Abstract
Study design:
Retrospective study at a rehabilitation center.
Objectives:
Patients with spinal cord injury, even if they are wheelchair users, sometimes suffer from fractures of the lower limb bones. As their bones are too weak to have surgery, and because a precise reduction is not required for restoration, such patients are often indicated for conservative treatment. This case series study investigated the use of a hinged, soft-plastic brace as a conservative approach to treating fractures of the lower extremities of patients with spinal cord injury.
Setting:
National Rehabilitation Center, Japan.
Methods:
Fifteen patients (male, n=10; female, n=5; average age, 52.7 years) with 19 fractures of the femur or the tibia who were treated with a newly-developed hinged, soft-plastic brace were studied. All of them used wheelchairs. We analyzed the time taken for fracture union and for wearing orthotics, degree of malalignment, femorotibial angle and side effects.
Results:
The fractures in this series were caused by relatively low-energy impact. The average time taken for fracture union was 80.1 (37–189) days, and the average amount of time spent wearing orthotics was 77.9 (42–197) days. On final X-ray imaging, the average femorotibial angle was 176.9° (s.d. ±8.90), and 15° of misalignment in the sagittal plane occurred in one patient.
Conclusion:
A hinged, soft-plastic brace is a useful option as a conservative approach for treating fractures of the lower extremities in patients with spinal cord injury.
Similar content being viewed by others
Introduction
The bones of the lower limbs of patients with spinal cord injury may become brittle because of paralysis and the absence of weight-bearing.1, 2, 3 Such patients, even if wheelchair users, sometimes fracture the bones of the lower limbs. Several treatment options that are currently available include intramedullary nailing, internal fixation with a locking plate system, external fixation, direct traction, immobilization with rigid cast fixation and functional orthosis.4, 5, 6 Surgery increases the rates of morbidity and complications.7 Those persons with spinal cord injury suffering from such fractures are indicated to receive conservative treatment because they have weak bones that cannot withstand internal fixation, and because a precise reduction is not critical. However, cast fixation onto vulnerable skin is too risky for such patients who also have sensory impairment. Furthermore, limitations on the activities of daily living (ADL) imposed by cast fixation are not acceptable for these patients. Considering these issues, we developed a new type of brace to fix fracture sites.
This case series study investigated the usefulness of our hinged, soft-plastic brace as a conservative approach to treating fractures of the lower extremities of patients with spinal cord injury.
Materials and methods
Subjects
A review of the surgical records between February 2006 and March 2011 at our hospital identified 15 persons with spinal cord injury with 19 fractures of the femur or the tibia who had undergone conservative treatment with our hinged, soft-plastic brace. During that period, we had selected this method for all patients with fracture around the knee joint or fracture of shaft of the tibia or femur. We analyzed 15 persons with spinal cord injury with 19 fractures of the femur or the tibia. All of them used wheelchairs. Most of the fractures were caused by twisting of the thigh or the lower leg during transfers from the wheelchair to locations such as a bed. Table 1 shows the demographics and characteristics of the patients.
Owing to paralysis and the absence of weight-bearing, the mechanical strength of the involved bones was so decreased that displacement of the fracture segments remained minimal as a result of the low-energy impact mechanism. This is an important point to consider for treatment indication.
If considerable swelling had already developed around the fracture site, and the patients lacked sufficient support from family members, they were admitted to our hospital. If family support was available, the patients could remain at home and be treated as outpatients.
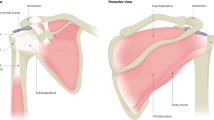
Brace fitting
After preparation of a plaster mold of the involved limb, a knee orthotic was constructed using the mold within a few days. The involved limb was fixed with a splint until the orthotic was available. Depending upon the fracture site, we prepared knee–ankle–foot or pelvis–knee orthotics. Fracture braces mainly comprised two components that covered the thigh and leg with a front opening, and they were connected with a plastic hinge at the knee joint. The site of the side bar attachment was reinforced with soft polyethylene. The brace was made of a soft thermoplastic, co(inter)-polymer of ethylene butyl acetate (Figure 1).
The components could be adjusted with a cuff and Velcro tapes as the swelling around the fracture subsided. Fractures around the knee joint were good indications for this brace. A pelvic component was added to stabilize the proximal thigh segment when treating femoral shaft fractures depending on the situation. An ankle part was also added in a case of tibial shaft fracture.
Brace application
Braces were adjusted to fit to the patient when swelling at the fracture site began to subside (Figure 2). The material was so soft, elastic and transparent that it could allow the patients to monitor their skin condition and to avoid tissue damage.
Inpatient training
The patients followed instructions to manage ADL by themselves, to take off and put on the orthotic, and to transfer between the bed and wheelchair.
Results
The 15 patients (male, n=10; female, n=5; average age, 52.7 years; range, 36–65 years) had 20 fractures. Spinal cord injuries occurred at C5 (n=2), C6 (n=1), C7 (n=2), and the thoracic (n=9) and lumbar (n=1) levels (Table 1). The degree of paralysis was American Spinal Injury Association (ASIA) Impairment Scale (AIS)-A (n=15). The average period between spinal cord injury and lower extremity fracture was 16.6 (s.d.±13.2) years. The fractures in this series were caused by relatively low-energy impact; 14 occurred during transfer (12 fell to the floor and 2 were twisted), three were caused by falls from a wheelchair to the floor, one was caused by twisting in the bath and one was unknown. Four patients were treated at outpatient clinics without admission to hospital. Among 14 femoral fractures, 2 fractures were in the shaft and 11 were in the supracondylar region. Two fractures occurred in the proximal tibia and two in the tibial shaft. Among five patients with bilateral lower limb fractures, only one had fractured both lower limbs at essentially the same time.
Pre- and post-injury ADL did not differ. The patients were able to use their wheelchairs after the brace was applied. They could bend their knees passively and transfer freely. Some patients developed angular deformities at the time visible callus appeared. Such misalignments were managed with appropriate padding at the site of the deformity under the brace.
In the majority of cases, fracture union was satisfactorily achieved. There were no obvious rotational deformities or problematic skin damage due to pressure from the orthotics. The patients could remain seated for a considerable amount of time while wearing the brace. They could transfer from their wheelchairs to other locations and thus prevent ADL decrease. The orthotic components were easy to open, remove and replace for wound care or bathing. Unlike cast fixation, this orthotic could maintain knee mobility, so the patients with refractory-pressure ulcers on the sacrum or ischium could use the wheelchair and did not require bed rest.
The average hospital stay was 130.8 (8–325) days and the average time taken for the bones to unite at the fracture sites was 80.1 (37–189) days (Table 2). The orthotics were worn for an average of 79.8 (42–197) days. On final X-ray imaging, the average femorotibial angle was 176.9° (s.d.±8.90) and 15° of misalignment in the sagittal plane occurred in one patient. Most patients had a spasticity of grade 0–2 of modified Ashworth scale; however, there was no correlation between spasticity and time to union. The fracture failed to unite in one patient (No. 10 in Table 1), but this did not cause pain or a loss of ADL. Patients 2 and 10 required additional treatment with low-intensity pulsed ultrasound.
Discussion
Osteoporosis and an increased frequency of fractures inevitably occur after spinal cord injury.1, 2, 3, 7, 8, 9 We have experience with such patients, who had fractured their lower limbs during low-energy collisions, in a rehabilitation institute for persons disabled due to spinal cord injury.
Several treatment options that are currently available for such patients include intramedullary nailing, internal fixation with a locking plate system, external fixation, direct traction, immobilization with rigid cast fixation and functional orthosis.4, 5, 6 Open reduction and internal fixation with metal plates and screws is usually not indicated, as fractures heal readily in limbs that are paralyzed after spinal cord injury. Surgery increases the rates of morbidity and complications.7 Conventional functional braces with a hard-type plastic shell have been used mainly to treat femoral fractures.5, 10, 11, 12, 13, 14, 15 Such functional braces should allow sufficient strength for weight-bearing. On the contrary, our type of brace cannot provide such high fracture stability. However, rigid fixation was not essential for spinal cord-injury wheelchair users, as such wheelchair users generally do not need to bear weight on their legs, except for certain kinds of transfer, but need to bend their knees in daily situations.7, 16 Braces with a hard plastic shell can result in pressure ulcers and patients often claim that they cannot put them on by themselves. The average period of hospital stay was 18.5 weeks in our study. This was longer than the previous reports on non-spinal cord patients with: traction, average 15.3 weeks (13–22 weeks); cast-brace, average 7.0 weeks (6–9 weeks); and nailing, average 5.4 weeks (3–9 weeks).6 Three patients were initially admitted for treatment of pressure ulcer, and thereafter broke their legs in some transfer during their long hospital stay. That was the reason why overall patients’ average hospitalization was so long in this study, even after fracture union. The average of 11.5 weeks for bony union in our study was also shorter than that reported previously on non-spinal cord patients with: traction, average 16.5 weeks (14–26 weeks); cast-brace, average 15.1 weeks (12–18 weeks); and nailing, average 13.0 weeks (10–22 weeks).6 This is because fractures rapidly heal in individuals with spinal cord injury.7, 17 Our orthotics have several advantages over other methods. The first is that a loss of ADL during the treatment period can be minimized. Second, patients can be treated as outpatients, which is cost-effective. Third, the soft material (with holes) used to make the orthotic does not cause pressure sores or skin damage. Fourth, the bones could unite without losing the prefracture range of motion.
Conclusion
A hinged, soft-plastic brace is a useful conservative option for treating fractures of the lower extremities of patients with spinal cord injury.
Data archiving
There were no data to deposit.
References
Lazo MG, Shirazi P, Sam M, Giobbie-Hurder A, Blacconiere MJ, Muppidi M . Osteoporosis and risk of fracture in men with spinal cord injury. Spinal Cord 2001; 39: 208–214.
Löfvenmark I, Werhagen L, Norrbrink C . Spasticity and bone density after a spinal cord injury. J Rehabil Med 2009; 41: 1080–1084.
Morse LR, Battaglino RA, Stolzmann KL, Hallett LD, Waddimba A, Gagnon D et al Osteoporotic fractures and hospitalization risk in chronic spinal cord injury. Osteoporos Int 2009; 20: 385–392.
Sarmiento A . Fracture bracing. Clin Orthop Relat Res 1974; 102: 152–158.
Baird RA, Kreitenberg A, Eltorai I . External fixation of femoral shaft fractures in spinal cord injury patients. Paraplegia 1986; 24: 183–190.
Thomas TL, Meggitt BF . A comparative study of methods for treating fractures of the distal half of the femur. J Bone Joint Surg Br 1981; 63: 3–6.
Freehafer AA, Mast WA . Lower extremity fractures in patients with spinal-cord injury. J Bone Joint Surg Am 1965; 47: 683–694.
Reiter AL, Volk A, Vollmar J, Fromm B, Gerner HJ . Changes of basic bone turnover parameters in short-term and long-term patients with spinal cord injury. Eur Spine J 2007; 16: 771–776.
Jones LM, Legge M, Goulding A . Intensive exercise may preserve bone mass of the upper limbs in spinal cord injured males but does not retard demineralization of the lower body. Spinal Cord 2002; 40: 230–235.
Mooney V, Nickel VL, Harvey JP, Snelson R . Cast-brace treatment for fractures of the distal part of the femur. A prospective controlled study of one hundred and fifty patients. J Bone Joint Surg Am 1970; 52: 1563–1578.
Connolly JF, Dehne E, Lafollette B . Closed reduction and early cast-brace ambulation in the treatment of femoral fractures. II. Results in one hundred and forty-three fractures. J Bone Joint Surg Am 1973; 55: 1581–1599.
Connolly JF, King P . Closed reduction and early cast-brace ambulation in the treatment of femoral fractures. I. An in vivo quantitative analysis of immobilization in skeletal traction and a cast-brace. J Bone Joint Surg Am 1973; 55: 1559–1580.
Lesin BE, Mooney V, Ashby ME . Cast-bracing for fractures of the femur. A preliminary report of a modified device. J Bone Joint Surg Am 1977; 59: 917–923.
McCollough NC, Vinsant JE, Sarmiento A . Functional fracture-bracing of long-bone fractures of the lower extremity in children. J Bone Joint Surg Am 1978; 60: 314–319.
Roper BA . Functional bracing of femoral fractures. J Bone Joint Surg Br 1981; 63: 1–2.
Freehafer AA, Hazel CM, Becker CL . Lower extremity fractures in patients with spinal cord injury. Paraplegia 1981; 19: 367–372.
Nottage WM . A review of long-bone fractures in patients with spinal cord injuries. Clin Orthop Relat Res 1981; 155: 65–70.
Acknowledgements
We thank all of the orthopedic surgeons, their staff and patients who participated in this study. We also thank Ms Kayoko Nakanishi for her help with the preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Uehara, K., Akai, M., Kubo, T. et al. Soft-plastic brace for lower limb fractures in patients with spinal cord injury. Spinal Cord 51, 327–330 (2013). https://doi.org/10.1038/sc.2012.145
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2012.145
Keywords
This article is cited by
-
Suitability of skin traction combined with braces for treating femoral shaft fractures in 3–5 years old children
Journal of Orthopaedic Surgery and Research (2023)
-
Surgical compared with nonsurgical management of fractures in male veterans with chronic spinal cord injury
Spinal Cord (2015)
-
Soft-plastic brace for lower limb fractures in patients with spinal cord injury
Spinal Cord (2014)
-
Response to Soft-plastic brace for lower limb fractures in patients with spinal cord injury
Spinal Cord (2014)