Key Points
-
Highlights that large numbers of implants are placed in the UK and worldwide.
-
Suggests their removal may need to be considered due to peri-implant disease.
-
Discusses variance in level of local bone loss for different implant removal techniques.
-
Reviews a number of techniques available.
Abstract
The use of dental implants is an accepted and predictable way of replacing missing or lost teeth. However, implants can and will fail and there are a variety of reasons why this occurs, which the practitioner should understand. In some instances failed implants may require removal and, therefore, practitioners should be aware of techniques that can be used to remove failed implants to potentially enable future rehabilitation of an edentulous region.
Similar content being viewed by others
Introduction
Since osseointegration was first described by Brånemark in 19771 and Schroeder in 19812 the use of dental implants to restore edentulous spaces has grown ever popular and has been supported by over 30 years of clinical research. Consequently the use of dental implants has revolutionised many aspects of dentistry.3,4 It has been estimated that at the turn of the millennium, over two million implants were being inserted annually in the US.5 In the UK the implant market is also well established.6
Implant success
There have been a number of studies and several meta-analyses indicating survival rates of dental implants are above 90%.7,8,9
These studies have demonstrated that implants are more successful in the mandible than the maxilla.9 They have also shown that implants placed for single tooth replacement were more successful than for implants placed in partial dentate patients, and they in turn were more successful than implants placed for overdentures.7 In addition, it has also been shown that implants are more successful in host bone than grafted bone.7,10
There are numerous studies in the literature that explore the well-established patient factors that affect failure/success rates which the clinician should be aware of when placing implants. Added to this are the many different combinations of implant systems, sites of fixture placement, designs of implant, widths and lengths of implant and surface morphology, meaning that it can be difficult to produce an overall failure rate for dental implants.
Implants are generally a successful and well-established treatment for tooth replacement; however, like everything in dentistry, things can and will fail and clinicians placing implants need to be well versed in interventions where implants have not succeeded.6
Implant failure
Despite implants having a high survival rate, it is increasingly evident that the successfully integrated implants are susceptible to disease which may lead to implant loss.11
Implant failure can either be described as early or late as stated by the Consensus Statement of the 6th European Workshop of Periodontology.12
Early failure is described as an implant that has failed and been unable to osseointegrate and these implants therefore tend to fail early. Late failure is described as an implant that has initially osseointegrated, however, osseointegration is lost and this could be due to disease of the marginal tissues or biomechanical overload, so these implants tend to fail later.13
There are a number of documented causes of implant failure that include prosthetic complications, implant mobility, excessive occlusal forces, fractured implant components, pain, inflammation, infection and neuropathy.14
Risk factors leading to implant failure need to be identified, modified or eliminated. This includes: maintaining good oral hygiene; stopping smoking; ensuring periodontal susceptible patients are under control and in an appropriate maintenance programme; ensuring implant fixtures are appropriately loaded and designed so they are cleansable and the patient is under regular review and in an appropriate maintenance/supportive programme, which will minimise implant failure.
There are multiple reasons identified in the literature for the failure of implants and the prostheses retained to these implants. Some of these will be briefly discussed and have been broadly categorised into the following groups:
-
Loss of integration
-
Implant factors
-
Positional failure
-
Clinician factors
-
Biomechanical.
Loss of integration
Failure of implants due to osseointegration can be divided into early or late failure. Early failure can occur due to a failure in osseointegration, and late failure due to bone loss or loss of osseointegration.15
Peri-implantitis is a well-established cause of late implant failure.5,8 It is an inflammatory lesion that affects the supporting bone as well as the surrounding soft tissues of a functioning implant, with progressive bone loss.16
One of the most frequently accepted factors in poor outcomes of dental implant treatment is smoking7,17,18,19,20 and it has been shown that smokers have an increased prevalence of peri-implant disease3 and, therefore, an increased likelihood of implant loss.7 Implant patients with previous experience of periodontitis are at an increased risk of getting peri-implantitis in comparison with non-periodontitis patients.21 It is also well documented that poor oral hygiene around implants and excess cement can contribute to peri-implantitis, thus compromising implant longevity.
Unstable diabetes has also been reported to affect osseointegration,22,23,24,25,26 as well as the use of corticosteroids and implant placement in immunosuppressed patients.25
The type of bone can affect the survival of implants with an increased incidence of failure in the presence of type IV bone compared with types I to III bone (as defined by Lekholm et al.).7
Radiation treatments to the head and neck region have also resulted in an increased incidence of implant loss, with higher failure noted in the maxilla than the mandible.7
Patients with parafunctional habits such as bruxism are at increased likelihood of premature implant failure.26
Implant factors
It has been demonstrated that implant dimensions can affect success, but this is dictated by the amount of available bone in the implant site. Shorter length (10 mm or less) implants have an increased likelihood of failure compared to longer length implants (greater than 10 mm in length).7 This increased length of bone to implant interface increases the mechanical resistance to masticatory forces.27 The diameter of implants has also been shown to affect success with wider diameter implants being more successful than narrow implants.27
A further factor that has been shown to affect success is implant form; the use of a threaded shape being more successful than smooth type implants28 due to threaded implants being able to transmit loading forces better than the smooth type implant.28 The threaded shaped implants also provide greater retention immediately after placement and maximise the potential area for osseointegration and provide good initial stability.28
Implants also have the potential to fracture which is often very difficult, if not impossible, to treat without removing the implant, although the incidence of this has been reported as being very low.7
Positional failure
Poor positioning of implants is a common cause of failure caused by poor treatment planning and/or poor clinical execution,29 and has been shown to affect implant success,29,30 with the incidence of this type of failure being estimated at 10%.8
The malposition of the implant can be in the following planes: mesio-distal, bucco-lingual and apical-coronal. Implant placement must be guided by the restoration it supports, and will ensure that the implant is placed in a position that can be restored predictably and aesthetically.12
Implants should be placed so that occlusal forces are loaded along the long axis of the implant and occlusal forces are evenly distributed. Malposition of the implant can lead to occlusal forces being placed unfavourably on the implant with potential biomechanical problems, which can lead to a number of complications such as abutment screw fracture29 and also the potential for peri-implant bone loss.
Consequently, placing implants correctly is important. The evidence suggests adequate separation between implants and teeth of at least 3 mm. This will allow more predictable soft tissue aesthetics and ensure an adequate blood supply to the bone and the natural tooth's periodontal ligament.31
Separation between implants has been suggested between 4–7 mm, to avoid bone necrosis.26,31
Clinical factors
The surgeon's experience has been demonstrated to have a major impact on the failure of implants,32 and has been shown to be an important causative factor in early implant failure.26,33 It has been shown that surgeons who have placed less than 50 implants are twice as likely to have early implant failure than those that have placed over 50 implants.34
Surgical trauma such as overheating the bone should be minimised and correct surgical techniques should be used;27 further discussions in this regard go beyond the scope of this article.
Surgeons with less experience are more likely to make poor decisions. The most common poor treatment planning decision includes placing implants into insufficient bone and using an implant with too small a diameter.30
Clinical decision making, including the design of the prosthesis supported by implants (which should be decided before implant placement) and the occlusion/occlusal scheme, should be considered as part of the design of the prosthesis, and can affect implant success.32,35 The subsequent timing of loading the implants also affects success.32
Regular recall and maintenance of implants is vital and should be stressed to the patient as well as the need for meticulous oral hygiene.27
Biomechanical factors
Implants can fail due to biomechanical factors, which can include loose abutment screws to fractured implant components. The main cause is often due to poor treatment planning and exposing implants to excessive forces.29
The majority of biomechanical problems can be dealt with, but in some instances these problems cannot be rectified and the implant is left unusable and non-functional. In some cases it may be decided that the implant needs to be removed.
This review demonstrates a variety of techniques documented within the literature that can be used to remove implants, and also highlights case reports where implants were removed.
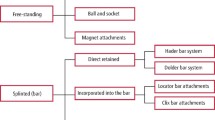
Techniques available for implant removal
There are a variety of techniques that can be used to remove implants. One of the main factors to consider is how well osseointegrated the implant is. Those that have failed due to a loss of osseointegration are usually much simpler and easier to remove. Those implants that are integrated are typically much more difficult and problematic. Where failed implants require removal, treatment should be as conservative as possible and try to minimise bone removal. This is particularly important if placement of a further implant fixture is planned. This, however, may not be possible; even when being conservative and using less invasive implant removal techniques, bone removal may be excessive and may lead to inadequate bone volume to place a further implant fixture. This may then necessitate the use of bone grafting methods to produce adequate bone volume.
Osseointegration failure
If an implant has failed to osseointegrate then it may be removed by rotating it anticlockwise using an implant driver, torque ratchet or even forceps.36 These measures are usually enough to facilitate implant removal without the need for further intervention. For implants that have osseointegrated, the use of the simple torque wrench will not be enough to facilitate removal.
Counter torque ratchet technique & reverse screw technique
Counter torque ratchet technique (CTRT) and the reverse screw technique (RST) may be useful where damage to the surrounding tissues is to be avoided.
Both of these techniques engage the implant and with a counter clockwise force, reverse screw the implant out of the bone.
Cases that are amenable to removal depend on the implant connection (external hex/internal hex), patency of the connections, implant diameter, implant geometry, implant location and the amount of osseointegrated bone around the implant.36
In CTRT a counter torque ratchet is used when the connection with the implant is intact and the implant is robust enough to be 'torqued out' without fracture. Care should be taken where implants are narrow and have less than 4 mm of length in dense cortical bone in order to avoid implant fracture. This technique requires that the connection component is firm and solid as there is a risk of destroying the connection using this technique. Consequently, the connection should not show signs of fatigue that could result in fracture of the implant.36
In cases where the implant connection is damaged or an external connection implant requires removal the CTRT technique may not be advisable and the RST technique should be adopted. A screw removal device is used to engage the implant.36
Figure 1 shows a reverse screw implant retrieval tool (Nobel Biocare); which was used to remove two implants that had fractured and were no longer useable. The retrieval tool engaged the internal thread and, using the hand torque with a reverse direction, removed the implants (Figs 2 and 3).
Figure 4 shows how the counter torque ratchet tool kit (Neobiotech Fixture Removal Kit, Neobiotech, Korea) was utilised to remove a fractured implant. The fractured portion was coronal and only extended 3-4 mm apically. The fractured implant wall was mobile and was removed before the implant was explanted.
The CTR tool kit is made up of three components; the first being the internal implant removal screw, which is screwed into the implant (Fig. 5). Second, the implant remover driver, which is screwed on the implant removal screw anticlockwise (Fig. 6). Lastly, the torque ratchet which has two torque gauges – one side measures the correct torque for the implant removal screw to be driven into the implant and the other side measures the correct torque for the removal of the final implant (Fig. 7).
The system has been designed to fit a large variety of implant systems and, therefore, is a universal kit and not implant specific. The correct implant removal screw is chosen according to the thread pitch of the implant connection to drive into the implant. This screw is one use only and essentially creates its own thread inside the implant – this is torqued to a maximum of 60 Ncm (Fig. 8). The implant remover driver is selected according to the implant platform. The implant remover driver has a thread inside it which screws down onto the implant removal screw – this is torqued to a maximum of 300 Ncm (Fig. 9). It is essential that when the torque wrench is used to remove the implant, the clinician turns it slowly anticlockwise working their way up to the maximum torque. Patients can find this slightly uncomfortable as the pressures exerted are high, therefore, a counterforce is necessary by supporting the patients jaw, but once the osseointegration has broken between the implant and the bone, the implant can be removed by hand (Fig. 10).
This is one of the most atraumatic ways of explanting an implant, preserving valuable surrounding bone for the future placement of another implant in the site.
Bone removal techniques
This can either be carried out using high speed burs, piezosurgical units or trephining burs.
It is recommended that as much bone as possible be preserved as this can help avoid or reduce the necessity of bone augmentation procedures. It may also allow placement of another implant if applicable, although replacement implants have been shown to have a decreased survival rate.37,38
Piezosurgery
Piezosurgery can be used to remove supporting bone around the implant to allow its removal. The advantage of the piezosurgery device is that it cuts shallow bone well, while preventing damage to soft tissue.39,40 It has also shown improved bone healing in comparison with high speed burs post-operatively.36 For deeper cuts into bone the piezosurgery instrument is less efficient,36 and where the cutting speed slows it is often wise to pause at intervals to prevent the tip overheating. Copious irrigation with saline is used throughout.
High speed burs
The traditional high speed bur can be used to remove bone efficiently; however, the air from the high speed turbine can be forced into the wound, creating surgical emphysema,41 and it is also invasive.36 Diamond burs are reported in the literature to be more favourable than tungsten carbide burs, and where important anatomical structures lie in the vicinity of surgery it is recommended that accurate images are taken, including cone beam computerised tomography (CBCT) scans where appropriate.36
Cutting with high speed burs can also cause pieces of the implant surface to be left in the wound site and should therefore be removed with regular irrigation.36
Trephines
Trephine burs can be used to remove implants, but this technique can be very invasive, and thus should be used only when absolutely necessary.
There are a variety of sizes of trephines and the smallest trephine should be used (the internal diameter of the trephine should be slightly larger than the implant to avoid engaging the implant body). The preferred cutting speed is 1200 rpm-1500 rpm.36 Once the coronal half of the bone has been removed, elevators, forceps and torque drivers can be used to remove the implant. A number of complications have been noted in the use of trephine burs including fatigue fracture of the mandible42 and osteomyelitis.43
Figure 11 shows a DPT of a patient's failing implants after 15 years of function. Removal of the fixed implant retained prosthesis confirmed two of the five implants had lost intergration and three had fractured (Fig. 12). The most distal left mandibular implant was left in-situ, due to its proximity to the mental nerve, but the other fractured implants were removed with a trephine (Fig. 13). Following three months of healing, four new implants were placed to retain a fixed implant prosthesis.
Combination techniques
Where possible, less invasive techniques such as CTRT and RST should be adopted in the first instance, and where these fail the use of piezosurgery and high speed burs can be utilised where necessary, until the procedure can be continued with the less invasive techniques in order to successfully remove the implant.
High frequency electro-surgery removal
It has been documented in a case report by Cunliffe et al.15 that another method for removal of osseointegrated implants is to use an ultra-high frequency mono-polar electro-surgery unit.11 This device is applied to the internal surface of the neck of the implant in order to cause a thermo-necrosis at the interface between bone and implant, thus facilitating implant removal. One week after the impulse was delivered the implant was then easily removed using a hand wrench. It is stated that by heating the tissue with a radio-frequency impulse, energy is absorbed into the tissues in two distinct ways: ohmic heating and di-electric heating. Ohmic heating is the process by which an electric current passes through a conductor (implant) releasing heat. Di-electric is the process in which a high-frequency alternating electric field heats a dielectric (implant) material.
This technique appears to be a very conservative approach to the removal of implants and does not appear to be particularly destructive of bone, making it an attractive option for both patient and clinician, especially if the implant is to be replaced later. Despite the apparent advantages of this technique, however, there are potential pitfalls to electrosurgical removal of implants, especially unwanted necrosis of surrounding bone due to excess heating. Furthermore, evidence is limited to support this technique and it is the recommendation of the authors of the case report11 that a laboratory-based project to assess the effects of electrosurgery on osseointegrated implants is needed to further assess the technique.15
Laser (Er,Cr: YSGG)
The use of a laser to explant dental implants in a single patient that had associated peri-implantitis has been described in a case report by Smith et al.44 The erbium, chromium-doped: yttrium, scandium, gallium, and garnet (Er,Cr:YSGG) laser was used to cut sufficient bone for the implants to then be removed using forceps.44
The article reported very good post-operative pain control, with the patient not requiring any analgesia afterwards, along with excellent haemostatic control during the procedure, and the procedure itself described as being technically easy to perform.44
The mechanism of cutting with the Er,Cr:YSGG laser is via micro-explosion which is created by the laser energy being absorbed by the air-water spray at the tissue surface; this process is called the hydrokinetic effect and produces clean cuts without thermal damage.44 The Er,Cr:YSGG laser has been demonstrated to effectively cut bone without burning, melting or altering the calcium to phosphorus ratio of the irradiated bone.45 Lasers have been used in dentistry for a number of reasons, including periodontal treatment of both teeth and implants.46
The results shown in the case report suggest that laser removal of implants is a medium that may grow in popularity in future, especially as more cases in the literature emerge.
Conclusion
There are numerous methods for the removal of implants now reported in the literature. Implant removal should be undertaken in the most atraumatic and conservative manner available. The aim of implant removal should be to preserve as much alveolar bone as possible, prevent unwanted post-operative side effects and ensure that any option for future replacement of the tooth by implant or otherwise has the best possible prognosis.
It is the recommendation of the authors that practitioners should always stay within their comfort zone and competency. When clinical cases go beyond the practitioner's comfort zone they should refer to a more experienced practitioner to ensure that the patient receives optimal treatment.
There are some promising reports in the literature that may hold the key to a 'gold standard' of implant removal emerging in future, however, more research is needed at present in order to identify the best technique for both clinicians and patients alike.
References
Branemark P I, Hansson B O, Adell R et al. Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-year period. Scand J Plast Reconstr Surg Suppl 1977; 16: 1–132.
Schroeder A, van der Zypen E, Stich H, Sutter F . The reactions of bone, connective tissue, and epithelium to endosteal implants with titanium-sprayed surfaces. J Maxillofac Surg 1981; 9: 15–25.
Algraffee H, Borumandi F, Cascarini L . Peri-implantitis. Br J Oral Maxillofac Surg 2012; 50: 689–694.
Demarosi F, Leghissa G C, Sardella A, Lodi G, Carrassi A . Localised maxillary ridge expansion with simultaneous implant placement: a case series. Br J Oral Maxillofac Surg 2009; 47: 535–540.
Klinge B, Hultin M, Berglundh T . Peri-implantitis. Dent Clin North Am 2005; 49: 661–676.
Levin L . Dealing with dental implant failures. J Appl Oral Sci 2008; 16: 171–175.
ADA Council on Scientific Affairs. Dental endosseous implants: an update. J Am Dent Assoc 2004; 135: 92–97.
Goodacre C J, Bernal G, Rungcharassaeng K, Kan J Y . Clinical complications with implants and implant prostheses. J Prosthet Dent 2003; 90: 121–132.
Lindh T, Gunne J, Tillberg A, Molin M . A meta-analysis of implants in partial edentulism. Clin Oral Implants Res 1998; 9: 80–90.
Becktor J P, Isaksson S, Sennerby L . Survival analysis of endosseous implants in grafted and nongrafted edentulous maxillae. Int J Oral Maxillofac Implants 2004; 19: 107–115.
Tonetti M . Risk factors for osseodisintegration. Periodontology 2000 1998; 17: 55–62.
Lindhe J, Meyle J . Peri-implant diseases: consensus report of the 6th European Workshop on Periodontology. J Clin Periodontol 2008; 35(Suppl 8): 282–285.
Chen S, Darby I . Dental implants: maintenance, care and treatment of peri-implant infection. Aust Dent J 2003; 48: 212–220.
American Academy of Periodontology. Parameter on placement and management of the dental implant. J Periodontol 2000; 71: 870–872.
Cunliffe J, Barclay C . Removal of a dental implant: An unusual case report. J Dent Implant 2011; 1: 22–25.
Lindhe J, Meyle J . Peri-implant diseases: Consensus Report of the Sixth European Workshop on Periodontology. J Clin Periodontol 2008; 35: 282–285.
Chuang S K, Wei L J, Douglass C W, Dodson T B . Risk factors for dental implant failure: a strategy for the analysis of clustered failure-time observations. J Dent Res 2002; 81: 572–577.
Quirynen M, De Soete M, van Steenberghe D . Infectious risks for oral implants: a review of the literature. Clin Oral Implants Res 2002; 13: 1–19.
Bain C A, Moy P K . The association between the failure of dental implants and cigarette smoking. Int J Oral Maxillofac Implants 1993; 8: 609–615.
Lindquist L W, Carlsson G E, Jemt T . Association between marginal bone loss around osseointegrated mandibular implants and smoking habits: a 10-year follow-up study. J Dent Res 1997; 76: 1667–1674.
Schou S . Implant treatment in periodontitis-susceptible patients: a systematic review. J Oral Rehabil 2008; 35: 9–22.
Farzad P, Andersson L, Nyberg J . Dental implant treatment in diabetic patients. Implant Dent 2002; 11: 262–267.
Balshi T J, Wolfinger G J . Dental implants in the diabetic patient: a retrospective study. Implant Dent 1999; 8: 355–359.
Fiorellini J P, Chen P K, Nevins M, Nevins M L . A retrospective study of dental implants in diabetic patients. Int J Periodontics Restorative Dent 2000; 20: 366–373.
Fujimoto T, Niimi A, Sawai T, Ueda M . Effects of steroid-induced osteoporosis on osseointegration of titanium implants. Int J Oral Maxillofac Implants 1998; 13: 183–189.
el Askary A S, Meffert R M, Griffin T . Why do dental implants fail? Part I. Implant Dent 1999; 8: 173–185.
Porter JA, von Fraunhofer JA . Success or failure of dental implants? A literature review with treatment considerations. Gen Dent 2005; 53: 423–432.
Lee JH, Frias V, Lee K W, Wright RF . Effect of implant size and shape on implant success rates: a literature review. J Prosthet Dent 2005; 94: 377–381.
Chee W, Jivraj S . Failures in implant dentistry. Br Dent J 2007 10; 202: 123–129.
Laine P, Salo A, Kontio R, Ylijoki S, Lindqvist C, Suuronen R . Failed dental implants- clinical, radiological and bacteriological findings in 17 patients. J Craniomaxillofac Surg 2005; 33: 212–217.
Misch C E . Dental implant prosthetics. St. Louis: Elsevier-Mosby. 2005.
Preiskel H W, Tsolka P . Treatment outcomes in implant therapy: the influence of surgical and prosthodontic experience. Int J Prosthodont 1995; 8: 273–279.
Esposito M, Hirsch J M, Lekholm U, Thomsen P . Biological factors contributing to failures of osseointegrated oral implants. (II). Etiopathogenesis. Eur J Oral Sci 1998; 106: 721–764.
Morris H F, Manz M C, Tarolli J H . Success of multiple endosseous dental implant designs to second-stage surgery across study sites. J Oral Maxillofac Surg. 1997; 55(12 Suppl 5): 76–82.
Misch C E, Suzuki J B, Misch-Dietsh F M, Bidez M W . A positive correlation between occlusal trauma and peri-implant bone loss: literature support. Implant Dent 2005; 14: 108–116.
Froum S, Yamanaka T, Cho S C, Kelly R, St James S, Elian N . Techniques to remove a failed integrated implant. Compend Contin Educ Dent 2011; 32: 22–26: 28–30.
Grossmann Y, Levin L . Success and survival of single dental implants placed in sites of previously failed implants. J Periodontol 2007; 78: 1670–1674.
Machtei E E, Horwitz J, Mahler D, Grossmann Y, Levin L . Third attempt to place implants in sites where previous surgeries have failed. J Clin Periodontol 2011; 38: 195–198.
Vercellotti T . Piezoelectric surgery in implantology: a case report-a new piezoelectric ridge expansion technique. Int J Periodontics Restorative Dent 2000; 20: 358–365.
Wallace S S, Mazor Z, Froum S J, Cho S C, Tarnow D P . Schneiderian membrane perforation rate during sinus elevation using piezosurgery: clinical results of 100 consecutive cases. Int J Periodontics Restorative Dent 2007; 27: 413–419.
Reznick J B, Ardary W C . Cervicofacial subcutaneous air emphysema after dental extraction. J Am Dent Assoc 1990; 120: 417–419.
Schroeder A, Sutter F, Buser D et al. Oral Implantology. Basics, ITI Hollow Cylinder System. Stuttgart, Germany: Georg Thieine Verlag, 1996; 445–476.
Esposito M, Hirsch J, Lekholm U, Thomsen P . Differential diagnosis and treatment strategies for biologic complications and failing oral implants: a review of the literature. Int J Oral Maxillofac Implants 1999; 14: 473–490.
Smith L P, Rose T . Laser explantation of a failing endosseous dental implant. Aust Dent J 2010; 55: 219–222.
Kimura Y, Yu D G, Fujita A, Yamashita A, Murakami Y, Matsumoto K . Effects of erbium, chromium: YSGG laser irradiation on canine mandibular bone. J Periodontol 2001; 72: 1178–1182.
Aoki A, Sasaki KM, Watanabe H, Ishikawa I . Lasers in non-surgical periodontal therapy. Periodontol 2000 2004; 36: 59–97.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Bowkett, A., Laverty, D., Patel, A. et al. Removal techniques for failed implants. Br Dent J 220, 109–114 (2016). https://doi.org/10.1038/sj.bdj.2016.88
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2016.88
This article is cited by
-
A systematic review on removal of osseointegrated implants: un update
BMC Oral Health (2023)
-
Implant removal using thermal necrosis—an in vitro pilot study
Clinical Oral Investigations (2021)