Abstract
Study design:
Retrospective database review.
Objective:
To compare lengths of stay (LOS), pressure ulcers and readmissions to the acute care hospital of patients admitted to the inpatient rehabilitation facility (IRF) from a model spinal cord injury (SCI) trauma center or from a non-SCI acute hospital.
Background:
Only sparse data exist comparing the status of patients admitted to IRF from a model SCI trauma center or from a non-SCI acute hospital.
Methods:
Acute care, IRF and total LOS were compared between patients transferred to IRF from the SCI center (n=78) and from non-SCI centers (n=131). The percentages of pressure ulcers on admission to IRF and transfer back to acute care were also compared.
Results:
Patients admitted to IRF from the SCI trauma center (SCI TC) had significantly shorter (P=0.01) acute care LOS and total LOS compared with patients admitted from non-SCI TCs. By neurological category, acute-care LOS was less for all groups admitted from the SCI center, but statistically significant only for tetraplegia. There was no significant difference in the incidence of readmissions to acute care from IRF. More patients from non-SCI centers (34%) than SCI centers (12%) had pressure ulcers (P<0.001).
Conclusion:
Acute care in organized SCI TCs before transfer to IRF can significantly lower acute-care LOS or total LOS and incidence of pressure ulcers compared with non-SCI TCs. Patients admitted to IRF from SCI TCs are no more likely to be sent back to an acute hospital than those from non-SCI TCs.
Similar content being viewed by others
Introduction
Spinal cord injury (SCI) is a devastating injury costing the US healthcare system $14.5 billion USD per year in direct medical costs, and disability support along with an additional loss of $5.5 billion on lost productivity.1 SCI is a relatively uncommon, yet devastating, cause of disability with an annual incidence of approximately 12 000 new cases each year.2 Therefore, the need for a coordinated, comprehensive system of care is necessary to meet the unique needs of these individuals. Providing a coordinated, multidisciplinary system of acute care and inpatient rehabilitation for individuals disabled by SCI in one geographic location allows staff to develop expertise in SCI care, and provides patients the opportunity to receive peer support, which may contribute to better outcomes.
In 1970, the Rehabilitation Services Administration of the US Department of Health, Education and Welfare funded the first demonstration project to establish a comprehensive, multidisciplinary model system of SCI care. One of its primary goals was to evaluate the efficiency of such a system.3 Although several studies have demonstrated that patients admitted to model SCI systems soon after injury tend to have better short- and long-term outcomes than patients whose admission to a model system is delayed,4, 5, 6 information on acute care in non-model system facilities has been limited. Therefore, the original mission to evaluate the effectiveness of treatment programs at these nine model SCI systems of care compared with traditional care proved difficult.
Very few studies were found to have attempted this comparison. In 1985, Yarkony et al.7 examined joint contractures on admission to inpatient rehabilitation facility (IRF) after acute care following an SCI in patients admitted in general hospitals versus those who received acute care in their SCI Center. They found that patients treated in general hospitals had a statistically significant increased incidence of joint contractures compared with spinal center patients. Also, patients treated in the spinal center were transferred to IRF sooner post injury. In a subsequent study, Heinemann et al.8 examined the functional outcomes of 185 patients with SCI undergoing rehabilitation who were initially treated in a specialized short-term care unit (center patients) along with 153 patients who were initially treated in general hospitals (non-center patients). Although the groups were comparable in terms of demographic, injury and medical characteristics at the time of IRF admission, the duration from the time of injury to the admission in an IRF was more than twice as long for non-center patients. Although these reports were encouraging, they were completed before the designation of level I trauma centers, and do not compare care provided by a level 1 model SCI system with other level 1 non-SCI trauma centers.
Since 1978, the Regional SCI Center of the Delaware Valley, a partnership between Thomas Jefferson University Hospital (TJUH or, simply, Jefferson) and Magee Rehabilitation Hospital (MRH or, simply, Magee), has provided a coordinated, multidisciplinary system of acute care and rehabilitation for individuals with traumatic SCI. At the Regional SCI Center of the Delaware Valley, one of the most significant changes over the past 5 years has been the decline in the number of admissions within 3 days of injury. As there are five level 1 trauma centers in the greater Philadelphia region, not all patients with acute traumatic SCI are sent to TJUH for acute care. Emergency medical technician routes in Philadelphia for spinal trauma are ordinary without certain predilection for TJUH regarding the severity of injury. However, many of these patients are sent directly to MRH for initial rehabilitation. MRH’s admission policy does not exclude individuals with SCI solely for the presence of pressure ulcers (even grades 3 and 4). Currently only about one-third of the patients with traumatic SCI admitted to MRH come from TJUH. This change in referral pattern has provided us with a unique opportunity to study the differences between those admitted acutely (within 24 h of injury) to a designated model SCI system of care level 1 trauma center and those admitted directly to the IRF from other non-SCI trauma centers in the region.
Therefore, the purpose of this study is to compare lengths of stay (LOS) and medical status of patients admitted to IRF from a model SCI trauma center and those of patients from a non-SCI level 1 trauma center. Medical status included the presence of pressure ulcers on admission to IRF and medical readmissions back to the acute care hospital after initial admission to IRF.
Materials and methods
This study was approved by the institutional review boards at TJUH and MRH. A retrospective database and chart review was performed on 281 individuals with SCI from 2005 to 2007. Patients with incomplete discharge notes from the acute care hospital were excluded, especially if the missing information included data that could influence length of stay (that is, type of injury and complications of treatment). Complete data were obtained on 209 patients. Information collected from the IRF chart included demographic data, date of injury, date of admission to IRF, final discharge from IRF, neurological level and ASIA impairment scale grade at admission, presence of pressure ulcers at admission, and, if transferred back to an acute care hospital, the date and reason for transfer. The policy at MRH during the period of the study was to take color photographs of any pressure ulcers, and include these in the chart. The locations and grades of all pressure ulcers were confirmed by review of these photographs. Pressure ulcers were graded as per National Pressure Ulcer Advisory Panel classification.9
Individuals were stratified by level (tetraplegia/paraplegia) and severity of injury (motor complete/incomplete, ASIA impairment scale A/B versus. ASIA impairment scale C/D). Mean acute care, IRF and total (acute care LOS and IRF LOS) LOS were calculated and compared. Subgroup (level and severity of injury) comparisons were performed only regarding mean acute care LOS. Percentage of pressure ulcers, minor (grades 1 and 2) and major (grades 3 and 4) on admission to IRF, and unplanned medical readmissions back to acute care within 30 days of initial inpatient rehabilitation were compared.
Statistical analysis of data was performed using SAS 9.1 for Windows (Cary, NC, USA). LOS was log-transformed to normalize the distribution and compared using a two-tailed t-test. In addition, a regression model was run to adjust for etiology, sex, neurological category and age. Differences in adjusted LOS were back-transformed to give geometric mean ratios for LOS. The χ2-test was used to compare presence and severity of pressure ulcers at admission to IRF, and the number of readmissions to acute care between the two groups. A significance level of less than 0.05 was set for P-value.
Results
Of the 209 individuals with SCI, 78 patients who were admitted within 24 h of injury to TJUH formed the SCI trauma center (SCI TC) group. The other 131 patients (non-SCI TC group) were admitted directly to the acute IRF SCI Unit at MRH from other non-SCI Level I TCs in the region. The two groups (SCI TC and non-SCI TC) were comparable in regard to race, but differed by sex and etiology of injury (Table 1). The SCI TC had a greater percentage of female patients (P=0.03), more falls and fewer acts of violence (P<0.01) than non-SCI TC. Stratification by level and severity of injury of patients is shown in Table 2. The average age of the 209 patients included in this study was 40.6 years and was slightly greater for the SCI TC group (Table 2).
Patients admitted to IRF from the SCI TC had significantly shorter (P=0.01) acute care LOS (mean 17.2±12.2 days) than patients admitted from a non-SCI TC (mean 35.4±42.3 days) (Table 3). In the regression model, only center and neurological category were significant predictors of acute care LOS; age, sex and etiology were not significant. Etiology was of borderline significance (P<0.10), and so was retained in the final regression model. This difference in acute care LOS was still significant after adjusting for neurological category and etiology. Those admitted to the SCI TC had a 30% reduction in acute care LOS compared with those admitted to a non-SCI TC. By neurological category, acute care LOS was less for all groups admitted from the SCI center, but statistically significant only for tetraplegia: motor complete (22.8 versus 53.5 days, P<0.05) and motor incomplete (13.3 versus 23.0 days, P<0.05).
Regarding IRF LOS (including medical readmits as time within rehabilitation), there was no statistical difference (P>0.05) between patients transferred to IRF from SCI (62.97±40.59) versus non-SCI TCs (67.49±47.08). When acute care LOS and IRF LOS were added to express the total LOS, the patients admitted for acute care in non-SCI TCs had still statistically significantly (P=0.01) longer total LOS (102.92±71.41) than patients from specialized SCI TCs (79.43±48.62).
There was no significant difference in the incidence of readmissions to acute care during the first 30 days of rehabilitation (19 readmissions (24%) of patients originating from the SCI center, 26 readmissions (20%) of patients originating from the non-SCI center). Reasons for transfer back to the acute hospital included fever/infections (n=13), abdominal/GI related (n=8), cardiovascular (n=7), surgical site issues (n=5), respiratory (n=4), bleeding (n=3) and miscellaneous (n=5).
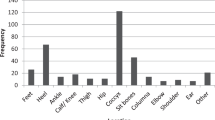
More patients from non-SCI centers (n=44, 34%) than SCI centers (n=24, 12%) had pressure ulcers (χ2 P<0.001) (Figure 1). However, the percentage of patients with grade III and IV pressure ulcers (6% SCI, 11% non-SCI) was not significantly different (P>0.05) (Figure 2).
Discussion
These results suggest that acute care in an organized SCI level I trauma center can significantly reduce acute care and total LOS compared with non-SCI level I trauma centers. Average acute care LOS (log-adjusted) was 30% less in the SCI TC. This was accomplished without an increase in transfers back to acute care for unstable medical conditions. There was also a threefold increase in incidence of pressure ulcers in patients admitted to IRF from non-SCI TCs. Both the presence of pressure ulcers on admission to IRF and medical readmissions back to the acute care hospital after initial admission to IRF were used as indicators of the quality of acute care.
In the model systems, patients receive interdisciplinary care from the time of injury and are provided with lifelong follow-up. Patients are initially treated in acute care units, and may then be transferred to IRF centers in an attempt to decrease the extent of the injury, limit complications and decrease the acute care LOS in the hospital.10 In 2005, the average LOS in acute care was about 15 days, and average LOS in IRF centers was 36 days. Overall, the mean number of days hospitalized (during acute care and rehabilitation) was greater for persons with neurologically complete injuries.10
In the interests of cost reduction and efficiency of care, much effort has been aimed at the reduction of patient LOS in acute care and in IRF.11 Between 1990 and 1997, the average LOS consistently declined; however, the rate of readmission also increased.11 Perhaps there is a limit to the decrease in LOS beyond which the patient outcomes begin to decline. Spine trauma patients are susceptible to a myriad of acute medical complications in rehabilitation, such as spinal and hemodynamic stabilization, abdominal injuries, multiple fractures and brain injury, among others.12 Physicians must determine the optimal LOS in order to minimize susceptibility to these secondary medical complications.
Length of stay in specialized hospital units has declined compared with LOS in general wards of hospitals owing to the more sophisticated care of patients.13 Zhu et al.14 found that the adjusted odds of an LOS more than 7 days were reduced by 30% on a stroke unit compared with general neurology/medical wards. Similarly, the presence of in-house core trauma surgeons and physician assistants improved management and outcome (including reduced LOS) of critically injured trauma patients within a level I TC.13 A systematic review of all available evidence on the timing of surgical fixation for thoracic and lumbar fractures with respect to clinical and neurological outcome showed that early fracture fixation is associated with less complications, shorter hospital and intensive care unit stay, but the effect on neurological outcome remained controversial.15
There is conflicting evidence regarding the timing of surgery of SCI patients, and the related complication rate and LOS. Marshall et al.16 reported in 1987 that postoperative neurological deterioration appeared only in cervical SCI patients who were operated early (5 days or less after injury). This report made some surgeons shy away from early surgery in patients with traumatic SCI. However, subsequent reports did not find excess complications in patients with early surgery. In a prospective randomized trial by Vaccaro et al.17 no significant difference in length of acute postoperative intensive care stay or length of inpatient rehabilitation between the early (<72 h) and late (>72 h) groups was found. Indeed, Duh et al.18 reported in 1994 that those patients operated early on (within the first 24 h) had a lower rate of complications than those undergoing operative intervention at later times. Furthermore, a study by McKinley et al.19 found that SCI patients who underwent late surgery (>72 h after admission) had significantly increased acute care, and total LOS and hospital charges along with higher incidence of pneumonia and atelectasis. However, surgical patients were not stratified further according to injury severity score or other comorbidities precluding early surgery.
LOS may also be influenced by the types of the IRF centers available to the patient. Perhaps the optimal care provided in the model SCI care systems leads to appropriately decreased total length of stay as compared with non-model centers.2, 10
Our results demonstrate that SCI patients with initial admission to SCI TC will have shorter acute care LOS and fewer pressure ulcers. Also, transfers to acute care from IRF are no more likely to occur in patients admitted to IRF from non-SCI acute hospitals than in those admitted from SCI TC. The importance of acute care is further emphasized by the finding that the total LOS was still longer for patients with initial admission to a non-SCI specialized center than to a SCI TC, even though the IRF LOS was comparable for both groups. The latter is expected, as the admission policy to MRH was universal for all patients independent of the origin of their acute care treatment.
Further, our findings confirm that shorter acute care LOS is associated with less severe injury and higher functional status as stated by Eastwood et al.11 The results also reveal that the pressure ulcers were approximately threefold less when a patient is cared in a SCI trauma center. It emphasizes the time, effort and education in daily monitoring of skin aimed at preventing pressure ulcers starting by waiting on a trolley from the emergency room awaiting investigations and clinical work-up, and thus delaying admission to a hospital bed where pressure relieving protocol can begin. Pressure ulcers increase the cost of care, and can delay or prolong rehabilitation due to restrictions in sitting. Acute care readmissions from IRF are dependent mainly on the preadmission medical stability status.20 Providing a coordinated, multidisciplinary system of acute care and rehabilitation for individuals disabled by SCI allows staff to develop expertise in SCI care, and allows patients to begin initial rehabilitation sooner and in better condition.
LOS is frequently viewed as an indicator of the effectiveness of health care delivery.
Even though shorter LOS is a result of effective management, expertise and organization of resources, LOS is dependent on multiple factors including level of injury, medical comorbidities, health care practices, insurance, reimbursement pattern, social, psychological, financial and the discharge destination. Nevertheless, the SCI TCs seem to begin to look into these important rehabilitation aspects right from the day of injury as much as medical and surgical interventions.
Limitations to our study include the differences between SCI patients included in the two groups with regard to sex and type of injury, implying a possible referral to SCI TC of a certain patient population. Also, understanding the limitations of the data, IRF LOS is expressed as total number of days hospitalized (days in IRF plus interim days in acute care hospitals) after initial IRF admission. Subgroup analysis was conducted only for acute care LOS, as our primary hypothesis was regarding the quality of acute care.
Conclusions
Acute care in organized model SCI TCs before transfer to IRF can significantly lower LOS compared with non-SCI TCs. There is approximately threefold increase in incidence of pressure ulcers in patients initially admitted to non-SCI TCs compared with those admitted to a model SCI TC.
References
Berkowitz M, O’leary PK, Kruse DL, Harvey C . Direct costs of spinal injury. In: Berkowitz M (ed.) Spinal Cord Injury: An Analysis of Medical and Social Costs. Demos Medical Publishing: New York, 1998, pp 107.
National Spinal Cord Injury Statistical Center. Spinal Cord Injury: Facts and Figures at a Glance 2009. The University of Alabama: Birmingham, AL, 2009.
Stover SL, DeVivo MJ, Go BK . History, implementation, and current status of the National Spinal Cord Injury Database. Arch Phys Med Rehabil 1999; 80: 1365–1371.
DeVivo MJ, Kartus PL, Stover SL, Fine PR . Benefits of early admission to an organised spinal cord injury care system. Paraplegia 1990; 28: 545–555.
Oakes DD, Wilmot CB, Hall KM, Sherck JP . Benefits of early admission to a comprehensive trauma center for patients with spinal cord injury. Arch Phys Med Rehabil 1990; 71: 637–643.
Donovan WH, Carter RE, Bedbrook GM, Young JS, Griffiths ER . Incidence of medical complications in spinal cord injury: patients in specialised, compared with non-specialised centres. Paraplegia 1984; 22: 282–290.
Yarkony GM, Bass LM, Keenan III V, Meyer Jr PR . Contractures complicating spinal cord injury: incidence and comparison between spinal cord centre and general hospital acute care. Paraplegia 1985; 23: 265–271.
Heinemann AW, Yarkony GM, Roth EJ, Lovell L, Hamilton B, Ginsburg K et al. Functional outcome following spinal cord injury. A comparison of specialized spinal cord injury center vs general hospital short-term care. Arch Neurol 1989; 46: 1098–1102.
National Pressure Ulcer Advisory Panel. Pressure Ulcer Stages Revised by NPUAP. NPUAP: Washington, DC, 2007.
National Spinal Cord Injury Statistical Center. Spinal Cord Injury Facts & Figures at a Glance 2008. University of Alabama: Birmingham, AL, 2008.
Eastwood EA, Hagglund KJ, Ragnarsson KT, Gordon WA, Marino RJ . Medical rehabilitation length of stay and outcomes for persons with traumatic spinal cord injury—1990–1997. Arch Phys Med Rehabil 1999; 80: 1457–1463.
Chen D, Apple Jr DF, Hudson LM, Bode R . Medical complications during acute rehabilitation following spinal cord injury—current experience of the Model Systems. Arch Phys Med Rehabil 1999; 80: 1397–1401.
Mains C, Scarborough K, Bar-Or R, Hawkes A, Huber J, Bourg P et al. Staff commitment to trauma care improves mortality and length of stay at a level I trauma center. J Trauma 2009; 66: 1315–1320.
Zhu HF, Newcommon NN, Cooper ME, Green TL, Seal B, Klein G et al. Impact of a stroke unit on length of hospital stay and in-hospital case fatality. Stroke 2009; 40: 18–23.
Rutges JP, Oner FC, Leenen LP . Timing of thoracic and lumbar fracture fixation in spinal injuries: a systematic review of neurological and clinical outcome. Eur Spine J 2007; 16: 579–587.
Marshall LF, Knowlton S, Garfin SR, Klauber MR, Eisenberg HM, Kopaniky D et al. Deterioration following spinal cord injury. A multicenter study. J Neurosurg 1987; 66: 400–404.
Vaccaro AR, Daugherty RJ, Sheehan TP, Dante SJ, Cotler JM, Balderston RA et al. Neurologic outcome of early versus late surgery for cervical spinal cord injury. Spine (Phila, PA, 1976) 1997; 22: 2609–2613.
Duh MS, Shepard MJ, Wilberger JE, Bracken MB . The effectiveness of surgery on the treatment of acute spinal cord injury and its relation to pharmacological treatment. Neurosurgery 1994; 35: 240–248;discussion 248–249.
McKinley W, Meade MA, Kirshblum S, Barnard B . Outcomes of early surgical management versus late or no surgical intervention after acute spinal cord injury. Arch Phys Med Rehabil 2004; 85: 1818–1825.
Marciniak CM, Heinemann AW, Monga T . Changes in medical stability upon admission to a rehabilitation unit. Arch Phys Med Rehabil 1993; 74: 1157–1160.
Acknowledgements
We acknowledge Benjamin Leiby, PhD for his assistance with the statistical analyses.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Ploumis, A., Kolli, S., Patrick, M. et al. Length of stay and medical stability for spinal cord-injured patients on admission to an inpatient rehabilitation hospital: a comparison between a model SCI trauma center and non-SCI trauma center. Spinal Cord 49, 411–415 (2011). https://doi.org/10.1038/sc.2010.132
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2010.132
Keywords
This article is cited by
-
Epidemiology features of traumatic and non-traumatic spinal cord injury in China, Wuhan
Scientific Reports (2024)
-
Retrospective trends in length of stay and bowel management at discharge from inpatient rehabilitation among individuals with spinal cord injury
Spinal Cord (2022)
-
Outcome after post-acute spinal cord specific rehabilitation: a German single center study
Spinal Cord Series and Cases (2017)
-
The effects of early or direct admission to a specialised spinal injury unit on outcomes after acute traumatic spinal cord injury
Spinal Cord (2017)
-
Epidemiology of traumatic spinal cord injury in Galicia, Spain: trends over a 20-year period
Spinal Cord (2017)