Abstract
Study design:
Single case report.
Objectives:
To present a case of lumbar disc herniation causing compression of a tethered cord that was successfully treated with lumbar decompression and fusion.
Background:
A tethered cord is a rare pathology associated with a congenital spinal malformation, spinal dysraphism. Furthermore, myelopathy due to lumbar disc herniation in the presence of a tethered cord is extremely rare.
Methods:
Single case report.
Results:
A 43-year-old male with a history of spina bifida presented to our clinic for an evaluation of a progressive spastic gait disturbance and numbness in the lower limbs. A neurological examination revealed muscle weakness and pyramidal tract signs in the lower limbs. Magnetic resonance imaging of the lumbar spine showed disc herniation at L2–3 causing compression of a low-lying cord. Surgical intervention, including herniotomy via a posterolateral approach and instrumented posterolateral fusion, was performed, and a good outcome was achieved 1 year after the surgery.
Conclusion:
The potential for lumbar disc herniation in the presence of a tethered cord should be taken into account in the differential diagnosis of spinal pathologies causing spastic gait disturbances. Furthermore, posterior decompression and fusion is a useful treatment option in such cases.
Similar content being viewed by others
Introduction
The spinal cord is usually present within the spinal canal from the craniocervical to upper lumbar level, with cauda equina being observed at the distal level to the end of the spinal cord. However, a so-called tethered or low-lying cord is sometimes observed in association with embryological errors in the development of the neural axis. This symptomatic entity is known as tethered cord syndrome (TCS).
We herein present a case of myelopathy due to lumbar disc herniation in the presence of a tethered cord in which a good neurological recovery was achieved following surgical intervention for the lesion.
Case Report
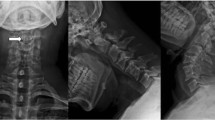
A 43-year-old male presented to our clinic due to gait disturbance and numbness in the lower limbs. The patient’s symptoms had begun spontaneously and gradually deteriorated over 6 months from onset. His past history included surgery for lumbar spina bifida at 0 years of age and ileal conduit surgery for neurologic bladder associated with spinal dysraphism at 13 years of age, after which he received follow-up management at the urological department of our hospital. However, he had no gait disturbance until the onset of the above symptoms. At his first visit, he was unable to walk due to severe spasticity and numbness in the lower limbs. A neurological examination revealed muscle strength in the proximal and distal lower limbs of grade 3-4/5 and 1-3/5, respectively, with a muscle stretch reflex indicating hyperreflexia. Magnetic resonance imaging (MRI) of the lumbar spine was performed, which showed L2–3 disc herniation with intramedullary signal intensity changes on T2 images and a tethered cord (Figure 1). Herniotomy was performed via a posterolateral approach following laminotomy and wide medial facetectomy on the left side and instrumented posterolateral fusion using an autologous bone graft for subligamentous extruded disc herniation at L2–3 (Figure 2). Postoperatively, the patient received physical therapy and his gait disturbance gradually improved. One year after surgery, MRI showed the low-lying cord to be completely decompressed and the patient was able to walk with the slight support of a single cane (Figure 3).
Discussion
A tethered or low-lying cord is part of the spectrum of spinal dysraphism. In this type of congenital malformation, the spinal cord remains attached to the base of the spinal canal due to errors in the embryonic development of the neural axis. Tethered cords can cause various symptoms, including weakness in the lower limbs and urinary disturbances. Although most cases of tethered cords are diagnosed as TCS in childhood, adult-onset TCS is also recognized.1, 2 In the present case, although the patient had a history of surgery for congenital spina bifida and urinary problems associated with dysraphism, he had no apparent lower limb symptoms, including a gait disturbance. The patient exhibited a spastic gait disturbance and hyperreflexia at his first visit. When physical findings consistent with lesions causing spinal cord compression are observed, the potential for low-lying cord compression due to lumbar disc herniation should be taken into account, especially in adults with known spinal dysraphism.
Adult-onset TCS usually occurs due to trauma or degenerative spinal stenosis, when relatively mild traction forces on the spinal cord remain asymptomatic in childhood.3 To our best knowledge, only two cases regarding disc herniation-related myelopathy in patients with a tethered cord have been reported. First, Kramer et al.4 reported a case of thoracic disc herniation in a 54-year-old female with tethered cord syndrome; however, the disc herniation itself was not associated with the onset of tethered cord-related symptoms. Second, Srinivas et al.5 reported a 77-year-old female with known spina bifida occulta who presented with severe low back pain and progressive paraparesis. MRI showed significant disc prolapse at L2–3 causing low-lying cord compression, and surgery involving laminectomy without fusion improved the patient’s symptoms. In the present case, MRI of the lumbar spine demonstrated compression of a low-lying cord due to L2–3 disc herniation, similar to the above report. However, the combined process of herniotomy and laminectomy/laminotomy is considered to be a better surgical procedure than laminectomy alone to achieve an adequate decompression of the spinal cord. Furthermore, the risk of neurological deterioration was evaluated due to retraction of the spinal cord when the herniotomy was performed via the posterior approach without sacrificing the facet joint. We performed a wide medial facetectomy to safely remove the herniated disc, while also performing posterolateral fusion. Consequently, we achieved a good neurological recovery after surgery. Therefore, this surgical procedure, which can be used to treat ventral spinal cord compression and stabilize the affected segment, is a potential treatment option for this rare pathology.
Conclusion
Posterior decompression and fusion was performed for low-lying cord compression due to L2–3 disc herniation, thus resulting in a good outcome. The potential for lumbar disc herniation in the presence of a low-lying cord should be taken into account in the differential diagnosis of adults presenting with spastic gait disturbances.
References
Lapsiwala SB, Iskandar BJ . The tethered cord syndrome in adults with spina bifida occulta. Neurol Res 2004; 26: 735–740.
Yamada S, Lonser RR . Adult tethered cord syndrome. J Spinal Disord 2000; 13: 319–323.
Pang D, Wilberger JE Jr . Tethered cord syndrome in adults. J Neurosurg 1982; 57: 32–47.
Kramer JL, Dvorak M, Curt A . Thoracic disc herniation in a patient with tethered cord and lumbar syringomyelia and diastematomyelia: magnetic resonance imaging and neurophysiological findings. Spine 2009; 34: E484–E487.
Srinivas S, Shetty R, Collins I . Symptomatic lumbar disc protrusion causing progressive myelopathy in a low-lying cord. Global Spine J 2012; 2: 115–118.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Endo, F., Iizuka, H., Iizuka, Y. et al. Myelopathy due to lumbar disc herniation in the presence of a tethered cord. Spinal Cord 52 (Suppl 1), S11–S13 (2014). https://doi.org/10.1038/sc.2014.67
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2014.67