjacent hard and soft tissues. They also maximise the strength of the residual tooth structure by use of optimal adhesive restorative materials designed to restore function and aesthetics with durable, long-lasting restorations that are easy for the patient to maintain. In contemporary oral healthcare practice, if patients are to give valid consent for operative interventions, minimally invasive options must be offered, and may be expected to be the first choice of fully informed patients. This paper describes concepts of MID and provides an update of the latest materials, equipment and clinical techniques that are available for the minimally invasive restoration of anterior and posterior teeth with direct restorations.
Similar content being viewed by others
Introduction
The concept of minimum intervention dentistry (MID) embraces all aspects of clinical practice and its primary focus is the prevention and control of oral disease.1,2 In clinical situations where prevention has failed and treatment of uncontrollable disease is indicated, procedures should be chosen which respect the patient's natural tissues.3 This is referred to as minimally invasive dentistry. It may be applied to the management of all oral diseases including the minimally invasive (MI) management of caries and has been termed 'ultraconservative dentistry', 'microdentistry' as well as the protocol-specific atraumatic restorative treatment (ART).3,4,5,6
Dental restorations are only indicated when lesions have advanced to obvious cavitation and where remineralisation techniques have reached their limits.1 Contemporary management of these lesions should use the least invasive solutions and preserve the maximum amount of sound tissue.1 All clinical stages of restorative procedures should be optimised, with prevention of disease recurrence as the ultimate goal.3 In addition to the minimally invasive management of primary caries, MI principles are equally applicable to the management of the restored dentition and should conform to the following well-established objectives:7
-
Restore significant loss of dental tissue
-
Eliminate plaque retention/stagnation
-
Restore physiological masticatory function
-
Minimise the risk of recurrent disease
-
Restore aesthetics where appropriate.
MI procedures have evolved significantly over the last three decades, particularly with innovative developments in adhesive dentistry and the use of resin composite restorative materials.8,9 This continual ongoing progress has promoted a more biologically-focused approach to patient care delivery and resulted in significant advances in the fundamental principles of contemporary restorative dentistry1,3,9 (Box 1).
Challenges in restorative dentistry
There is no such thing as permanent restoration of teeth.3 Unequivocal evidence exists to show that dental restorations fail clinically and that the most commonly reported modes of failure are caries associated with restorations and sealants (CARS – formerly termed secondary/recurrent caries) and tooth-restoration complex fracture.3,11,12,13,14 At least half of the average general dental practitioner's clinical time is spent replacing and repairing existing restorations that have been placed using traditional systematic management protocols.15 It has been demonstrated that a significant number of these replacement interventions are unnecessary, as the diagnosis of tooth-restoration complex (TRC) failure is clinically subjective.11 Many failing TRCs are amenable to minimally invasive renovation techniques that will increase their functional longevity with little biological cost in the long term.10,16
When restorations are removed there is a concomitant increase in cavity size created by the operator17 resulting in further weakening of residual tooth tissue.18 The majority of cavity preparations involving proximal surfaces result in collateral iatrogenic damage, with 60–70% of adjacent surfaces developing caries more frequently than undamaged surfaces.19
Under the auspices of traditional caries management rationales, the placement of restorations has long been regarded by many, erroneously, as the primary solution to manage the caries process.1 It is clear that operative therapy is a futile method of treating disease as this has little/no effect on aetiological factors and treats only the cavities which are symptoms/signs of caries.3
The self-propelling negative spiral of repeated TRC failure and replacement, without managing the disease, has been described as the 'tooth countdown' or 'death spiral' and may ultimately result in tooth loss. Furthermore the prescription of indirect restorations is associated with a significant deterioration of this irreversible cycle due to a range of well-recognised disadvantages:20
-
Indirect restorations invariably sacrifice most or all of the residual enamel, which is the most resilient tissue and the best bonding substrate
-
Most stages of indirect restorative procedures may pose a significant threat to pulp death
-
As well as a high level of iatrogenic damage to adjacent teeth, indirect preparations carry a significant risk of damage to adjacent periodontal tissues, which may lead to persistent inflammatory conditions
-
Failure of indirect restorations can be difficult to detect and may result in complications including tooth loss
-
Aesthetic integration with residual dentition is challenging
-
In addition to high biological cost, indirect restorations are financially expensive and carry an increased risk of dento-legal complications.
In all cases of operative intervention (direct, indirect, endodontic etc), restorations should only be considered once the cause of the initial problem is detected, diagnosed and then managed.1,3 Placement of restorations without first addressing and managing the causes of lesion formation, in modern day restorative dentistry, could and should be considered as malpractice. The prescription of restorations that may be viewed as clinically unnecessary and/or cannot be maintained by the patient in the long term may also result in dento-legal claims of negligence.
MI direct restorative techniques
MI direct restorative techniques focus on biologically respectful interventions designed to address aetiological factors, maximise preservation of natural tooth tissue and promote smaller restorations of increased longevity,9 that are easier to maintain and renovate and leave future restorative options open as required.
With a growing evidence base, they demonstrate encouraging improved longevity statistics and are a proven, cost-effective, replacement to traditional restorative techniques, which in many cases should now be considered as historical.
Improvements in operative technology, dental biomaterials and the introduction of innovative techniques have made contemporary minimally invasive dentistry outcomes more predictable for almost all clinical situations from the smallest interventions right through to the management of patients with severely worn dentitions.21
Clinical stages
Detection and diagnosis
The clinical detection and diagnosis of caries lesions is challenging, especially in the presence of existing restorations.22,23 It is widely considered that a significant number of unnecessary restorative procedures are carried out every year on teeth that would have been amenable to non-operative management or renovation using minimally invasive techniques.10
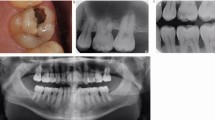
Early detection and accurate diagnosis based on individualised risk assessment are fundamental principles of MI dentistry. The use of specialised assessment and classification systems, magnification coupled with illumination, consented clinical photography and appropriate investigations have all been shown to improve the quality of clinical decision making, and will help to inform patients to give valid consent when operative intervention is deemed necessary16 (Fig. 1).
Pre-operative investigations
A detailed risk assessment and periodontal, occlusal, endodontic and aesthetic analysis should all be carried out before care planning. In addition patients' expectations for treatment and their adherence to preventive advice given by the oral healthcare team must also be ascertained in advance.
Cavity preparation
Traditional approaches to cavity design were denounced decades ago and many dentists have been practising minimally invasive tooth preparation for over 30 years.7,9 Globally, however, MI concepts are far from ubiquitous3 and many dentists continue to favour cavity designs based on outmoded, restorative material-based, surgical principles that result in over-preparation and other disadvantages that include:
-
Unnecessary removal of healthy tissue will weaken teeth, increasing the likelihood of crack propagation and fracture3,18
-
The depth, intensity, duration and extent of cavity preparation all have considerable implications for the degree of injury to pulp cells and their survival potential24
-
Although shallow dentine cavity preparation frequently damages odontoblast processes they appear to have the capacity for self-repair;24 the repercussions of deeper cavity preparation may include irreparable cell damage and the death of odontoblasts and other pulpal cells underlying the lesion24
-
Excessively long and/or inaccessible cavity margins increase the risk of microleakage, CARS and also increase the technical challenge of restorative procedures themselves
-
The difference in intrinsic moisture between superficial and deep dentine may result in reduced adhesion.8
It is well-established that complete caries excavation is unnecessary25 as selective caries removal before placing a sealed overlying restoration will arrest the process.26 Complete caries excavation in deep lesions seems careless to the point of being unethical.27 The rationale behind minimally invasive cavity preparation16,25,26 may be summarised as follows:
-
Access to carious tissue is limited to that which allows visualisation and excavation of soft, irreversibly demineralised tooth tissue
-
Existing restorations should be carefully removed to minimise the risk of cavity enlargement
-
Soft, irreversibly demineralised carious dentine should be carefully excavated using appropriate instrumentation
-
The excavation endpoint is determined by lesion texture (not colour) and stopped immediately when leathery/firm affected dentine is reached16,25,26
-
Pulp exposure should be avoided when excavating deep lesions in vital teeth
-
Overlying, unsupported enamel that is weak and liable to fracture should be removed
-
A sound cavity margin should be achieved to optimise bonding (ideally with enamel present where anatomically possible)
-
No extension into sound fissures is indicated
-
Bevels may be used to increase retention or disguise margins anteriorly,28 but are not recommended on posterior occlusal surfaces, as they may result in thin restorative margins that are liable to fracture
-
The use of magnification (+/− light) will facilitate MI preparation and caries removal3
-
Care must be taken to avoid all contact with adjacent teeth which should be inspected for early cavitated lesions, which may be restored conservatively while there is direct access during the procedure
-
Current commercially available caries detector dyes are contraindicated26 as they lead to significant over-preparation as a result of diffusion and porosity effects within the dentine.25
Although specialised equipment and materials are available to assist MI cavity preparation,29 the careful use of conventional instruments should yield acceptable results that may be expected to improve with experience.26 As the use of rotary instruments has been demonstrated to have an important influence on pulp response, the following guidelines should be observed:24
-
High speed burs must be cooled with copious water spray at all times
-
When excavating caries with round steel or tungsten carbide burs, they should be used at slow speed, with light pressure (Fig. 2a)
-
Hand instruments should be used when excavating caries-infected dentine close to the pulp to maximise selective control through tactile feedback (Fig. 2b)
Air-abrasion
A range of innovative technology is now available to assist MI cavity preparation29 and includes: plastic burs, chemomechanical agents, sono-abrasion, laser systems and fluoresce-aided caries excavation (FACE). Air-abrasion (Fig. 3) pre-dates the air turbine30 and has seen a recent resurgence by practitioners who have welcomed its advantages, which include:
-
A variety of abrasive powders are available to allow the quick, easy, predictable creation of ultra-conservative cavity preparations with potential tissue selectivity31
-
Preparation with air-abrasion produces rounded cavity line angles that will generate less stress at bonded interfaces during polymerisation shrinkage
-
Studies have demonstrated that air-abrasion with bioactive glass particles is capable of creating a therapeutic bioactive smear layer that encourages remineralisation, preserves the integrity of dentine-bonded interfaces and enhances the bond strength to certain adhesive materials.8
Iatrogenic damage
A spectre hanging over operative dental procedures is the high prevalence of iatrogenic damage to adjacent hard and soft tissues, particularly when operative interventions involve proximal surfaces.19 A recent study demonstrated that experienced dentists, when using high-speed rotary instruments, damage 75% of adjacent surfaces with a range of severity, rising to 95% for inexperienced dentists with extensive damage recorded in over 20% of cases.32 Reducing this risk is one of the cornerstones of MID and may be optimised in a number of ways, most notably with careful technique, magnification/good lighting and specialised equipment such as the use of protective proximal wedges seen in Figure 4.
Direct restorative material options
It is advisable to delay the final decision on choice of restorative material until cavity preparation is complete. The final histology of the prepared cavity surface coupled with knowledge of the chemistry behind the adhesive materials available and their handling characteristics will allow the practitioner to select the most appropriate material.
While research continues into innovative biomaterials designed to minimise tooth preparation, reinforce remaining tooth structure, stimulate pulp healing and encourage remineralisation (bioactivity), dental amalgam for now remains the world's most commonly used direct restorative material, followed by resin-based composite materials and glass ionomer cement and its derivatives.
Historically dental amalgam exhibits the greatest material longevity in many reported studies33,34 but resin composite now demonstrates the capability of providing decades of success and when inevitable failure occurs, it remains amenable to minimally invasive refurbishment, re-sealing, repair or replacement10 (Fig. 5).
Although amalgam has served dentistry for over 150 years, its use is declining primarily due to patient and professional demand for tooth-coloured alternatives that are generally less sacrificial of tooth tissue. This is coupled with the environmental, health and economic concerns as well as political changes sweeping across nations with the signing of the UNEP Minamata Treaty to phase down and ultimately ban the use of mercury-containing products globally.35
Although amalgams may be employed as a more minimally invasive alternative to indirect restorations in the badly broken down posterior dentition, they generally require more destructive tooth preparations to optimise retention and resistance form and additionally provide an inferior cavity seal compared to adhesive restorations.
Glass ionomer and resin-modified glass-ionomer cements
Glass ionomer cements (GIC) and their derivatives possess the ability to create dynamic chemical bonds to enamel and dentine. While they are reported to possess anti-microbial properties that may increase resistance to demineralisation, in part by their potential to release fluoride ions, the clinical relevance of this feature remains the subject of debate.36
Resin-modified glass ionomer cements (RMGIC) have been described as being resistant to the challenging conditions of the oral environment.8 They have thermal expansion coefficients that closely match those of dentine8 but suffer hygroscopic expansion due to water absorption which can affect their long term colour stability in vivo.
Despite recent developments in reinforced GIC materials the currently available published evidence suggests that further improvements in the mechanical properties of GICs are required before they can be recommended for the routine restoration of teeth with extensive class I and II lesions.37 They also have aesthetic disadvantages compared to resin composite materials. Current recommendations limit their use to non-load bearing restorations for example, class V cavities, ART restorations in deciduous teeth, provisional restorations, as part of an open or closed 'sandwich'/laminate restorative protocol under more durable materials, or as indirect pulp protection materials designed to enhance bond durability in deeper cavities.8
Resin composite materials
Resin composite (RC) materials are the mainstay of MI direct restorative techniques and are suitable for many clinical situations.38 For the last 30 years RC restorations have continued to gain popularity among clinicians worldwide8,38 as they offer a range of significant advantages, including:
-
Promotion of minimally invasive cavity preparation limited to that required to visualise and excavate irreversibly damaged tooth tissue
-
Adhesive techniques/tissue penetration may increase fracture resistance9,18
-
Efficacy for the conservative restoration of aesthetically important teeth, significantly reducing or even eliminating the need for indirect restorations and satisfying patient demand for tooth-coloured restorations38
-
May be effective for the immediate treatment of painful, cracked teeth39
-
Adaptation to cavity form for example, the root surfaces of elderly patients who are retaining their natural teeth and require restorative treatment into old age
-
Sealed restorations promote pulp cell survival and repair, by reducing the risk of bacterial microleakage.24
Preventive resin restorations (therapeutic fissure sealants) may be considered to be the material of choice for the ultra-conservative restoration of early, discrete lesions in the fissures of posterior teeth in high risk patients where non-operative prevention/remineralisation regimes have failed repeatedly. These have been demonstrated to produce excellent long-term results.23
Posterior RCs are also the logical choice for the treatment of more extensive lesions, where minimally invasive techniques can still be applied.38 Since RC may be adapted to any shape or size of cavity the undermined enamel that remains after selective removal of dentine caries can be retained, where it will be supported by the bonded composite.10 The resultant, smaller surface area restoration will be easier to shape and will be subject to reduced occlusal loading.9 When RC is used in the treatment of primary occlusal lesions, such restorations have been shown to occupy 80% less tooth surface area than an equivalent traditional amalgam restoration.40
Encouraging long term outcomes are now allowing clinicians to favour RCs, even when restoring complex, multi-surface cavities (Fig. 6), endodontically treated teeth and severely worn dentitions.21 In addition the majority of clinicians now use direct composite routinely to restore damaged anterior teeth and some consider these materials to have obviated the need for more destructive indirect restorations.
Moisture control
Rubber dam is the optimal method of moisture control41 and although it is possible to get good results using other methods,21 blood, saliva and crevicular fluid will all affect adhesion adversely and increase the subsequent risk of microleakage. Careful use of rubber dam will guarantee isolation and improve visibility, making procedures easier and more predictable.
Matrix systems
Reproduction of tight, anatomically-correct proximal contacts on posterior and anterior restorations is essential and a good matrix technique has been shown to be the most important determinant of success.42 Traditional 'matrix and holder' circumferential matrix systems, designed over 50 years ago for use with amalgam, have limited use in contemporary MI restorative dentistry.43 A wide range of specialised matrix and wedge systems are now available for both anterior and posterior restorations that help to:38
-
Provide restorations that minimise the risk of food impaction and subsequent periodontitis and CARS2
-
Recreate embrasure anatomy that facilitates plaque biofilm removal from interproximal areas
-
Reduce the risk of adhesive failures which have commonly been tracked to the gingival margin of class II restorations21
-
Promote tight contacts via thin, adaptable, burnishable matrices
-
Reduce the risk of cervical extrusion of composite which, once cured, is virtually impossible to remove completely without damage to adjacent tissues
-
Provide tooth separation to compensate for matrix thickness.
A specialised matrix system like the one demonstrated in Figure 7 has been shown to give the best proximal contact areas when placing posterior composite restorations44 and comprises:
-
A thin sectional matrix
-
A plastic wedge which has a concave gingival contour to fit over and compress the interdental papilla
-
A separation ring which along with the wedge helps to separate the teeth to account for the matrix thickness and seal laterally to reduce the risk of excess.
Adhesion
Bonding between the cavity and the restorative material is one of the most important stages in MI direct restorative procedures. Optimising adhesion is essential for the following reasons:
-
Obviates the need for traditional and often outdated 'lining/base' materials
-
The cavity seal is very important to pulp health as bacterial microleakage will perpetuate and exacerbate pulpal inflammation24
-
Sealing the cavity will arrest lesion progression by isolating residual bacteria from their fermentable carbohydrate nutrient source and allow time for the defence reactions of tubular mineralisation and tertiary dentine formation25,26
-
The failure of moderate to large adhesive restorations has been linked to degradation of the bond at the tooth-surface composite interface.2 The last two decades have seen dramatic improvements in dental adhesives and research continues on innovative bioactive bonding systems that may promote remineralisation and enhance the longevity of resin-dentine bonds8
-
Optimal adhesion is required to resist the shrinkage forces generated when resin-based materials are polymerised.8
Since successful bonding is a fundamental requirement for long-lasting composites, fastidious attention to the manufacturer's protocols is essential for each adhesive system.45 As errors in application may have adverse clinical consequences, the following widely accepted guidelines should be followed:16,45
-
Follow manufacturer's instructions with regard to etching, washing and drying, application of adhesive and light curing
-
Etch and rinse systems with separate primer and adhesives are considered to be the optimal method of bonding in dentistry at present
-
Simplified fewer-step adhesive protocols are designed to reduce technique sensitivity but can exhibit lower bond strengths and poorer durability,8 partially as a result excessive water absorption leading to hydrolytic degradation of the resin matrix8
-
The aim of 'moist bonding' with etch and rinse adhesives is to allow the dentine collagen to remain fully hydrated throughout the bonding protocol.8 Before adhesive application the cavity should appear slightly but visibly moist, with no obvious pooling38
-
Following adhesive application all cavity surfaces should appear glossy/shiny before light-curing as per manufacturer's instructions38
Placement and shaping
Placement technique is one of the most important variables determining the long-term success of adhesively bonded restorations.38 Operator skill and experience are important factors governing the quality of marginal adaptation, the elimination of non-homogeneous layers and formation of an anatomically correct final layer.21
When placing posterior composites, the use of small 2 mm increments has been recommended for many years to give a more effective and uniform volumetric polymerisation and reduce total polymerisation shrinkage.38 Incremental placement technique also helps control the shape of restorations. When placing anterior composites the latter is a more important benefit than the management of polymerisation shrinkage stress, due to the favourable configuration (C) factor of most anterior cavities.28
Recently introduced 'bulk-fill' materials have reduced technique sensitivity in posterior restorations by partially or completely eliminating the need for traditional incremental placement technique. Development of low-shrink composites is an area of ongoing research with an increasing number of published studies.46 The original 'bulk-fill base' materials for example, SDR (Dentsply Sirona, York, USA) (Fig. 8a) or 'full contour bulk-fill' materials for example, SonicFill (Kerr, California, USA) are proving popular with clinicians as they may offer a number of significant advantages:
-
Flowable consistency gives improved marginal adaptation and reduced porosity inclusion at the base of deep cavities
-
Innovative monomer chemistry promotes lower polymerisation shrinkage stress concentration at the tooth interfaces47,48
-
Use of large or even single increments offers significant time savings compared to traditional incremental placement techniques
-
Bulk-fill materials are more light sensitive, giving enhanced cure depths, for example 4-5 mm depending on material and its shade
-
Injection technology obviates the need for instrumentation and reduces the risk of voids between layers or at margins.
Whether using bulk-fill or traditional materials, it is recommended to shape the final increment as anatomically as possible. Composite materials should be chosen that are non-sticky, easy to shape and do not slump before light polymerisation. Specialised placement and shaping instruments (Fig. 8b) may be used to minimise finishing and marginal excess which, once set, can be difficult to visualise and remove with control.
Light curing
Various light curing regimes have been proposed but the clinical significance of these protocols is the subject of debate and may have a limited effect on polymerisation shrinkage and therefore stress formation.
When light curing, the following generally accepted guidelines should be followed:49
-
Use high quality lights with optimal irradiance and uniform beam profiles that preclude any 'cold spots' on the light guide tip
-
The light tip should be placed as close and as perpendicular to the restoration surface as possible
-
LED units are recommended by many and may offer up to 10,000 hours of service
-
While RC cannot realistically be 'over-cured' (25–40% remains as unreacted monomer), care must be taken not to overheat the pulp
-
Lighter shades will cure more readily than darker shades, which absorb more light
-
Light units should be meter-tested regularly as low intensity light still appears bright
-
Care must be taken to prevent premature polymerisation by the overhead chair light
-
As most light guides will be destroyed by sterilisation processes, transparent barrier materials should be employed to prevent cross infection.
Finishing and polishing
Despite best efforts, slight functional and/or aesthetic adjustments are usually necessary and an array of specialised diamond and tungsten carbide burs are available to facilitate this. They should be applied intermittently with light pressure and water spray to prevent overheating and potential pulp irritation. A variety of polishing discs are also available and may be used to impart smooth surfaces. They are especially useful for transition lines and marginal ridges (Fig. 9), where they are less likely to damage adjacent teeth and will impart a high shine in the completed restoration.
Heavy, immediate finishing will also increase the potential for formation of 'white-line' fractures around the restoration. It is believed that these are related to enamel fractures occurring 10–50 μm from the restoration margin.28
As with all clinical stages the use of magnification will facilitate finishing procedures by reducing the risk of iatrogenic damage when removing marginal excess.
Maintenance
As well as designing restorations that restore function and where appropriate aesthetics, care should be taken to shape restorations so that they are easily maintained by the patient. Oral hygiene instructions given at the planning stage should be reinforced and the quality of homecare regimes carefully monitored at review consultations. Finished MI direct restorations (Fig. 10) should be regularly assessed using objective criteria, ideally as part of a systematic protocol50 (Table 1).
The materials, equipment and techniques that have been employed should be precisely documented to enable a long-term clinical audit of minimally invasive restorative procedures.
Summary
Minimally invasive direct restorations are an integral component of contemporary oral healthcare practice and present a number of significant advantages compared to more destructive traditional treatments, especially indirect restorative alternatives.
An array of materials, equipment and clinical techniques are available to simplify and optimise MI direct restorative procedures. These are designed to maximise conservation of biological tissues, ensure the lifelong health of the teeth that they restore and leave future options open for MI renovation when failure occurs.
The time taken to equip practices, master and refine minimally invasive direct restorative techniques will be rewarding for patients and clinicians alike.
References
Featherstone J D B, Doméjean S . Minimal intervention dentistry: part 1. From 'compulsive' restorative dentistry to rational therapeutic strategies. Br Dent J 2012; 213: 441–445.
Banerjee A . Minimal intervention dentistry: part 7. Minimally invasive operative caries management: rationale and techniques. Br Dent J 2013; 214: 107–111.
Ericson D . The concept of minimally invasive dentistry. Dent Update 2007; 34: 9–10.
Schwendicke F, Frencken J E, Bjørndal L et al. Managing carious lesions: consensus recommendations on carious tissue removal. Adv Dent Res 2016; 28: 58–67.
Smales R J, Yip H K . The atraumatic restorative treatment (ART) approach for primary teeth: review of literature. Paediatr Dent 2000; 22: 294–298.
Holmgren C J, Roux D, Doméjean S . Minimal intervention dentistry: part 5. Atraumatic restorative treatment (ART) – a minimum intervention and minimally invasive approach for the management of dental caries. Br Dent J 2013; 214: 11–18.
Elderton R J, Jenkins C B, Marshall K J et al. Changing perceptions of the requirements of cavity preparations. Br Dent J 1990; 168: 30–32.
Salvatore S, Pashley D H . Strategies to stabilise dentine-bonded interfaces through remineralising operative approaches – State of the art. Int J Adhesion Adhesives 2016; 69: 39–57.
Shortall A C, Wilson H J . New materials, bonding treatments and changes in restorative practice. Br Dent J 1988; 164: 396–400.
Green D, Mackenzie L, Banerjee A . Minimally invasive long-term management of direct restorations: the '5 Rs'. Dent Update 2015; 42: 413–426.
Mjör I A, Toffenetti F . Secondary caries: a literature review with case reports. Quintessence Int. 2000 Mar; 31: 165–79.
Hickel R, Manhart J . Longevity of restorations in posterior teeth and reasons for failure. J Adhes Dent 2001; 3: 45–64.
Manhart J, Chen H, Hamm G, Hickel R . Buonocore Memorial Lecture. Review of the clinical survival of direct and indirect restorations in posterior teeth of the permanent dentition. Man Oper Dent 2004; 29: 481–508.
Lucarotti P S, Holder R L, Burke F J . Outcome of direct restorations placed within the general dental services in England and Wales (Part 1): variation by type of restoration and re-intervention. J Dent 2005; 33: 805–815.
McAndrew R, Chadwick B, Treasure E T . The influence of a short training programme on the clinical examination of dental restorations. Oper Dent 2011; 36: 143–152.
Banerjee A, Watson T F . Pickard's guide to minimally invasive operative dentistry. 10th ed. OUP Oxford, 2015.
Dörter C, Yildiz E, Erdemir U . Effect of operators' skills on increase in cavity volume of restorations. Quintessence Int 2003; 34: 27–30.
Burke F J T . From extension for prevention to prevention of extension: (minimal intervention dentistry). Dent Update 2003; 30: 492–498, 500, 502.
Qvist V, Johannessen L, Bruun M . Progression of approximal caries in relation to iatrogenic preparation damage. J Dent Res 1992; 71: 1370–1373.
Maglad A S, Wassell R W, Barclay S C, Walls A W . Risk management in clinical practice. Part 3. Crowns and bridges. Br Dent J 2010; 209: 115–122.
Opdam N J M, Skupien J A, Kreulen C M et al. Case report: a predictable technique to establish occlusal contact in extensive direct composite resin restorations: the DSO-Technique. Oper Dent 2016; 41: 96–108.
Kidd E A . Diagnosis of secondary caries. J Dent Educ 2001; 65: 997–1000.
Mackenzie L M, Banerjee A . The minimally invasive management of early occlusal caries: A practical guide. Prim Dent J 2014; 3: 42–49.
Smith A J, Murray P E, Lumley P J . Preserving the vital pulp in operative dentistry: I. A biological approach. Dent Update 2002; 29: 64–69.
Banerjee A, Watson T F, Kidd E A M . Dentine caries: take it or leave it? Dent Update 2000; 27: 272–276.
Kidd E A M . How 'clean' must a cavity be before restoration? Caries Res 2004; 38: 305–313.
Kidd E, Fejerskov O, Nyvad B . Infected dentine revisited. Dent Update 2015; 42: 802–806, 808–809.
Mackenzie L M, Parmar D, Shortall A C, Burke F J . Direct anterior composites: a practical guide. Dent Update 2013; 40: 297–308.
Banerjee A, Watson T F, Kidd E A . Dentine caries excavation: a review of current clinical techniques. Br Dent J 2000; 188: 476–482.
Banerjee A, Watson T F . Air abrasion: its uses and abuses. Dent Update 2002; 29: 340–346.
Banerjee A, Thompson I D, Watson T F . Minimally invasive caries removal using bio-active glass air-abrasion. J Dent 2011; 39: 2–7.
Milic T, George R, Walsh L J . Evaluation and prevention of enamel surface damage during dental restorative procedures. Aust Dent J 2015; 60: 301–308.
Osborne J W . Amalgam: dead or alive? Dent Update 2006; 33: 94–98.
Ferracane J L . Resin composite - state of the art. Dent Mater 2011; 27: 29–38.
Bailey M (ed) . Minimata Convention on Mercury. United States Environmental Protection Agency, 2013.
Burke F J . Dental materials - what goes where? The current status of glass ionomer as a material for loadbearing restorations in posterior teeth. Dent Update 2013; 40: 840–844.
Cury J A, de Oliveira B H, dos Santos A P, Tenuta L M . Are fluoride releasing dental materials clinically effective on caries control? Dent Mater 2016; 32: 323–333.
Mackenzie L M, Shortall A C C, Burke F J T B . Direct posterior composites: a practical guide. Dent Update 2009; 36: 71–80.
Opdam N J, Roeters J J, Loomans B A, Bronkhorst E M . Seven year clinical evaluation of painful cracked teeth restored with a direct composite restoration. J Endod 2008; 34: 808–811.
Roeters J J, Shortall A C, Opdam N J . Can a single composite resin serve all purposes? Br Dent J 2005; 199: 73–79.
van Dijken J W, Hörstedt P . Effect of the use of rubber dam versus cotton rolls on marginal adaptation of composite resin fillings to acid-etched enamel. Acta Odontol Scand 1987; 45: 303–308.
Peumans M, Van Meerbeek B, Asscherickx K, Simon S, Abe Y, Lambrechts P, Vanherle G . Do condensable composites help to achieve better proximal contacts? Dent Mater 2001; 17: 533–541.
Strydom C . Handling protocol of posterior composites - part 3: matrix systems. SADJ 2006; 61: 18–21.
Loomans B A, Opdam N J, Roeters et al. A randomized clinical trial on proximal contacts of posterior composites. J Dent 2006; 34: 292–297.
Green D J, Banerjee A . Contemporary adhesive bonding: bridging the gap between research and clinical practice. Dent Update 2011; 38: 439–450.
Mackenzie L M, Burke F J T B, Shortall A C C . Posterior composites: a practical guide revisited. Dent Update 2012; 39: 211–212, 215–216.
Ilie N, Hickel R . Investigations on a methacrylate-based flowable composite based on the SDR™ technology. Dent Mater 2011; 27: 348–355.
Moorthy A, Hogg C H, Dowling A H, Grufferty B F, Benetti A R, Fleming G J . Cuspal deflection and microleakage in premolar teeth restored with bulk-fill flowable resin-based composite base materials. J Dent 2012; 40: 500–505.
Shortall A C, Price R B, Mackenzie L, Burke F J . Guidelines for the selection, use, and maintenance of LED light-curing units – Part 1. Br Dent J 2016; 221: 453–460.
Ryge G, Snyder M . Evaluating the clinical quality of restorations. J Am Dent Assoc 1973; 87: 369–377.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Mackenzie, L., Banerjee, A. Minimally invasive direct restorations: a practical guide. Br Dent J 223, 163–171 (2017). https://doi.org/10.1038/sj.bdj.2017.661
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2017.661
This article is cited by
-
Minimally invasive selective caries removal: a clinical guide
British Dental Journal (2023)
-
Top tips for minimally invasive dentistry in primary care
British Dental Journal (2023)
-
A scoping literature review on minimum intervention dentistry for children with dental caries
British Dental Journal (2022)
-
The effects of photodynamic therapy with blue light and papain-based gel associated with Urucum, on collagen and fibroblasts: a spectroscopic and cytotoxicity analysis
Lasers in Medical Science (2020)