Abstract
Introduction:
Retro-odontoid mass rarely occur in patients with noninflammatory retro-odontoid lesions without atlantoaxial instability. We describe a rare case of retro-odontoid mass without atlantoaxial instability operated on by a transdural approach.
Case Presentation:
The patient was an 83-year-old man who presented with a retro-odontoid mass causing symptomatic cervical myelopathy. Preoperative magnetic resonance imaging (MRI) revealed that the mass was severely compressing the spinal cord. We operated on it via a C1 laminectomy and performed tumor resection by a transdural approach. Pathological findings from the operative specimen confirmed the diagnosis; histopathological examination revealed that the mass contained fibrinoid material, and collagenous tissue with myxoid changes, but no granulation or a granulomatous lesion. Postoperative MRI confirmed spinal cord decompression. The patient’s symptoms were alleviated, and he has not had a recurrence or cervical instability in the 7 years since his surgery.
Discussion:
We successfully used a transdural approach in the present case and have observed no recurrence for 7 years postoperatively. C1 laminectomy is reportedly beneficial, especially for elderly patients, given the risk of other surgical options using an anterior transoral approach or posterior fusion. However, most tumors do not attenuate after C1 laminectomy alone; hence, we think that tumor resection by the transdural approach is one effective method to perform enucleation of the tumor after C1 laminectomy.
Similar content being viewed by others
Introduction
Although retro-odontoid pseudotumoral lesions that compress the cervicomedullary junction are relatively common in patients who have rheumatoid arthritis with atlantoaxial instability, they rarely occur in those with noninflammatory retro-odontoid lesions without atlantoaxial instability. We report here a case of a retro-odontoid pseudotumor causing cervical myelopathy without atlantoaxial instability, and review the relevant literature.
Several authors have reported these retro-odontoid pseudotumoral lesions as synovial cysts, herniated discs, ganglion cysts, damaged transverse ligaments, degenerated transverse ligaments or pseudogout.1–7 Some authors reported surgical treatment using the transoral approach for direct decompression of the spinal cord.8–10 However, because this lesion is benign, indirect decompression of the spinal cord is usually performed via a posterior approach. We report here a patient with a retro-odontoid pseudotumor causing cervical myelopathy. The pseudotumor was surgically removed via a transdural approach.
Case report
An 83-year-old man presented with a 2-month history of vague numbness, pain and motor weakness in the upper and lower extremities. Fine movement disturbance was observed in his daily life. Neurological examination revealed abnormal reflexes, including pathological plantar reflex. A manual muscle test (MMT) showed MMT grade 3 in both the upper and lower extremities, but there was no sensory loss. The patient complained of urinary retention and fecal incontinence. The Japanese Orthopaedic Association (JOA) score for cervical myelopathy was 5 out of a maximum of 17 points.
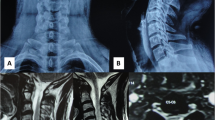
Plain radiography showed moderate osteoarthritis at the C1/2 joint with sclerotic change in the odontoid process. Dynamic radiography did not reveal any instability at the C1/2 level (Figures 1a and b). The atlas-dens interval was 2.5 mm in cervical flexion. Magnetic resonance imaging (MRI) demonstrated a retro-odontoid mass severely compressing the spinal cord. The mass had isointensity on T1-weighted MRI, and mixed isointensity and high intensity on T2-weighted MRI (Figures 1c and d). Peripheral enhancement of the mass was observed on T1-weighted MRI with gadolinium (Figure 1e). A high-intensity area within the spinal cord was observed on T2-weighted MRI (Figure 1c).
Preoperative imaging of the cervical spine. Dynamic radiography in (a) flexion, and (b) distraction. Radiography showed osteoarthritis at the C1/2 joint with sclerotic change in the odontoid process. Dynamic radiography revealed no instability at the C1/2 level. MRI: (c) sagittal view of T2-weighted image, (d) sagittal view of T1-weighted image, (e) sagittal view of T1-weighted image with gadolinium enhancement. Note that there was peripheral enhancement of the mass (e) and edematous changes in the spinal cord (c).
C1 laminectomy was performed, followed by a posterolateral transdural approach to the mass. After opening the dura, the spinal cord was gently reflected with the denticulate ligament. The vertebral artery was protected using a gauze containing phosphate-buffered saline. After a straight incision was made in the anterior part of the dura, the content of the mass was resected. The mass was yellowish, with some parts being soft mucous tissue (Figure 2a). Vascular development was poor, and no granular tissue was observed. The mass was partially removed and the spinal cord replaced anteriorly. Decompression of the spinal cord was confirmed with postoperative MRI (Figure 3).
Laminectomy of C1 was performed, followed by a posterolateral transdural approach to the mass. (a) Photograph and representative diagram of the pseudotumor before removal. The specimen consisted of many small pieces of yellowish white and partially myxoid soft tissue. (b) A microscopic view of a section of the pseudotumor stained with hematoxylin and eosin showing fibrinoid, degenerated material or collagenous tissue with myxoid changes. (c) Cartilaginous metaplasia and fibrinoid degeneration were also seen. There was some inflammatory cell infiltration, but no granulation or granulomatous lesion. No amyloidosis was observed with Congo red staining. There was no evidence of malignancy or neoplasm.
Microscopic examination revealed that the mass contained collagenous tissue with myxoid changes (Figure 2b), cartilaginous metaplasia (Figure 2c) and fibrinoid degeneration. There was partial infiltration with inflammatory cells, but no granulation or granulomatous lesion. Degenerated ligamentous tissue was also observed (Figures 2b and c). The resected material contained tendon-like, dense, collagenous tissue with fibrinous deposits but no inflammatory cell infiltrates or calcification. Congo red staining revealed no amyloidosis.
Postoperatively, the patient recovered from his urinary retention and fecal incontinence. At discharge, the patient was ambulant without a cane. It is now 7 years after surgery, and there has been no recurrence of the retro-odontoid pseudotumor and no instability of the cervical spine. The patient is now 90 years old, and has an improved JOA score of 11.5 points.
Discussion
Periodontoid synovial cysts, or pseudotumors, are rare lesions that cause symptomatic cervicomedullary compression. The etiology of this condition has not yet been clarified. Some authors have reported that these cysts are composed of inflammatory granulation tissue that grows from the synovial tissue between the dens and the posterior articular facet of the posterior arch of C1, or between the dens and the transversal ligament.3 Others have reported that reactive fibrous tissue secondary to mechanical stress causes these periodontoid synovial cysts.5
Conservative treatment with an external cervical brace along with systemic therapy with nonsteroidal anti-inflammatory drugs and steroids is reportedly effective.11 Because the laboratory data did not indicate inflammation, we preoperatively excluded inflammatory diseases such as rheumatoid arthritis or infection. Our pathological findings revealed a degenerative condition with no reactive changes such as inflammation; this suggests that anti-inflammatory drugs could not have decreased the size of this lesion. We therefore conclude that surgical intervention is an alternative treatment for patients with myelopathy.
Several surgical procedures for these patients have been described, including atlantoaxial fusion, C1 laminectomy, C1 laminoplasty, direct transdural tumor resection and fusion. A transoral removal subsequent to posterior fusion has historically been the most common treatment.8–10 By contrast, some surgeons have used a posterior approach to avoid the morbidity of a transoral approach.12–15 It has been reported that C1/C2 or C0/C3 fixation techniques can guarantee the same results for reduction or regression of retro-odontoid pseudotumors and spinal cord decompression under both inflammatory and degenerative conditions.12 Kakutani et al.13 reported that C1 laminectomy without fusion resulted in spontaneous regression of pseudotumors and alleviation of the neurological deficit in all patients. However, spontaneous mass regression is reported after posterior fusion even in the absence of radiographical atlantoaxial instability.14 With atlantoaxial instability, occipitocervical fusion reduces myelopathy, but a subaxial lesion may occur in highly active patients who live long lives after the surgery.16
C1 laminectomy can cause the disappearance of a pseudotumor diagnosed by enhanced MRI within 1 year postoperatively. The improved blood flow in the neovascularized area caused by C1 laminectomy may contribute to regression of the retro-odontoid pseudotumor, similarly to the disappearance of herniated nucleus pulposus.13 However, in the present case the pseudotumor had poor neovascularization. Thus, it is possible that another mechanism promotes the pseudotumor disappearance. Ohnishi et al.17 reported a different appearance and pathological finding of a pseudotumor to the one in the present case. Byun et al.18 reported cervical spine chondroma. It is possible that the mass in our case was a chondroma with degenerative changes, because of the presence of cartilaginous metaplasia.
We used a transdural approach in the present case and have observed no recurrence for 7 years postoperatively. Takemoto et al.15 reported that C1 laminectomy is beneficial, especially for elderly patients, given the risk of other surgical options using an anterior transoral approach or posterior fusion. However, most tumors do not attenuate after C1 laminectomy alone;13 hence, we think that tumor resection by the transdural approach is one effective method to perform enucleation of the tumor after C1 laminectomy.
References
Cai CY, Palmer CA, Paramore CG . Exuberant transverse ligament degeneration causing high cervical myelopathy. J Spinal Disord 2001; 14: 84–88.
Chen TY, Lui TN . Retrodental fibrocartilaginous mass. Report of a case. Spine 1997; 22: 920–923.
Crockard HA, Sett P, Geddes JF, Stevens JM, Kendall BE, Pringle JA . Damaged ligaments at the craniocervical junction presenting as an extradural tumour: a differential diagnosis in the elderly. J Neurol Neurosurg Psychiatry 1991; 54: 817–821.
Miller JD, al-Mefty O, Middleton TH 3rd . Synovial cyst at the craniovertebral junction. Surg Neurol 1989; 31: 239–242.
Sze G, Brant-Zawadzki MN, Wilson CR, Norman D, Newton TH . Pseudotumor of the craniovertebral junction associated with chronic subluxation: MR imaging studies. Radiology 1986; 161: 391–394.
Tabaddor K, Sachs D, Llena JF, Testaiuti MA . Ganglion cyst of the odontoid process. Case report and review of the literature. Spine 1996; 21: 2019–2022.
Griesdale DE Jr, Boyd M, Sahjpaul RL . Pseudogout of the transverse atlantal ligament: an unusual cause of cervical myelopathy. Can J Neurol Sci 2004; 31: 273–275.
Birch BD, Khandji AG, McCormick PC . Atlantoaxial degenerative articular cysts. J Neurosurg 1996; 85: 810–816.
Van Gompel JJ, Morris JM, Kasperbauer JL, Graner DE, Krauss WE . Cystic deterioration of the C1-2 articulation: clinical implications and treatment outcomes. J Neurosurg Spine 2011; 14: 437–443.
Kerschbaumer F, Kandziora F, Klein C, Mittlmeier T, Starker M . Transoral decompression, anterior plate fixation, and posterior wire fusion for irreducible atlantoaxial kyphosis in rheumatoid arthritis. Spine 2000; 25: 2708–2715.
Cecchi PC, Peltz MT, Rizzo P, Musumeci A, Pinna G, Schwarz A . Conservative treatment of an atlantoaxial degenerative articular cyst: case report. Spine J 2008; 8: 687–690.
Barbagallo GM, Certo F, Visocchi M, Palmucci S, Sciacca G, Albanese V . Disappearance of degenerative, non-inflammatory, retro-odontoid pseudotumor following posterior C1-C2 fixation: case series and review of the literature. Eur Spine J 2013; 22 (Suppl 6): S879–S888.
Kakutani K, Doita M, Yoshikawa M, Okamoto K, Maeno K, Yurube T et al. C1 laminectomy for retro-odontoid pseudotumor without atlantoaxial subluxation: review of seven consecutive cases. Eur Spine J 2013; 22: 1119–1126.
Chikuda H, Seichi A, Takeshita K, Shoda N, Ono T, Matsudaira K et al. Radiographic analysis of the cervical spine in patients with retro-odontoid pseudotumors. Spine 2009; 34: E110–E114.
Takemoto M, Neo M, Fujibayashi S, Sakamoto T, Ota M, Otsuki B et al. Clinical and radiographic outcomes of C-1 laminectomy without fusion in patients with cervical myelopathy that is associated with a retro-odontoid pseudotumor. Clin Spine Surg (e-pub ahead of print 18 May 2016; doi:10.1097/BSD.0b013e31829eb7e6).
Matsunaga S, Sakou T, Onishi T, Hayashi K, Taketomi E, Sunahara N et al. Prognosis of patients with upper cervical lesions caused by rheumatoid arthritis: comparison of occipitocervical fusion between c1 laminectomy and nonsurgical management. Spine 2003; 28: 1581–1587.
Ohnishi Y, Iwatsuki K, Taketsuna S, Ninomiya K, Yoshimine T . Retro-odontoid synovial cyst resected via an anterolateral approach without fusion. Eur Spine J 2015; 24 (Suppl 4): S508–S513.
Byun YH, Sohn S, Park SH, Chung CK . Cervical spine chondroma compressing spinal cord: a case report and literature review. Korean J Spine 2015; 12: 275–278.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Tominaga, H., Setoguchi, T., Nagano, S. et al. Retro-odontoid mass without atlantoaxial instability causing cervical myelopathy: a case report of transdural surgical resection. Spinal Cord Ser Cases 2, 16025 (2016). https://doi.org/10.1038/scsandc.2016.25
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/scsandc.2016.25