Abstract
Introduction:
This was a retrospective monocentric study conducted at Centre Calvé, France, with the objective of evaluating the effectiveness of a 5-day course of antibiotics for symptomatic (mild urinary tract infection, UTI) or asymptomatic (aBact) bacteriuria in patients with spinal cord injury on intermittent catheterization.
Case presentation:
This study was conducted from May 2013 to September 2016. Antibiotic selection always followed culture collection and analysis of antibiograms. Patients with febrile UTI (>38°5) or recent history of urolithiasis were excluded.
Discussion:
Fifty-seven patients underwent 111 5-day courses of antibiotics. The two main bacteria involved were Escherichia coli and Klebsiella Pneumoniae. Most commonly prescribed antibiotics were cephalosporins, cotrimoxazole, fluoroquinolones and nitrofurantoins. On day 4 of the antibiotic course, bacteria were eradicated in 99% of cases. Clinical cure occurred in all patients by day 5 (end of treatment). After treatment, recurrence of UTI occurred in 16% of patients at week 3, 38% at week 6 and 50% at week 9. This rate was not significantly different from patients initially treated for aBact (20%, 35% and 44%, respectively). The UTI-free period was significantly shorter after treatment for aBact (45.5 days) than after treatment for UTI (53.7 days). None of the following characteristics were found to be risk factors for UTI: level or severity of lesion, gender, voiding mode, use of anticholinergic drugs and time since lesion. Results of this study support the use of a short 5-day course of antibiotics to treat mild UTI in patients with spinal cord injury, and provide further evidence against treatment of aBact.
Similar content being viewed by others
Introduction
Urinary tract infection (UTI) is the most common medical complication in patients with spinal cord injury (SCI), both in the acute phase and throughout the patient’s lifetime.1–3 Intermittent catheterization (IC) has become the standard voiding method for patients with neurogenic bladders as it is associated with fewer urologic complications than other bladder management strategies such as indwelling catheters.1,3 However, lower urinary tract colonization (asymptomatic bacteriuria—aBact) is common in patients with SCI, both at home and in hospital, with a prevalence ranging from 50 to 90%.4–6
The optimal duration of therapy for UTI in patients with SCI has not been established. Patients should be treated with narrow spectrum antibiotics (ATBs) when possible, for the shortest duration that is clinically safe.7 It is a general belief that 3–5 days of ATB treatment is probably effective in the treatment of mild UTI1 and in patients with chronic SCI.8 The Infectious Diseases Society of America recommends a 7-day course of ATBs for patients on IC who have a prompt resolution of symptoms, and a 10–14-day course for those with a delayed response. A 5-day course of levofloxacin may be considered for patients who are not severely ill.9
The potential benefits of short-course therapy could include a reduction in adverse effects, antimicrobial resistance and cost.10 Febrile UTI, accompanied by fever and chills, indicates involvement of the upper urinary tract and warrants a longer duration of ATB therapy than in the case of mild symptoms.1
The aim of this study was to evaluate the effectiveness of a 5-day ATB course for mild UTI in patients with SCI on IC. The secondary aims were to evaluate clinical cure, relapse and reinfection rates, and to compare between symptomatic and asymptomatic groups.
Materials and methods
This retrospective study was conducted from May 2013 to September 2016 in the SCI rehabilitation unit of the Centre Calve.
Inpatients with neurogenic bladder were enrolled if they met the following inclusion criteria:
-
Patients using IC (usually five times a day, performed either by the patient or by the nurse, or twice a day when associated with spontaneous voiding);
-
Prescription of a 5-day course of ATBs, either for symptomatic (UTI) or asymptomatic (aBact) bacteriuria; aBact is treated before invasive urological procedures (cystoscopy or urodynamics) or surgery for pressure sores, or before starting hydrotherapy to comply with our hospital’s infectious disease policy;
-
Presence of UTI compatible with cystitis (mild illness with urinary, bladder signs, mild fever without chills);
-
Inpatients with planned stays of more than a further 60 days.
Exclusion criteria
-
Pyelonephritis or febrile UTI (>38°5) with chills and altered general condition;
-
Recent history of urolithiasis;
-
Recurrent need for ATB for other reasons (mostly patients with high cervical lesions and tracheostomy).
Urine cultures (UC) were systematically performed before ATB therapy and monitored on day 4 of the treatment. Urine samples were collected by IC using standard procedures (either clean intermittent self-catheterization or clean IC by the nurses).
The treatment of choice was targeted ATB therapy following susceptibility testing. In case of empiric ATB therapy, only cases with infecting strains susceptible to the ATB were included in the analysis.
For urine cultures, the criteria of the American Paraplegia Society were followed:
-
Significant bacteriuria—a threshold of 102 cfu ml−1 for patients on IC,
-
UTI—significant bacteriuria, at least one clinical sign or symptom, and leukocyturia >103 per ml and
-
aBact: significant bacteriuria without any clinical signs.
To evaluate the effectiveness of the ATB treatment, the following definitions were used:
-
On day 4 of the ATB course:
-
Microbiological cure was defined as UC with negative results;
-
Eradication of bacteria was defined as the disappearance of the causative bacteria in the control UC; and
-
Treatment failure was defined as the persistence of significant bacteriuria with the causative bacteria in the control UC.
-
-
Clinical cure was defined as the complete resolution of symptoms and clinical signs related to UTI without the need for further ATB therapy.
-
Relapse was defined as recurrence of UTI due to a similar bacterial species to that found at the onset of the 5-day ATB therapy; and
-
Reinfection was defined as recurrence of UTI due to different bacterial species to that found at the onset of the 5-day ATB therapy.
The following information was obtained from the medical chart of each patient—drug treatment, mono or dual therapy, diagnosis (UTI or aBact), clinical cure at end of therapy, bacteriological data and clinical data (including type of neurological deficit and voiding method).
End points
The primary outcome was occurrence of UTI at both the short- (3 weeks) and long-term (6 and 9 weeks) follow-ups, and the duration of UTI-free urine.
The secondary outcomes were microbiological cure and eradication of bacteria on day 4 of the ATB course, clinical cure at the end of therapy for UTI (day 5), and relapse and reinfection rates at the short- and long-term follow-ups.
The time from the end of the 5-day ATB course to the onset of another 5-day ATB course or discharge was analysed. Time data were expressed as means, and further categorized into three time slots—3 weeks (W3)=short-term follow-up, and 6 (W6) and 9 weeks (W9)=long-term follow-up.
Patients were divided into four groups according to the outcome at the end of the 5-day ATB course:
-
Group 1, recurrence of a treated UTI (UTI to UTI)
-
Group 2, occurrence of UTI after treatment for aBact (aBact to UTI)
-
Group 3, treatment for aBact after UTI (UTI to aBact)
-
Group 4, consecutive treatments for aBact (aBact to aBact)
Statistical analysis
Data analyses were carried out using the SAS 9.3 software (SAS Institute Inc., Cary, NC, USA). Univariate analyses were carried out using χ2 and Fisher exact tests, including all variables known to be associated with UTI (that is, statistically or clinically significant)—gender, age, type of neurological deficit, type of voiding and positive blood culture. Risk factors for developing UTI and the duration of UTI-free urine following ATB treatment for each group were assessed using a Cox regression model.
Statistical significance was defined as P<0.05.
Results
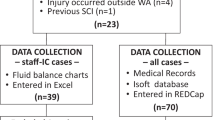
Fifty-seven patients underwent 111 5-day courses of ATBs during the study period. Their baseline characteristics are listed in Table 1. Thirty-two patients had a single 5-day ATB course, 12 had 2 courses and 5 had 3 courses, whereas the remaining 8 patients had between 4 and 7 courses.
The population was mostly male (n=43), composed mostly of young adults (mean age: 40.9 years old ±16.8) with paraplegia (n=38) and complete motor lesions (n=38). Time since injury was a mean 18.4 months±49.1, with 19 patients in the acute phase (<3 months since injury). Voiding method was IC, alone (n=41 self-IC and n=10 by nurse), or associated with reflex voiding (n=6). Most patients took anticholinergic drugs (n=36), whereas 10 had had concomitant botulinum toxin injections for neurogenic detrusor overactivity.
Table 2 presents the patient characteristics, microorganism samples and ATB treatments for all 111 ATB courses in the four groups. There were no statistical differences between the four groups.
The two main bacteria involved were Escherichia coli (n=60; 52%) and K. Pneumoniae (n=24; 21%). Five UCs were polymicrobial with two bacteria.
There were 94 targeted and 17 empiric ATB therapies. The most commonly prescribed ATBs were third-generation cephalosporins (n=43; 39%), cotrimoxazole (n=32; 29%), fluoroquinolones (n=17; 15%) and nitrofurantoins (n=16; 15%). Dual therapy was prescribed in five cases.
Table 3 shows the primary and secondary outcomes for the four groups. Ninety-seven UCs were performed on day 4 of the ATB treatment. Microbiological cure was found in 91, whereas 6 were positive. Of these 6, 5 were contaminated with another bacteria, and in 1 the treatment failed. There was thus a 99% eradication rate (96 out of 97). Clinical cure occurred in all patients at the end of the 5-day treatment for UTI.
The UTI-free period was not significantly shorter after treatment of aBact (45.5 days) than that after treatment of UTI (53.7 days). Relapses (n=45) occurred slightly more often than reinfections (n=37). Antimicrobial sensitivity testing showed that 18% of bacteria were resistant to the ATB used (8/45) in cases of relapse and 30% (11/37) in cases of reinfection. Recurrences of UTI (group 1) were mainly cystitis treated with a 5-day course of ATBs (37/38); one was a severe UTI that appeared at day 29, treated with a 10-day dual ATB course.
The rate of UTI was not significantly different after treatment of UTI or aBact (Table 4). Recurrence of UTI occurred in 16% of patients at W3, 38% at W6 and 50% at W9, compared to 20%, 35% and 44%, respectively, for occurrence of UTI after treated aBact. In the aBact group, there was no statistical difference in the occurrence of UTI between those who subsequently underwent invasive urologic exams (n=20) and those who underwent non-urologic procedures (n=21) (Table 5), although the rate was slightly higher at W3 and W6 (24% vs 15% and 41% vs 29%) in those who underwent invasive urologic exams.
Data from groups G1 and G2 (ending with UTI) were further analysed to determine the risk factors for developing UTI in this population. There was no significant difference in UTI-free periods after ATB treatment for UTI or aBact (P=0.51) (Figure 1). No risk factors could be identified among level (tetraplegics vs paraplegics, P=0.98) or severity (ASIA Injury Scale grade, P=0.55) of lesion, gender (P=0.27), voiding modes (IC by patient, IC by nurse, spontaneous voiding and additional IC), P=0.54, use of anticholinergic drugs (P=0.27) or time since lesion (P=0.67).
Discussion
Even though UTI is the most common complication and a significant cause of morbidity in patients with SCI, the optimal duration of therapy for UTI has not been established. In this retrospective study, we showed that, following eradication of bacteria and clinical cure, the recurrence rate of UTI was limited to 16% in the short term, and 38% in the long term, suggesting that a 5-day course of ATBs might be suitable for the management of mild UTI.
Eradication of bacteria/clinical cure
There are limited data on the mid-treatment effect of ATB in patients with SCI. When ATB therapy is determined according to susceptibility, the eradication rate varies between 54 (7–14-day ATB courses in catheter-free patients)11 and 97% (unpublished data). Stannard et al.12 reported similar rates (97%) in patients on ciprofloxacin (5-day ATB courses in patients on IC and with indwelling catheters), as did Dow et al.10(96%, 3-day ATB course in patients on IC). The present study confirms the high rate (99%) of eradication of bacteria after 3 days of targeted ATB in mild UTI. Evaluation of treatment effectiveness can be achieved using simple dipsticks, followed by UC only if the results are positive (unpublished data).
Eradication of bacteria is the key to confirm the effectiveness of ATB therapy. However, from the patients’ perspective, disappearance of symptoms is clearly the most important parameter.13 The relative importance of microbiological and clinical outcomes is an important issue. Confirmation of eradication of bacteria at mid-treatment is necessary to ensure that ATBs are correctly used and that it certainly helps reduce bacteria resistance. However, microbiological cure cannot be the only approach, especially when subjects are inpatients on SCI wards where aBact is common, as well as exposure to nosocomial pathogens. Reinfection with another bacteria can therefore occur very easily. A prompt clinical response with disappearance of signs and symptoms of UTI, usually on day 2 or 3 of ATB therapy, is further proof of ATB efficacy and is reassuring for both patients and clinicians.
Treatment duration
Studies are rare in patients with SCI on IC.
A study by Mohler et al.,14 involving 46 patients, compared a 3-day course with a 10-day course of ATBs prescribed following antimicrobial susceptibility testing (mostly trimethoprim–sulfamethoxazole) for aBact and UTI. Both groups had similar rates of cure, microbiologic persistence and relapse.
In a recent retrospective study of 112 patients, Dinh et al.15 found no difference in cure rates for febrile UTI treated with <10 days, between 10 and 15 days, and more than 15 days of ATBs. The results suggested that a treatment duration of 8 days was appropriate in the case of febrile UTI.
In a randomized, double-blinded, placebo-controlled trial, Dow et al.10 compared 3-day and 14-day courses of ciprofloxacin (250 mg twice daily) for the treatment of mild UTI in a group of 60 patients. At the long-term follow-up (6 weeks), microbiological cure was significantly greater in patients who received 14 days of treatment compared with those who received 3 days of treatment. Also, microbiological relapse and symptomatic relapse both occurred more frequently in patients treated for 3 days. The authors concluded that longer treatment durations lead to improved clinical and microbiological outcomes. However, the percentages of patients with clinical cure at both short-term and long-term follow-ups were similar for both study arms, raising the possibility that a 2-week ATB regimen may not be necessary, and a shorter ATB regimen that exceeds 3 days could be sufficient.16 Further, when their results were adjusted for clinical cure and bacteria eradication, as in the present study (that is, exclusion of treatment failure due to bacteria resistant to ciprofloxacin and patients lost to follow-up), rates of UTI were then of 27% (7/26) at W3 and 58% (15/26) at W6 for the 3-day arm, and of 16% (3/19) at W3 and 37% (7/19) at W6–8 for the 14-day arm. The rates of UTI of 16% at W3 and 38% at W6 in the present study are strikingly similar to those found in the 14-day arm treatment.
For mild, non-febrile UTI, most experts and scientific societies promote durations of ATBs between 3 and 7 days.1,8,9 Our results provide some evidence that a 5-day course of ATBs might be suitable, when prompt microbiological (UC negative at mid-treatment) and clinical (disappearance of symptoms) responses occur. Longer durations of therapy are required for more severe (febrile) UTIs that indicate involvement of the upper urinary tract, or in patients with a delayed response.8,9,15
There was no difference in the recurrence rate of UTI between patients in the acute and chronic phases of SCI, either at W3 (4/14 vs 7/56) or at W6 (5/13 vs 18/48). Thus, there is no rationale for a longer duration of treatment in the acute phase.8
Risk factors for developing UTI in patients with SCI have been identified, by order of importance, as vesicoureteral reflux, dependence, chronic permanent catheterization, cervical SCI and invasive procedures carried out without ATB prophylaxis.17 In the present study, the voiding mode was controlled, and no significant risk factors were found. However, the statistical analysis must be interpreted with care in view of the heterogeneity and the relatively small size of the sample studied.
Treating bacteriuria
The prevalence of bacteriuria in patients with SCI is high, ranging from 50 to 90%, irrespective of the technique used for bladder emptying.4–6 Despite this high prevalence, the incidence of UTI is relatively low.18 Furthermore, studies in patients with aBact and IC showed similar rates of UTI and recurrence of aBact at follow-up, whether or not prophylactic ATBs were administered.14,19 This explains why most authorities and consensus guidelines recommend against routine screening and treatment of aBact in patients with SCI because of the unclear long-term benefit and because treatment increases the selective pressure for drug resistance.1,20–22 The comparison of outcomes following treatment for aBact and UTI in the present study supports this view, with no statistical difference in the rates of UTI, in the short term or in the long term (Table 4). Moreover, UTI-free periods were shorter after treatment of aBact than UTI.
ATB prophylaxis is recommended by the European Urologic Association in ‘high-risk patients’ before invasive urological procedures (cystoscopy or urodynamics), with risk factors identified as a history of UTI or urogenital infection, use of indwelling catheters or bacterial burden.23 This provides a rationale for the administration of ATB in the case of aBact before urodynamic assessments or intradetrusor injections in patients with SCI;24 however, evidence is poor and recent studies suggest otherwise.25 The 24% rate of UTIs found in the present study following urological procedures, despite prophylactic ATBs at W3, may seem high (Table 5). If the follow-up had been shorter, no UTIs would have been diagnosed after 7 days, and only 2 after 14 days, compared to 5 at W3. This suggests that the UTIs may not be the result of the urological procedures, but were probably related to the high bacterial burden associated with IC.
Bacteria and ATB
The bacteria found in this study were the usual ones found on SCI wards. The Enterobacteriaceae family represents the most commonly isolated organisms in the neurogenic population. Within this family, there is a predominance of E. coli (usually around 50%) followed by Klebsiella.7,26 Gram-negative bacteria (that is, E. coli) tend to cause severe inflammation associated with intense leukocyturia.2
ATB stewardship is of paramount importance. In our practice, ATB selection always follows culture collection and analysis of antibiograms. Third-generation cephalosporin, trimethoprim–sulfamethoxazole, nitrofurantoin or quinolone are usually appropriate in the population with SCI.7,8
Conclusion
In patients with SCI and on IC, a 5-day course of ATBs was associated with a high rate of eradication of causative bacteria (99%) and clinical cure (100%) at the end of the therapy. Recurrence rates of UTI at the short-term (16%) and long-term (38%) follow-ups were similar to those in other studies. These data support short-duration courses of ATBs for the treatment of mild UTI, as long as prompt microbiological (UC negative at mid-treatment) and clinical (disappearance of symptoms) responses occur. These results should be confirmed by randomized trials.
References
Cardenas DD, Hooton TM . Urinary tract infection in persons with spinal cord injury. Arch Phys Med Rehabil 1995; 76: 272–280.
Ronco E, Denys P, Bernede-Bauduin C, Laffont I, Martel P, Salomon J et al. Diagnostic criteria of urinary tract infection in male patients with spinal cord injury. Neurorehabil Neural Repair 2011; 25: 351–358.
Wyndaele JJ . Intermittent catheterization: which is the optimal technique? Spinal cord 2002; 40: 432–437.
Cameron AP, Rodriguez GM, Schomer KG . Systematic review of urological follow up after spinal cord injury. J Urol 2012; 187: 391–397.
Colgan R, Nicolle LE, McGlone A, Hooton TM . Asymptomatic bacteriuria in adults. Am Fam Physician 2006; 74: 985–990.
Hoffman JM, Wadhwani R, Kelly E, Dixit B, Cardenas DD . Nitrite and leukocyte dipstick testing for urinary tract infection in individuals with spinal cord injury. J Spinal Cord Med 2004; 27: 128–132.
Vigil HR, Hickling DR . Urinary tract infection in the neurogenic bladder. Transl Androl Urol 2016; 5: 72–87.
Everaert K, Lumen N, Kerckhaert W, Willaert P, van Driel M . Urinary tract infections in spinal cord injury: prevention and treatment guidelines. Acta Clin Belg 2009; 64: 335–340.
Hooton TM, Bradley SF, Cardenas DD, Colgan R, Geerlings SE, Rice JC et al. Diagnosis, prevention, and treatment of catheter-associated urinary tract infection in adults: 2009 International Clinical Practice Guidelines from the Infectious Diseases Society of America. Clin Infect Dis 2010; 50: 625–663.
Dow G, Rao P, Harding G, Brunka J, Kennedy J, Alfa M et al. A prospective, randomized trial of 3 or 14 days of ciprofloxacin treatment for acute urinary tract infection in patients with spinal cord injury. Clin Infect Dis 2004; 39: 658–664.
Waites KB, Canupp KC, DeVivo MJ . Eradication of urinary tract infection following spinal cord injury. Paraplegia 1993; 31: 645–652.
Stannard AJ, Sharples SJ, Norman PM, Tillotson GS . Ciprofloxacin therapy of urinary tract infections in paraplegic and tetraplegic patients: a bacteriological assessment. J Antimicrob Chemother 1990; 26 (Suppl F): 13–18.
Gupta K, Hooton TM . Duration of therapy for urinary tract infection: the long and the short of it. Clin Infect Dis 2004; 39: 665–666.
Mohler JL, Cowen DL, Flanigan RC . Suppression and treatment of urinary tract infection in patients with an intermittently catheterized neurogenic bladder. J Urol 1987; 138: 336–340.
Dinh A, Toumi A, Blanc C, Descatha A, Bouchand F, Salomon J et al. Management of febrile urinary tract infection among spinal cord injured patients. BMC Infect Dis 2016; 16: 156.
Darouiche RO, Al Mohajer M, Siddiq DM, Minard CG . Short versus long course of antibiotics for catheter-associated urinary tract infections in patients with spinal cord injury: a randomized controlled noninferiority trial. Arch Phys Med Rehabil 2014; 95: 290–296.
Esclarin De Ruz A, Garcia Leoni E, Herruzo Cabrera R . Epidemiology and risk factors for urinary tract infection in patients with spinal cord injury. J Urol 2000; 164: 1285–1289.
Nicolle LE . Asymptomatic bacteriuria: review and discussion of the IDSA guidelines. Int J Antimicrob Agents 2006; 28 (Suppl 1): S42–S48.
Maynard FM, Diokno AC . Urinary infection and complications during clean intermittent catheterization following spinal cord injury. J Urol 1984; 132: 943–946.
Morton SC, Shekelle PG, Adams JL, Bennett C, Dobkin BH, Montgomerie J et al. Antimicrobial prophylaxis for urinary tract infection in persons with spinal cord dysfunction. Arch Phys Med Rehabil 2002; 83: 129–138.
Nicolle LE, Bradley S, Colgan R, Rice JC, Schaeffer A, Hooton TM . Infectious Diseases Society of America Guidelines for the Diagnosis and Treatment of Asymptomatic Bacteriuria in Adults. Clin Infect Dis 2005; 40: 643–654.
NIDRR. National Institute on Disability and rehabilitation research Consensus Statement (NIDRR). The prevention and management of urinary tract infections among people with spinal cord injuries. J Am Par Soc 1992; 33: 194–204.
Grabe M, Bartoletti R, Bjerklund-Johansen TE, Cai T, Çek HM, Koves B et al. Guidelines on Urological Infections: European Association of Urology. 2015. Available at: http://uroweb.org/wp-content/uploads/19-Urological-infections_LR2.pdf.
Bothig R, Fiebag K, Thietje R, Faschingbauer M, Hirschfeld S . Morbidity of urinary tract infection after urodynamic examination of hospitalized SCI patients: the impact of bladder management. Spinal Cord 2013; 51: 70–73.
Weglinski L, Rouzaud C, Even A, Bouchand F, Davido B, Duran C et al. Prospective evaluation of antibiotic treatment for urological procedure in patients presenting with neurogenic bladder. Med Mal Infect 2016; 46: 300–307.
Yoon SB, Lee BS, Lee KD, Hwang SI, Lee HJ, Han ZA . Comparison of bacterial strains and antibiotic susceptibilities in urinary isolates of spinal cord injury patients from the community and hospital. Spinal Cord 2014; 52: 298–301.
Acknowledgements
We are grateful to Dr Vincke Bernard for statistical assistance and to Johanna Robertson for revision of the English.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Previnaire, JG., Le Berre, M., Hode, E. et al. A 5-day antibiotic course for treatment of intermittent catheter-associated urinary tract infection in patients with spinal cord injury. Spinal Cord Ser Cases 3, 17017 (2017). https://doi.org/10.1038/scsandc.2017.17
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/scsandc.2017.17