Abstract
Study design:
Diagnostic study.
Objectives:
The objective of this study was to compare patterns of electromyography (EMG) recordings of abdominal muscle function in persons with motor-complete spinal cord injury (SCI) above T6 and in able-bodied controls, and to determine whether manual examination or ultrasound measures of muscle activation can be accurate alternatives to EMG.
Setting:
Research center focused on SCI and University laboratory, Vancouver, Canada.
Methods:
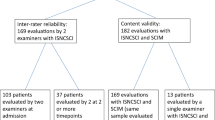
Thirteen people with SCI (11 with American Spinal Injury Association Impairment Scale (AIS) A and 2 AIS B; C4-T5), and 13 matched able-bodied participants volunteered for the study. Participants completed trunk tasks during manual examination of the abdominal muscles and then performed maximal voluntary isometric contractions, while EMG activity and muscle thickness changes were recorded. The frequency of muscle responses detected by manual examination and ultrasound were compared with detection by EMG (sensitivity and specificity).
Results:
All individuals with SCI were able to elicit EMG activity above resting levels in at least one abdominal muscle during one task. In general, the activation pattern was task specific, confirming voluntary control of the muscles. Ultrasound, when compared with EMG, showed low sensitivity but was highly specific in its ability to detect preserved abdominal muscle function in persons with SCI. Conversely, manual examination was more sensitive than ultrasound but showed lower specificity.
Conclusion:
The results from this study confirm preserved voluntary abdominal muscle function in individuals classified with motor-complete SCI above T6 and highlight the need for further research in developing more accurate clinical measures to diagnose the level of trunk muscle preservation in individuals with SCI.
Similar content being viewed by others
Introduction
Currently, there are no established clinical methods for examining motor function in the abdominal muscles following a spinal cord injury (SCI).1 As a result, the International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI) relies solely on sensory tests to determine the level and completeness of the lesion in the thoracic spinal segments,1 making conclusions about the motor level and function of abdominal muscles uncertain. This has been demonstrated by recent electromyographic (EMG) recordings of preserved abdominal muscle activity in persons that were clinically classified with a complete high thoracic SCI. For example, Bjerkefors et al.2 used indwelling fine-wire EMG to record preserved abdominal muscle activity during voluntary contractions in a person with a motor-complete SCI at the T3 level. Likewise, Bjerkefors et al.3 detected preserved voluntary abdominal muscle activity using surface EMG in individuals with motor-complete SCI above T6, and confirmed that this activity was a result of corticospinal preservation by using transcranial magnetic stimulation. Therefore, within a limited sample, there is evidence that EMG may provide a sensitive, accurate technique to detect preserved motor function in the abdominal muscles of individuals with SCI. However, questions remain about whether similar findings can be extended to a larger sample of persons with SCI clinically classified with motor-complete SCI above T6 and whether abdominal muscle function may be detected using less-specialized equipment than EMG. Within a clinical setting, manual examination and ultrasound measurement could be accessible methods to identify preserved abdominal muscle function. Once those pathways have been identified, clinicians can prescribe targeted rehabilitation exercises for those muscles to improve function.4 In the legs, identifying even small amounts of preserved function to these muscles has the potential to allow for greater improvements in function.5, 6, 7
Although manual examination of abdominal musculature is not currently used within the ISNCSCI, it has been incorporated into classification of trunk function for paralympic athletes such as in wheelchair rugby8 and Nordic skiing.9 During this classification procedure, athletes are asked to perform different trunk function tasks while the classifier observes the performance and/or palpates the appropriate trunk muscles. The reason for using different trunk tasks is that they each involve unique combinations of abdominal muscle activity to move the trunk into a new orientation or stabilize the spine.10, 11 As individual abdominal muscles receive innervation from different thoracic segment levels,12 the assessment of different abdominal muscles should help to further increase the diagnostic accuracy in identifying the specific level and completeness of the SCI. However, to our knowledge, no studies have examined the accuracy of using manual examination to determine abdominal muscle function in persons with SCI.
Ultrasound provides another non-invasive option for assessing abdominal muscle activity.13, 14 Changes in muscle thickness measured from ultrasound recordings are highly correlated with changes in muscle activation recorded using surface and indwelling EMG.15, 16, 17 Ultrasound has another advantage over surface EMG and manual examination, in that it can distinguish muscle activity from multiple layers of overlapping deep and superficial abdominal muscles.15, 16 Although ultrasound measures of muscle thickness have been established as a reliable indicator of muscle activity in patients with low back pain,15 there is no evidence to date that it can be an effective surrogate for EMG recordings to detect the low levels of activity that are likely to be present in persons with partial preservation of abdominal muscle function following SCI.
Therefore, the purpose of this study is to (a) compare patterns of EMG recording of abdominal muscle function in persons with motor-complete SCI above T6 and in able-bodied controls; (b) to compare the sensitivity and specificity of manual examination or ultrasound measures of muscle thickness against surface EMG for detecting preserved abdominal muscle function in persons with SCI; and (c) to evaluate the intra-rater reliability of ultrasound measures of abdominal muscle activity in both persons with SCI and in able-bodied controls.
Materials and methods
Participants
Thirteen individuals (five females, 37±8 years, 71.6±14.1 kg, 1.77±0.1 m) with chronic motor-complete SCI, rated by the American Spinal Injury Association Impairment Scale (AIS) as either, no sensory or motor function preserved in the sacral segments S4–S5 (AIS A), or sensory but not motor function preserved below the neurological level and includes the sacral segments S4–S5 (AIS B)1 volunteered for the study. To be included in the study, participants must have had an SCI above the T6 level suffered at least 1-year prior. A detailed description off all SCI participants is presented in Table 1. In addition, 13 able-bodied, matched controls volunteered for the study (five females; 35±9 years, 77.6±14.7 kg, 1.78±0.1 m). All participants received oral and written information describing the study, and signed written consent to voluntarily participate. The study was approved by the University of British Columbia Clinical Research Ethics Board and the Vancouver Coastal Health Research Institute.
Experimental design and procedure
Clinical classification and trunk muscle assessment (day 1)
The neurological lesion level, completeness of the injury and zone of partial preservation of the SCI were assessed by an experienced physician/PhD according to the ISNCSCI1 to verify the participant’s reported AIS level.
Participants lay supine on a plinth and were instructed to perform four different trunk muscle tasks: trunk flexion, trunk rotation to the left and right, and the hollowing maneuver. They were asked to attempt to bring their fingertips to their knees (trunk flexion) or to their contralateral knee (trunk rotation) or to draw their navel into the spine (hollowing). During the task, the clinician palpated the key abdominal muscles (transversus abdominis (TrA), obliquus internus (OI), obliquus externus (OE) and rectus abdominis (RA)), and detectable muscle activity was classified as present or absent. The tasks were chosen to selectively activate different abdominal muscles, and in some case the asymmetrical activation of muscle pairs. Comparing the task-specific pattern of activity in muscles from able-bodied controls and individuals with SCI helps determine whether the muscle responses are voluntary and not simply global activity that could be attributed to changes in intra-abdominal pressure, spasticity or stretch reflexes.
Voluntary activation of abdominal muscles (days 2 and 3)
The following protocol was repeated on two separate days. Participants were instructed to perform seven different trunk muscle tasks: trunk flexion, trunk rotation to the left and right, trunk lateral flexion to the left and right, hollowing maneuver and Valsalva maneuver. Participants lay supine on a plinth with their arms crossed over their chest. Their trunk was secured with a strap placed over the chest to minimize movements of the upper body. Participants’ breathing pattern was matched to a metronome (60 beats per minute) and the contraction was performed during normal exhalation. The following instruction was given: breathe out (2 s), breathe in (2 s), breathe out (2 s) and maximally contract your abdominal muscles (2 s). Participants performed two trials of each task, for four blocks, with a 30-s rest between trials. Two-minute breaks were given between tasks and blocks.
Muscle activity was recorded with surface EMG bilaterally from TrA/OI, OE and RA. Before placing the electrodes, the skin was cleaned with alcohol and, if needed, shaved. Pairs of electrodes (10 mm diameter, Kendall, Tyco Healthcare Group LP, Mansfield, MA, USA) were attached with ~2-cm inter-electrode separation. EMG data were collected at 1500 Hz (Telemyo 2400R, Noraxon, Scottsdale, AZ, USA), amplified (500 times), band-pass filtered between 10 and 500 Hz, A/D converted (Power 1401, CED, Cambridge, UK) and digitally sampled at 1000 Hz, before processing offline (Spike2, CED).
Ultrasound recordings were made using a broadband linear array ultrasound transducer probe (L38e, SonoSite, Inc., Bothell, WA, USA) that was placed bilaterally over two different sites, including (a) transversely across the abdominal wall below the ribcage in vertical alignment with the anterior superior iliac spine (ASIS) for TrA, OI and OE, and (b) 2–3 cm lateral to the umbilicus for RA (Figure 1). A 6-s video clip was recorded (Micromaxx, SonoSite, Inc.) from the first inhalation to the end of each maximal isometric contraction. The same assessor obtained all recordings and was blinded to the results of the first day.
Electrode positions were as follows: obliquus internus (OI)/transversus abdominis (TrA): ~2 cm medial to the anterior superior iliac spine (ASIS; black circles); obliquus externus (OE): ~2 cm below the lowest point of the ribcage (white circles); and rectus abdominis (RA): ~3 cm lateral and 2 cm caudal to the umbilicus (gray circles). The ultrasound transducer was placed transversely across the abdominal wall below the ribcage in vertical alignment with the ASIS for TrA, OI and OE (dark gray rectangles). For RA, the transducer was placed 2–3 cm laterally to the umbilicus (hatched rectangles).
Data analysis
EMG and ultrasound data were analyzed by an experimenter who was blind to the results of the manual muscle examination. EMG data recorded during voluntary tasks was high-pass filtered at 30 Hz and root mean square amplitude was calculated over a 500-ms time period for each muscle, and task during rest and voluntary contraction. The resting muscle thickness was measured from the first frame of the 6-s video clip and the contracting muscle thickness at the 5-s frame. The muscle thickness was measured offline and taken as the average of three measurements (Figure 2).14, 15 For both EMG and ultrasound data, if the average root mean square amplitude or muscle thickness of the two contraction trials for a given muscle and task exceeded 2 s.d. above the mean resting value (calculated from all trials), the value was defined as ‘present’ for the given technique and was included in the frequency analysis.18, 19, 20 For each task, only the appropriate muscles were included to determine presence of response (flexion: bilateral RA; rotation: ipsilateral TrA/OI and contralateral OE; lateral bending: ipsilateral OE; hollowing: bilateral TrA/OI and Valsalva: all muscles).
Ultrasound images from obliquus externus (OE), obliquus internus (OI) and transversus abdominis (TrA) in one subject with SCI. The distance of the muscle thickness was measured offline and made at the middle part of each muscle, between the top of inferior fascial layer and bottom of superior fascial layer, that is, perpendicular to the fascia. The average of three measurements: the middle of the muscle and 1 cm on either side was used in the statistics.
Statistics
To estimate the intra-rater reliability, intraclass correlation (ICC2,1) were calculated between days 2 and 3 for ultrasound measurements during rest. For each muscle, a two-way between- and within-subject analysis of variance was performed with the factors; group (SCI and control) and side (right and left). The frequency of muscle responses detected by ultrasound and manual examination were compared with detection by EMG (treated as the gold standard) to calculate measures of sensitivity, specificity, overall agreement, as well as positive and negative likelihood ratios. In addition, 95% confidence intervals (CIs) are reported. Sensitivity was calculated as the number of true positives divided by the sum of true positives plus false negatives, multiplied by 100. Specificity was calculated as the number of true negatives divided by the sum of false positives plus true negatives, multiplied by 100. Overall percent agreement was calculated as the sum of true positives plus true negatives divided by the total number of cases, multiplied by 100.
Results
Electromyography
All participants completed the protocol with no adverse effects. All participants with SCI were able to produce EMG activity above resting level (2 s.d. above mean resting root mean square amplitude) in at least one abdominal muscle, in one task. EMG activity in individuals with an SCI was detected in the primary mover or orienting muscles for the task and direction (Figure 3), during flexion (number of participants=9), rotation (n=12), lateral bending (n=12), hollowing (n=9) and Valsalva (n=12). Control participants were able to elicit EMG activity above resting levels in the appropriate muscles for a given task in 99% of cases.
Representative participant EMG activity during voluntary maximal (or attempted) trunk movements for the SCI group (upper panel) and control group (lower panel). The top trace in each task represents left-sided activity and the bottom (inverted) trace represents right-sided activity. The primary muscle activation expected for each task (that is, bilateral for flexion and unilateral for lateral bending) is highlighted with black lines. Please note the similarities in task-specific activation patterns demonstrated by both the SCI and control participants.
Ultrasound
The average ICC for the muscle thickness test–retest was 0.793 (95% CI: 0.711–0.875) in the SCI group and 0.957 (95% CI: 0.948–0.966) in the control group. Resting muscle thickness was significantly reduced in all muscles (range 49–58%) in the SCI group compared with the control group (Figure 4; TrA: F=23.42, P=0.0004; OI: F=25.00, P=0.0003; OE: F=21.74, P=0.0005; RA: F=21.43, P=0.0006). No significant differences were seen between sides in any of the abdominal muscles.
Muscle thickness (means and s.d.’s) from ultrasound measurements from transversus abdominis (TrA), obliquus internus (OI), obliquus externus (OE) and rectus abdominis (RA) in the SCI group (black bars) and from the control group (white bars). The ultrasound values are means of left- and right-sided measurements when subjects were resting in supine. *P<0.001.
Muscle thickness changes in individuals with an SCI were detected in the appropriate muscles during rotation (number of participants=5), lateral bending (n=2), hollowing (n=3) and Valsalva (n=2). No appropriate muscle responses were detected during trunk flexion. For the control group frequencies were as follows: flexion (n=12), rotation (n=13), lateral bending (n=13), hollowing (n=6) and Valsalva (n=12).
Manual examination
The abdominal muscles of persons with SCI were detected using palpation during trunk flexion (number of participants=5), trunk rotation (left, n=7; right, n=7) and hollowing maneuver (n=8).
Specificity and sensitivity
As shown in Table 2, ultrasound was found to be highly specific, showing few false positives, but had a poor sensitivity in all tasks. Conversely, manual examination was less specific than ultrasound, but was more sensitive (Table 3). Both methods had similar overall agreement and likelihood ratios with EMG.
Discussion
Although participants with an SCI had injuries classified as motor-complete and above T6, every participant showed measurable abdominal muscle activation with EMG in at least one muscle during one task. Despite the ambiguous definition of ‘motor-complete’ (that is, no sacral sparing at S4/S5), this activity is surprising as none of the participants had any detectable muscle function upon clinical examination below the level of injury and had only minimal sensory preservation (1–2 levels below the clinically defined level). This is consistent with previous work showing EMG recordings of abdominal muscle activity in patients clinically classified as motor-complete above T6.2, 3, 21 Using different movements, we have been able to observe asymmetries in muscle activation patterns, creating a stronger argument that this activation is task specific, confirming voluntary control of the muscles. However, the EMG analysis can potentially be improved by considering indwelling electrodes to make conclusion about the involvement of each of the deep abdominal muscles (TrA and OI) and minimize artifacts related to surface EMG recording, which might lead to more diagnostic utility.
Furthermore, we have ruled out increases in intra-abdominal pressure as a main factor in this activation as all tasks were performed during exhalation, with an open glottis. Although these results provide a more comprehensive analysis of abdominal function in a larger sample of persons that have been clinically classified as having motor-complete SCI above T6, the mechanism of this activation is still unknown. Previous work demonstrates that persons with these injuries show responses to transcranial magnetic stimulation with similar latencies and patterns as able-bodied controls.3 Therefore, this observed muscle activity could potentially be a result of preserved corticospinal pathways. However, whether this is owing to partial preservation of the anterior corticospinal tract, the lateral corticospinal tract or other descending motor pathways is currently unclear.
Although EMG is useful in a laboratory setting, more commonly used techniques in the clinic, for example, real-time ultrasound, are needed to accurately detect abdominal muscle function in patients with SCI. Ultrasound measures of abdominal muscle thickness at rest revealed reduced but not completely atrophied muscles in individuals with an SCI. This observation corroborates prior case study results2 and is consistent with the measure of small, but detectable levels of EMG activity in these muscles. When considering the reliability of ultrasound as a measure of abdominal muscle function, our results with high ICC value of 0.957 in the control group are supported by previous work;15, 22 however, we observed less reliability in the SCI group. This finding may be because of difficulties in identifying fascial borders, as observed in the atrophied muscles of patients with Duchenne’s muscular dystrophy or motor neuron disorders23 and/or mislabelling of fascia borders owing to increased intramuscular fat, causing loss of contrast.24
Compared with EMG, ultrasound measures of voluntary activity were highly specific (no false positive), but had poor sensitivity in detecting muscle activity when present. This imprecision is also reflected by the wide CIs and relatively poor positive and negative likelihood ratios (Table 2). It may be possible that the ultrasound probe used does not have sufficient resolution, or contrast, to determine such small changes in muscle thickness even at the more superficial muscle layers. Therefore, further studies using probes with higher resolutions and contrasts may provide a more sensitive measure.
Manual examination using palpation provided a more sensitive measure for detecting abdominal muscle function compared with ultrasound (Table 3), but was less specific, with some false-positive results. However, similar to ultrasound, relatively poor positive and negative likelihood ratios and wide CIs were observed, reflecting somewhat poor diagnostic accuracy. Increases in sensitivity and specificity may be achieved by implementing a more specific scoring system for the manual examination of abdominal muscle activity during attempted voluntary contractions in SCI and refinements to the optimal testing positions for the patient and clinician, and optimal tasks. Just as the ISNCSCI has been updated over the years to be more specific in arm and leg positions during motor scoring,1 a more standardized approach in determining trunk muscle function via palpation may be possible.
These results highlight the need to include an assessment of trunk musculature in the current ISNCSCI; relying solely on the sensory level does not provide adequate information of abdominal motor function. Although ultrasound currently has its limitations, further investigation is warranted, as it is a highly accessible technique in a clinical setting. In addition, palpation may provide a good opportunity to keep the ISNCSCI methodology consistent if an exam can be further standardized. Although the multisegmental innervation of abdominal musculature may complicate the motor level determination, providing both the patient and clinician more information about the function of abdominal musculature may significantly affect rehabilitation programs and their outcomes.
Data archiving
There were no data to deposit.
References
Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A et al. International standards for neurological classification of spinal cord injury (Revised 2011). J Spinal Cord Med 2011; 34: 535.
Bjerkefors A, Carpenter MG, Cresswell AG, Thorstensson A . Trunk muscle activation in a person with clinically complete thoracic spinal cord injury. J Rehabil Med 2009; 41: 390–392.
Bjerkefors A, Squair JW, Chua R, Lam T, Chen Z, Carpenter MG . Assessment of abdominal muscle function in individuals with motor-complete spinal cord injury above T6 in reponse to transcranial magnetic stimulation. J Rehabil Med 2014 (in press).
Bjerkefors A, Thorstensson A . Effects of kayak ergometer training on motor performance in paraplegics. Int J Sports Med 2006; 27: 824–829.
Behrman AL, Harkema SJ . Locomotor training after human spinal cord injury: a series of case studies. Phys Ther 2000; 80: 688–700.
Manella KJ, Torres J, Field-Fote EC . Restoration of walking function in an individual with chronic complete (AIS A) spinal cord injury. J Rehabil Med 2010; 42: 795–798.
McDonald JW, Becker D, Sadowsky CL, Jane JA Sr, Conturo TE, Schultz LM . Late recovery following spinal cord injury. Case report and review of the literature. J Neurosurg 2002; 97: 252–265.
Altmann VC, Groen BE, van Limbeek J, Vanlandewijck YC, Keijsers NL . Reliability of the revised wheelchair rugby trunk impairment classification system. Spinal Cord 2013; 51: 913–918.
Pernot HF, Lannem AM, Geers RP, Ruijters EF, Bloemendal M, Seelen HA . Validity of the test-table-test for Nordic skiing for classification of paralympic sit-ski sports participants. Spinal Cord 2011; 49: 935–941.
Urquhart DM, Hodges PW, Allen TJ, Story IH . Abdominal muscle recruitment during a range of voluntary exercises. Man Ther 2005; 10: 144–153.
Juker D, McGill S, Kropf P, Steffen T . Quantitative intramuscular myoelectric activity of lumbar portions of psoas and the abdominal wall during a wide variety of tasks. Med Sci Sports Exerc 1998; 30: 301–310.
Hislop H, Avers D, Brown M . Daniels and Worthingham's Muscle Testing. Techniques of Manual Examination and Performance Testing. W.B. Saunders Company. 2013, 34–55.
Rankin G, Stokes M, Newham DJ . Abdominal muscle size and symmetry in normal subjects. Muscle Nerve 2006; 34: 320–326.
Teyhen DS, Gill NW, Whittaker JL, Henry SM, Hides JA, Hodges P . Rehabilitative ultrasound imaging of the abdominal muscles. J Orthop Sports Phys Ther 2007; 37: 450–466.
Ferreira PH, Ferreira ML, Nascimento DP, Pinto RZ, Franco MR, Hodges PW . Discriminative and reliability analyses of ultrasound measurement of abdominal muscles recruitment. Man Ther 2011; 16: 463–469.
Hodges PW, Pengel LH, Herbert RD, Gandevia SC . Measurement of muscle contraction with ultrasound imaging. Muscle Nerve 2003; 27: 682–692.
McMeeken JM, Beith ID, Newham DJ, Milligan P, Critchley DJ . The relationship between EMG and change in thickness of transversus abdominis. Clin Biomech 2004; 19: 337–342.
Musampa NK, Mathieu PA, Levin MF . Relationship between stretch reflex thresholds and voluntary arm muscle activation in patients with spasticity. Exp Brain Res 2007; 181: 579–593.
Bjerkefors A, Carpenter MG, Thorstensson A . Dynamic trunk stability is improved in paraplegics following kayak ergometer training. Scand J Med Sci Sports 2007; 17: 672–679.
Tokuno CD, Carpenter MG, Thorstensson A, Garland SJ, Cresswell AG . Control of the triceps surae during the postural sway of quiet standing. Acta Physiol 2007; 191: 229–236.
Li K, Atkinson D, Boakye M, Tolfo CZ, Aslan S, Green M et al. Quantitative and sensitive assessment of neurophysiological status after human spinal cord injury. J Neurosurg Spine 2012; 17: 77–86.
John EK, Beith ID . Can activity within the external abdominal oblique be measured using real-time ultrasound imaging? Clin Biomech 2007; 22: 972–979.
Pillen S, Arts IM, Zwarts MJ . Muscle ultrasound in neuromuscular disorders. Muscle Nerve 2008; 37: 679–693.
Elder CP, Apple DF, Bickel CS, Meyer RA, Dudley GA . Intramuscular fat and glucose tolerance after spinal cord injury—a cross-sectional study. Spinal Cord 2004; 42: 711–716.
Acknowledgements
We thank the Swedish Centre for Sports Research (CIF), The Swedish Association for Survivors of Accident and Injury (RTP) and the Canadian Institute for Health Research for financial support. The ultrasound system was funded by Natural Sciences and Engineering Research Council of Canada - Research Tools and Instruments (NSERC RTI). Special thanks are due to the participants.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Bjerkefors, A., Squair, J., Malik, R. et al. Diagnostic accuracy of common clinical tests for assessing abdominal muscle function after motor-complete spinal cord injury above T6. Spinal Cord 53, 114–119 (2015). https://doi.org/10.1038/sc.2014.202
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2014.202
This article is cited by
-
Properties of the surface electromyogram following traumatic spinal cord injury: a scoping review
Journal of NeuroEngineering and Rehabilitation (2021)
-
Overground walking with a robotic exoskeleton elicits trunk muscle activity in people with high-thoracic motor-complete spinal cord injury
Journal of NeuroEngineering and Rehabilitation (2018)
-
Overground vs. treadmill-based robotic gait training to improve seated balance in people with motor-complete spinal cord injury: a case report
Journal of NeuroEngineering and Rehabilitation (2017)
-
Response to: Diagnostic accuracy of common clinical tests for assessing abdominal muscle function after motor-complete spinal cord injury above T6
Spinal Cord (2015)
-
Response to ‘Diagnostic accuracy of common clinical tests for assessing abdominal muscle function after motor-complete spinal cord injury above T6’
Spinal Cord (2015)