Abstract
Study design:
Retrospective study.
Objectives:
Most men with spinal cord injury are anejaculatory. Much has been reported about their semen quality collected by penile vibratory stimulation and electroejaculation (EEJ). What is not well-described is the nature of semen quality in SCI patients who can ejaculate by masturbation. This study was performed to understand the degree to which their semen quality differed from that of anejaculatory SCI patients versus that of healthy non-SCI control subjects.
Setting:
University of Miami.
Methods:
Retrospective chart review of Male Fertility Research Program participants from 1991 to 2011.
Results:
Of 528 SCI subjects, 444 met inclusion criteria of completing an algorithm in which ejaculation occurred by masturbation than the PVS group or EEJ group as the PVS group and control group than the PVS group or EEJ group (41%, P<0.001).
Conclusion:
This is the first report focusing on semen quality obtained by masturbation in men with SCI. Sperm motility was higher in men with SCI who could, versus could not, ejaculate by masturbation. Completeness of injury may contribute to this difference.
Similar content being viewed by others
Introduction
Spinal cord injury results most often from traumatic events such as motor vehicle accidents, gunshot wounds, falls and sports-related accidents.1 Young men comprise the majority of new SCI cases.1 Similar statistics are found in countries worldwide.2, 3, 4 Infertility is a sequella of SCI in men.5 The majority of men with SCI are anejaculatory and require penile vibratory stimulation or electroejaculation to retrieve their semen.5 Much has been reported about semen quality obtained by PVS and EEJ;5 however, the features of semen quality obtained by masturbation in men with SCI have not been well-described. Contributing to this lack of information is that few men with SCI can achieve ejaculation via masturbation.
After 20 years of studying semen quality in 528 men with SCI, our research program has accumulated data on 43 men with SCI who could achieve ejaculation via masturbation. The goal of the present study was to characterize semen quality in these men. We further compared the ejaculates of these men to ejaculates of healthy, non-SCI men, as well as to SCI men who could not achieve ejaculation via masturbation.
Materials and methods
Patients
We retrospectively reviewed our database of 528 men with SCI who participated in the Male Fertility Research Program of the Miami Project to Cure Paralysis between 1991 and 2011. All men were in good general health and had no known causes of infertility other than SCI. Men in the control group were non-SCI, healthy men with no history of infertility. All participants signed an informed consent before entry into the study.
Sperm collection
In the control group, semen was collected by masturbation. In the group of men with SCI, semen was collected according to our sperm retrieval algorithm, which has been previously published.6 Each SCI subject was assigned to a group based on his ability to ejaculate. If he could ejaculate by masturbation, he was assigned to the SCI-masturbation group. If he could not ejaculate by masturbation, but could ejaculate by PVS, he was assigned to the PVS group. If he could not ejaculate by masturbation or PVS, but could ejaculate with EEJ, he was assigned to the EEJ group. Each man was assigned to only one group. If a subject was unresponsive to masturbation, PVS and EEJ, he was excluded from further analysis.
Semen analysis
Only antegrade specimens, that is, no retrograde specimens, were analyzed in this study, because of the variability in sperm motility introduced by the bladder contents.7 Antegrade specimens were allowed to liquefy for 20 to 30 minutes at room temperature. Semen volume, sperm concentration and sperm motility were determined according to WHO criteria8 using manual microscopy.
Data collection and statistical analysis
For all men with SCI, demographic information was collected and included level and completeness of injury as assessed by standard methods,9 age, years post injury and cause of injury. The following variables were collected for all SCI and control subjects: antegrade semen volume (cc), sperm concentration (millions of sperm per cc ejaculate), and sperm motility (percent of sperm with forward progression).
Statistical analysis was performed using SPSS 18 for Windows (SPSS Inc., Chicago, IL, USA). For each subject, data from multiple ejaculation trials were averaged. Means were calculated±s.e.m. The Mann–Whitney U-test was used to compare continuous variables including age, years post injury, semen volume, sperm concentration and sperm motility. Chi-square tests were used to analyze nominal data including level of injury and completeness of injury. Statistical significance was considered at P<0.05.
Statement of ethics
We certify that all applicable institutional regulations concerning the ethical use of human volunteers were followed during the course of this research.
Results
Of the 528 men analyzed, 444 men met the inclusion criteria for this study. The 84 men who were excluded from the study were those who did not return for PVS after failing masturbation, or those who did not return for EEJ or did not complete EEJ, after failing masturbation and PVS. Demographic data for SCI subjects are shown in Table 1. There was no significant difference in the mean age or mean years post injury between groups.
The level of injury and completeness of injury were unknown in 1% and 52% of patients, respectively. When comparing patients for whom the level of injury was known, the SCI-masturbation group had significantly more men with cervical injuries than the EEJ group, but was not significantly different from the PVS group. In patients for whom completeness of injury was known, the SCI-masturbation group had significantly more men with incomplete injuries compared with the PVS group and the EEJ group (Table 1). There were no significant differences between the PVS and EEJ groups with respect to completeness of injury. Table 1 shows the total number of ejaculation trials per group. Some patients had a large number of trials because they participated in several research studies performed by our group.
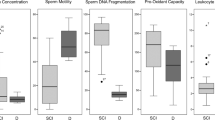
Table 2 shows semen quality in all groups of subjects. In the SCI-masturbation group, the mean±s.e.m. semen volume was significantly higher than that of the EEJ group, and significantly lower than that of the control group. There was no statistically significant difference between the mean semen volume in the SCI-masturbation group and the PVS group.
The SCI-masturbation group had a higher mean sperm concentration than that of the EEJ group. There was no statistically significant difference in mean sperm concentration between the SCI-masturbation group and the PVS group or between the SCI-masturbation group and the control group.
The mean sperm motility was significantly higher in the SCI-masturbation group compared with both the PVS group and EEJ group. The mean sperm motility of the SCI-masturbation group, however, was significantly lower than that of the control group. Similar to previous reports,5 the mean sperm motility was significantly higher in the PVS group compared with the EEJ group.
The SCI-masturbation group had significantly higher mean total motile sperm count than the EEJ group, but significantly lower than the control group. There was no significant difference in mean total motile sperm count between the SCI-masturbation group and the PVS group.
Within the SCI-masturbation group, information regarding erectile dysfunction was collected from 43 men. Twenty-four men retained reflexogenic erection and four had no erections (9%).
Discussion
The majority of men with SCI cannot ejaculate by masturbation and require medical assistance for sperm retrieval. The methods of PVS and EEJ have been the primary methods of sperm retrieval in couples with SCI male partners undergoing assisted conception procedures.10, 11 Previous studies have shown that sperm motility is better when collected by PVS versus EEJ in men with SCI.12, 13 While the exact mechanism is unknown, it has been speculated that ejaculation by PVS is more physiologically normal than ejaculation by EEJ.7
Previous reports indicate that approximately 10% of men with SCI retain the ability to ejaculate by masturbation.14, 15 In line with these reports, our study found that 8.1% retained this ability. The goal of the present study was to characterize semen quality in this subgroup of SCI subjects and compare it with semen quality of SCI subjects who could not ejaculate by masturbation. A secondary aim was to compare semen quality collected by masturbation in SCI subjects to that collected by masturbation in control subjects.
The present study found that men with SCI who were able to ejaculate by masturbation had significantly higher sperm motility than men with SCI who were not able to ejaculate by masturbation. However, semen collected by masturbation in SCI subjects had significantly lower sperm motility than semen collected by masturbation in control subjects.
Our finding of higher sperm motility in the SCI-masturbation group versus the PVS group differs from data we presented in 2000 in which there was no statistically significant difference in sperm motility between these two groups, that is, 29.0% versus 26.0%.7 We attribute this discrepancy to the low number of subjects in the SCI-masturbation group of the previous study.
The findings of the present study raise questions as to why sperm motility was higher in the SCI-masturbation group compared with the PVS group. We hypothesize that the difference may be attributable to neurological differences between the groups, and not to the method of ejaculation itself. These differences in neurological injury may cause differing degrees of dysinnervation to the seminal vesicles and prostate glands, which may result in abnormal constituents to the seminal plasma that are toxic to sperm. In a previous case–control study of 500 men with SCI, completeness of injury was found to be a significant factor influencing semen quality.16 In our study, the SCI-masturbation group had a significantly higher percentage of men with incomplete injuries compared with the PVS group (54%). Incomplete injuries in the SCI-masturbation group were associated with better semen parameters, and therefore may be a significant factor affecting sperm quality in this population.
In a study of six non-SCI healthy men, no significant differences were found in semen quality obtained by masturbation versus PVS, indicating that the method of PVS does not lead to lower sperm motility.17 We performed our own comparison of PVS versus masturbation in the same group of SCI subjects (n=7). Though our results may be limited due to a small sample size, we found no statistically significant difference in sperm motility between the two groups (data not shown), indicating that neurological status, rather than method of ejaculation, contributes to the difference. For example, all patients in this small sub-analysis could ejaculate by masturbation and PVS, while the PVS group of the present study could not ejaculate by masturbation and had significantly fewer men with incomplete injuries compared with the SCI-masturbation group.
It may be of interest to note that we routinely collect retrograde fractions on all SCI subjects at their initial visit. In our 20-year experience, we have found that retrograde fractions are uncommon with masturbation or with PVS, but fairly common with EEJ. When necessary, retrograde fractions can be a useful source of sperm for insemination procedures.10, 11
Our study is limited by a possible selection bias. The extent to which our study is representative of the general population of men with SCI is uncertain. It is possible that our sample size reflects a select group of men with SCI that are healthy and motivated to seek assistance with fertility at a university setting. However, our participants had demographic and clinical characteristics similar to those reported in other studies, and therefore may be representative of the general population of men with SCI. In addition, our study is also limited by the number of men with SCI where completeness of injury was unknown.
This is the first report to focus on semen quality obtained by masturbation in men with SCI. These men had higher sperm motility than men with SCI who could not ejaculate by masturbation, but lower sperm motility than healthy non-SCI control subjects. These differences may be attributable to the neurological completeness of injury. This study contributes significant new information to our understanding of semen quality in this small but important subgroup of SCI patients.
Data archiving
There were no data to deposit.
References
National SCI Statistical Center. Spinal Cord Injury - Facts and Figures at a Glance 2010. https://www.nscisc.uab.edu/public_content/pdf/Facts%20and%20Figures%20at%20a%20Glance%202010.pdf.(2010).
Pirouzmand F . Epidemiological trends of spine and spinal cord injuries in the largest Canadian adult trauma center from 1986 to 2006. J Neurosurg Spine 2010; 12: 131–140.
Chiu WT, Lin HC, Lam C, Chu SF, Chiang YH, Tsai SH . Review paper: epidemiology of traumatic spinal cord injury: comparisons between developed and developing countries. Asia Pac J Public Health 2010; 22: 9–18.
Wyndaele M, Wyndaele JJ . Incidence, prevalence and epidemiology of spinal cord injury: what learns a worldwide literature survey? Spinal Cord 2006; 44: 523–529.
Brackett NL, Lynne CM, Ibrahim E, Ohl DA, Sonksen J . Treatment of infertility in men with spinal cord injury. Nat Rev Urol 2010; 7: 162–172.
Brackett NL, Ibrahim E, Iremashvili V, Aballa TC, Lynne CM . Treatment for ejaculatory dysfunction in men with spinal cord injury: an 18-year single center experience. J Urol 2010; 183: 2304–2308.
Brackett NL, Lynne CM . The method of assisted ejaculation affects the outcome of semen quality studies in men with spinal cord injury: a review. NeuroRehabilitation 2000; 15: 89–100.
World Health Organization Laboratory Manual for the Examination of Human Semen and Sperm-Cervical Mucus Interaction, 4th edn. Cambridge University Press: Cambridge, United Kingdom. 1999.
Marino RJ, Barros T, Biering-Sorensen F, Burns SP, Donovan WH, Graves DE et al International standards for neurological classification of spinal cord injury. J Spinal Cord Med 2003; 26 (Suppl 1): S50–S56.
Kathiresan AS, Ibrahim E, Aballa TC, Attia GR, Lynne CM, Brackett NL . Pregnancy outcomes by intravaginal and intrauterine insemination in 82 couples with male factor infertility due to spinal cord injuries. Fertil Steril 2011; 96: 328–331.
Kathiresan AS, Ibrahim E, Aballa TC, Attia GR, Ory SJ, Hoffman DI et al Comparison of in vitro fertilization/intracytoplasmic sperm injection outcomes in male factor infertility patients with and without spinal cord injuries. Fertil Steril 2011; 96: 562–566.
Brackett NL, Padron OF, Lynne CM . Semen quality of spinal cord injured men is better when obtained by vibratory stimulation versus electroejaculation. J Urol 1997; 157: 151–157.
Ohl DA, Sonksen J, Menge AC, McCabe M, Keller LM . Electroejaculation versus vibratory stimulation in spinal cord injured men: sperm quality and patient preference. J Urol 1997; 157: 2147–2149.
Bors E, Comarr AE . Neurological disturbances of sexual function with special reference to 529 patients with spinal cord injury. Urol Surv 1960; 10: 191–222.
Biering-Sorensen F, Sonksen J . Sexual function in spinal cord lesioned men. Spinal Cord 2001; 39: 455–470.
Iremashvili VV, Brackett NL, Ibrahim E, Aballa TC, Lynne CM . A minority of men with spinal cord injury have normal semen quality--can we learn from them? A case-control study. Urol 2010; 76: 347–351.
Toussaint D, Roth EJ, Chen D, Ling EA, Jeyendran R . Comparison of semen quality obtained by vibratory stimulation and masturbation. Hum Reprod 1993; 8: 1067–1069.
Acknowledgements
This study was funded by The Miami Project to Cure Paralysis, University of Miami Miller School of Medicine, Miami, FL, USA.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Kathiresan, A., Ibrahim, E., Modh, R. et al. Semen quality in ejaculates produced by masturbation in men with spinal cord injury. Spinal Cord 50, 891–894 (2012). https://doi.org/10.1038/sc.2012.71
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2012.71