Key Points
-
Describes the approach taken by North Wales to reshape the NHS orthodontic provision.
-
Provides information on the protocols and practices which were established to allow a fair and transparent process to be followed.
-
Highlights the need for a fully functioning Orthodontic Managed Clinical Network with engagement from the clinical, managerial and commissioning teams to enable a coherent strategy to be formed and implemented.
Abstract
The orthodontic service provision within North Wales, in common with many areas of the United Kingdom, was experiencing increasing waiting times for assessment and treatment. Reasons for this included an increasing population, patient demand and fixed NHS contracted orthodontic provision. In addition to these universal challenges, the geography of North Wales contributed to difficulties in accessing care. It was felt that with a reshaping of the orthodontic services there was potential to enhance the quality of orthodontic care available to patients and deliver prudent NHS orthodontic services. Three distinct, but inter-related steps, were identified to progress the reshaping of the service with the intended outcome of achieving an improved co-ordinated service. Initially, this involved the re-commissioning of the primary care specialist service through a formal retendering process. Following this, a standardised orthodontic referral form was developed, to be used for all orthodontic referrals regardless of whether their destination was a primary or secondary care provider. Finally, a formal accreditation process for all non-specialist dentists who were undertaking NHS orthodontic treatment was developed and implemented. The successful outcome of this process was only possible because of the close working partnership between the North Wales Orthodontic Managed Clinical Network (OMCN) and Betsi Cadwaladr University Health Board.
Similar content being viewed by others
Introduction
As with many areas across the United Kingdom, the orthodontic service provision in North Wales was stretched with waiting lists for assessment and treatment increasing. Reasons included an increasing population, increasing patient demand for care and a fixed NHS contracted orthodontic provision. In addition to these universal challenges, the geography of North Wales contributed to difficulties in accessing care.
There was a view that with some reshaping of orthodontic services there was potential to enhance the quality of orthodontic care available to patients and deliver prudent1 NHS orthodontic services. It was considered that reliance on secondary care providers for orthodontic assessments and treatments could be reduced for those cases that could safely be delivered in primary care. Three distinct but inter-related steps were identified to progress the reshaping of the service with the intended outcome of achieving an improved co-ordinated service.
The first step was the re-commissioning of the primary care specialist service through a formal retendering process. Following this a standardised orthodontic referral form was developed, to be used for all orthodontic referrals regardless of whether their destination was a primary or secondary care provider. Finally, a formal accreditation process for all non-specialist dentists who were undertaking NHS orthodontic treatment was developed and implemented. The successful outcome of this process was only possible because of the close working partnership between the North Wales Orthodontic Managed Clinical Network (OMCN) and Betsi Cadwaladr University Health Board.
This paper outlines the processes involved and demonstrates the improvements in the provision of orthodontic care across the region.
The Forum
Orthodontic Managed Clinical Network and Strategic Advisory Forum
The Welsh Government (WG) has been proactively looking at orthodontic provision within Wales for a number of years. In order to improve the coordination of services, WG requested that each area of Wales (North Wales, including Powys; South East Wales; South West Wales) established a functioning OMCN. These OMCNs not only provide an advisory role to their Local Health Boards (LHBs) but also make representation to the WG Strategic Advisory Forum in Orthodontics (SAFO) which was established in 2011.
Under this directive an OMCN was established in North Wales covering Betsi Cadwaladr University Health Board (BCUHB) & Powys Teaching Health Board. This OMCN had representation from all stakeholders which enabled it to effectively address strategic orthodontic issues affecting the region. The membership included representation from the Health Boards; primary care orthodontic sector; secondary care orthodontic sector; Community Dental Service (CDS); Dental Public Health; Local Dental Committee (LDC); Local Orthodontic Committee (LOC) and a Dental Advisor. The OMCN reports locally to the North Wales Oral Health Strategy Group (NWOHSG) and nationally to the SAFO. Figure 1 indicates the lines of reporting associated with the OMCN
The situation
Geographically, North Wales covers almost a third of the land mass of Wales and is home to approximately a quarter of its population. Access to orthodontic services is problematic because of its relatively wide spread population and rural nature.
Traditionally, the BCUHB has commissioned specialist orthodontic services in both the primary and secondary care settings. This has been supplemented by a number of dentists, both GDS and CDS, who have extensive orthodontic experience but who are not on the GDC's Orthodontic Specialist List. These non-specialist orthodontic providers undertake a valuable role in the delivery of an orthodontic service especially in the more remote geographic areas.
Specialist primary orthodontic services were concentrated in five localities across North Wales with secondary care orthodontic provision sited at the three district general hospitals.
Dental public health undertook a comprehensive Orthodontic Needs Assessment and produced a working document in August 2013 (Orthodontic Needs Assessment, Version 1, 16 August 2013, Dr J. S. Sandham)2 to inform the Primary Dental Care Orthodontic Commissioning Group (a working group from both the OMCN & NWOHSG).
In addition to epidemiological and research evidence, the report addressed deprivation; orthodontic treatment need; prevalence of orthodontic problems; current activity within BCUHB and cross border activity. The report made recommendations on the number of units of orthodontic activity (UOAs) to be commissioned and the LHB concluded that specialist primary care services should ideally be centred in the four areas of largest population density. The aim was to manage service provision within existing historical funding utilising appropriate efficiency savings and potential equalisation of UOA values across North Wales.
The report also detailed the current orthodontic provision including dentists with special interest in orthodontics, CDS, primary care specialist services and secondary care specialist services. The prevalence of malocclusion in the 12-year-old population is commonly used as a reference for quantifying orthodontic treatment need and the 2011 census indicated that North Wales had a 12-year-old population of 7,689 (Figure 2 [ONS, Census 20113]). Figure 2 shows the 12-year-old population distribution in 2011 and the orthodontic service provision in 2013.
Orthodontic services in Wales have been reviewed both regionally and nationally. In the Welsh Government's Delivery Plan Together for Wales: A National Oral Health Plan for Wales 2013-184 the findings of two national groups are summarised. Both the Independent Task and Finish Group established by Welsh Government to review orthodontic provision in Wales5 and an inquiry conducted by the Welsh Assembly Health, Wellbeing and Local Government Committee made similar recommendations.6 They highlighted the pressing requirement for Health Boards to develop more effective planning and management of these services and to ensure improvement in the efficiency and effectiveness of orthodontic services delivered in Wales.
Taking account of the reports, The National Oral Health Plan stated:4
'With effective procurement and contracting, improvement in the appropriateness of referrals and performance management, there appears to be sufficient resources to meet the orthodontic need of the population and to ensure that limited resources are not wasted.'
The intention of Welsh Government was stated as:
'To move towards the position where all primary care orthodontics is provided by specialists and/or dentists with a special interest (DwSI).' and to develop a workforce 'led by Specialist Orthodontists supported by orthodontic therapists, DwSIs, orthodontic nurses and orthodontic technicians.'4
Based on these recommendations and the Local Orthodontic Needs Assessment, BCUHB undertook a recommissioning exercise of primary care specialist orthodontic services.
Recommissioning services
The Primary Care Orthodontic Commissioning Group had delegated authority from the NWOHSG to develop and deliver the process for the re-tendering of the specialist orthodontic practice contracts. The group's aim was to establish the local requirements to meet the Health Board defined need, evaluate and select the bidders, appoint the successful bidders and assist the Health Board in entering into a contract with the chosen providers. The membership included the BCUHB Director of Oral Health; an LDC representative; a BCUHB Finance representative; a BCUHB Clinical Programme Group representative; two BCUHB Primary Care Support Unit staff; a dental public health representative and two orthodontic specialists. One of the specialists was the OMCN representative with no primary care practice interests. The other was an out of area primary care orthodontic specialist commissioned for the sole purpose of the development of relevant aspects of the service specification. This arrangement avoided any conflict of interests. The service specification was one of a number of documents developed to support the recommissioning process. It also formed part of the Memorandum of Information (MOI) which outlined the procurement process, the commercial framework and the governance and administrative requirements. The MOI provided sufficient information on the procurement process to enable potential bidders to make an informed decision on whether they wished to participate. Interested parties were required to submit a pre-qualification questionnaire (PQQ). This covered the business and clinical organisational structures with the purpose of demonstrating an ability to be able to meet the obligations entailed in delivering services. A weighted standard scoring system was utilised together with pass/fail categories to evaluate the PQQs before the Invitation to Tender (ITT) documentation was issued.
During the development of the processes and accompanying documentation, the commissioning group was supported by a member of the Health Board Project Team. The Primary Care Support Unit took forward the tendering and subsequent stages in conjunction with the commissioning group. Table 1 outlines the process.
The Health Board developed contingency plans should any current contract holders be unsuccessful in the re-tendering process. These were as follows:
-
1
A long run in period between the outcome of the bidding process and the end of existing contracts/start of new contracts to allow for any unsuccessful practices to adapt their business model and minimise any disruption for patients involved
-
2
Adequate arrangements for the continued care of patients under treatment with any unsuccessful bidder. If a new successful bidder took on the practice site and/or patient portfolio of an unsuccessful bidder, then the incoming contractor would pick up the continuing care responsibilities of the outgoing contractor. If this was not the case, then the outgoing contractor would be provided with an extension of their PDS contract on a 'continuing care only' basis allowing the completion of all outstanding treatment cases until the end of the retention period and thus minimising any disruption to the patients involved
-
3
Arrangements to transfer any patients on an 'assessment and treatment' waiting list from an unsuccessful bidder to the nearest successful bidder.
After due tendering process, four orthodontic PDS contracts were awarded (geographically based in the four main population centres of North Wales). Key components of these new contracts were:
-
1
The overall level of activity contracted by the health board with specialist orthodontic practices was increased by around 30%, with a distribution between practices matching the anticipated demand set out in the needs assessment
-
2
The competitive tender process resulted in a reduction in UOA rate effectively limiting the increase in overall contract values to 13%
-
3
Key performance indicators (KPI) were introduced into the new contracts to improve monitoring and maximise the amount of orthodontic activity being used on treatment starts rather than orthodontic review activity (minimum number of treatment starts per year calculated by 'contracted UOA ÷ 22.5' and only one review per patient in a 24 month period)
-
4
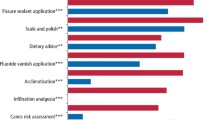
Stipulation introduced on the appropriate supervision of the non-specialist dental team members (that is, therapists and GDPs with or without DwSI accreditation)
-
5
Contract length was increased to ten years, subject to satisfactory performance at review and with an optional break clause after the first four years. Knowing the funding stream would be for an extended period, has resulted in stability to the practice system as well as encouraging orthodontic practices to invest in their infrastructure. Locally this has resulted in training of orthodontic therapists and employment of ancillary staff to facilitate this.
Standardised referral form
After establishing a stable and appropriate primary care specialist orthodontic service, efforts of the OMCN were then directed towards developing a suitable orthodontic referral form to be used for all orthodontic referrals from primary care across the BCUHB area.
Historically, North Wales consisted of six separate Local Health Boards and three Trusts. Over time these merged, eventually forming Betsi Cadwaladr UHB in 2009. As such there was a legacy of various methods of referral to specialist orthodontic providers (both in primary and secondary care) across North Wales. The vision of the Chief Dental Officer of Wales was to have an All Wales Electronic Orthodontic Referral Form. However, the introduction of universal dental e-referrals for all disciplines is likely to be dictated by the provision of a robust IT infrastructure across all service sectors in Wales. As this appeared to be some way off, an interim measure was considered necessary. It was therefore determined that each area, covered by the three MCNs, should have its own standardised orthodontic referral form prior to the adoption of an 'All Wales' orthodontic referral process.
Regional variations in the perceived information required as part of a referral generated challenges in producing an All Wales Referral Form. Both OMCNs in South Wales had only recently introduced their own stand-alone referral protocols and felt it was too early to change the process. North Wales OMCN determined to take the opportunity to produce a Universal Orthodontic Referral Proforma which would standardise all referrals from primary care to specialist orthodontic providers in North Wales and also suggested a prototype of an All Wales Orthodontic Referral Form. Referral forms from across North Wales, Merseyside and Cheshire were collected and a working group analysed them highlighting the most desirable features which would cover referrals to both primary and secondary care orthodontic services. Two referral forms were created and opinions sought from the local dental committee and local orthodontic committee. A grid based referral form was ultimately selected which guided the referrer to the most appropriate service provider.
This pilot referral form was then discussed between the three OMCNs of Wales and modified to ensure the information gathered by the referral form was potentially suitable for all regions of Wales. It was accepted that an All Wales Universal Orthodontic Referral Form will inevitably not cover all local requirements across Wales but it was considered that the referral form produced would cover the majority of cases being referred for specialist orthodontic care with the free text spaces allowing for the referring practitioner to provide additional information for the more unusual referrals. The new Universal Orthodontic Referral Form was subsequently discussed again with local stakeholders as well as at the Strategic Advisory Forum in Orthodontics where it was accepted as a precursor for an All Wales version. The new referral form (Appendix 1) has been introduced in North Wales and was disseminated to all NHS dental providers with a covering explanatory letter which detailed the IOTN system and the new referral pathways.
This referral form was introduced in September 2015 and is now in exclusive use. Any inappropriate referrals or referrals by other means are no longer accepted and returned to the referring practitioner.
Anecdotally, it is reported that it has already made it easier for specialist providers to identify cases requiring prioritisation as well as reducing inappropriate referrals. It has also assisted in reducing 'double' referrals. A particular feature of this form is that it guides the referring practitioner to both the appropriateness of the referral as well as guiding them to refer to the most suitable service provider by following the 'tick-box' format. This 'tick-box' layout with additional indication for priority referrals allows the person receiving the referral to triage the referral quickly (Appendix 1).
DwSI accreditation process
As mentioned previously, BCUHB provides the healthcare services for a population of almost 687,800 people spread out over approximately a third of the land mass of Wales (6172 square kilometres). In addition to the uneven population distribution, North Wales also demonstrates a topography which further hinders access to specialist care generally and specialist orthodontic services in particular. It is under these circumstances where the use of dentists with special interest in orthodontics working in GDS or CDS setting, provide a crucial role in the provision of orthodontic care to a geographically disadvantaged population.
One of the intentions of the National Oral Health Plan was 'to move towards the position where all primary care orthodontics is provided by specialists and/or dentists with a special interest (DwSI)'.
It had been decided at a National Wales level that all orthodontic treatment planning should be undertaken by a clinician on the orthodontic specialist list and that all non-specialist dentists providing NHS orthodontic treatment should be accredited. This would assure the Welsh Government of the competency of the workforce delivering NHS orthodontic provision. It was determined that the accreditation process should look at the capability of the DwSI to both assess the need for orthodontic intervention and to carry out a treatment plan provided by an orthodontic specialist. Tripartite discussions were held between the three OMCNs in Wales to agree the basic principles for the remit of a dentist with special interest in orthodontics. Each of the regions subsequently undertook an accreditation process that was geared towards their own local needs.
In North Wales, this formal process was based on a model developed by the South-East Wales Orthodontic Managed Clinical Network. An outline of the proposed accreditation process was discussed with all stakeholders including the BCUHB, LDC and LOC, in order to ensure that the process was robust and fair to all (Table 2).
To ensure that the accreditation process was fair and open to all, the invitation to apply was distributed to all providers of NHS dental care within BCUHB. Applicants were required to present a portfolio listing their most recent ten consecutively completed cases including before and after peer assessment rating (PAR) scores and percentage improvement as well as start and finish study models (with accompanying photographs if available).
The logbooks were assessed by an external consultant who produced a report for the accreditation panel. Two cases were then selected for formal assessment by the appointed accreditation panel. This panel comprised of the head of Primary Care Commissioning for BCUHB, Chair of the LDC, Director of Dental Public Health and an Orthodontic Consultant. As the local orthodontic consultants/specialists were potentially involved in either training of the applicants and/or the provision of their treatment plans, it was felt that, in order to eliminate any potential bias or conflicts of interest, the orthodontic input to the accreditation panel would be from an orthodontic specialist from outside the region. It was necessary for this person to be experienced in training and treatment planning for non-specialists.
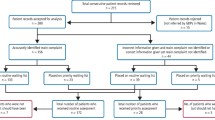
There were 15 expressions of interest received with 12 candidates submitting completed applications. These candidates were interviewed by the panel. Following the accreditation process, ten candidates were fully accredited, one was awarded provisional status and one failed to meet the accreditation criteria. Candidate feedback from the process was that although considerable work had been involved in completing the application and providing the ten consecutive cases, the actual process of writing up the cases provided an invaluable opportunity to critically appraise the treatment undertaken. The educational benefits of the process were also recognised.
Other GDP providers of NHS orthodontics who did not apply for accreditation, subsequently relinquished their orthodontic activity. In all cases, very small amounts of activity were involved (fewer than five [full] cases per year).
A robust local orthodontic committee structure has been important in providing support and guidance for the non-specialist practitioners applying for recognition through this process. Regular meetings of the LOC are held which are all inclusive involving orthodontic therapists, DwSIs, specialist practitioners and hospital consultant orthodontists. Peer assessment rating (PAR) scoring audit has been carried out involving all these providers and it is envisaged that this will continue.
Outcome
The core structure of these strategic changes has been the development of an effective Orthodontic Managed Clinical Network with BCUHB commissioners positively engaged with the group to ensure the success of these large and positive changes.
As a result of the above measures, the BCUHB has been able to develop a unique model for providing primary care NHS orthodontic treatment. It has increased service capacity, effectiveness and efficiency, which has stabilised the waiting times within the region for assessment and treatment in primary care without requiring the historic need for additional non-recurrent funding. It has also improved access issues previously experienced by patients in geographically remote areas. At the same time, it has developed robust monitoring processes to ensure that these treatments are performed to the highest clinical standards. Importantly, this model has taken a long term view and has provided stability to the provision of care cognisant of the Welsh Government's Prudent Health Care1 agenda.
References
Public Health Wales. Making prudent healthcare happen: Available online at http://www.prudenthealthcare.org.uk/ (accessed May 2017).
Sandham J S . Orthodontic Needs Assessment, Version 1. Public Health Wales. Available online at http://www2.nphs.wales.nhs.uk:8080/DentalPublicHTDocs.nsf/($All)/749487F6052F754180257C9F00440E64/$File/Ortho%20Need%20Assessment%20-%20Final%20Version.doc?OpenElement (accessed May 2017).
Office for National Statistics. 2011 Census. Available online at https://www.ons.gov.uk/census/2011census (accessed May 2017).
Welsh Government. Delivery Plan Together for Health: A National Oral Health Plan for Wales (2013–18). Available online at http://gov.wales/topics/health/nhswales/plans/oral-plan/?lang=en (accessed May 2017).
Richmond S . Review of the orthodontic services in Wales 2013–14. Public Health Wales. Available at http://gov.wales/docs/dhss/publications/150515dentalen.pdf (accessed May 2017).
National Assembly for Wales Health, Wellbeing and Local Government Committee. Orthodontic services in Wales. 2011. Available online at http://www.assembly.wales/Laid%20Documents/CR-LD8423%20-%20Health,%20Wellbeing%20and%20Local%20Government%20Committee%20Report%20on%20Inquiry%20into%20Orthodontic%20services%20in%20Wal-17022011-210599/cr-ld8423-e-English.pdf (accessed May 2017).
Acknowledgements
Mr. Tony Benton, Dental Contracts Manager, Betsi Cadwaladr University Health Board.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Lewis, B., Plunkett, D., Hickman, J. et al. Re-shaping NHS orthodontic provision – the North Wales experience. Br Dent J 222, 803–808 (2017). https://doi.org/10.1038/sj.bdj.2017.458
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2017.458