Abstract
Study design:
The study was a retrospective analysis.
Objective:
The objective of the study was to survey a chronic spinal cord injury (SCI) population for the prevalence and prognostic significance of anemia (AN) and hypoalbuminemia (HA).
Setting:
The study was conducted at VA Boston Healthcare System, USA.
Methods:
A review of records of 322 SCI subjects (318 males) scheduled for annual examination was carried out for the period from 1998 to 2007. The number of follow-up years with AN (hematocrit <40%) or severe anemia (SAN) (hematocrit <30%) or HA (serum albumin <3 g%) was recorded for all subjects, divided between survivor and deceased subjects.
Results:
A total of 239 subjects survived to an average age of 60 and 30 years of paralysis and 83 subjects died at an average age of 70 and 27 years of paralysis (P<0.01 and P<0.06, respectively). The level and grade of paralysis were similar in these groups. The average prevalence rates of AN, SAN and HA were 34, 6 and 6% of survey years in the survivor group and 83, 18 and 22% in the deceased group; the respective ratios were 2.4, 3.0 and 3.7 (P<0.001). The fractions of survey years that were positive for SAN and/or HA among causes of death were sepsis, 42%; cancer, 33%; pulmonary failure 30%; cardiovascular disease, 25%; and undetermined causes, 9%. The mortality rate for the 95 subjects with a recurrence of SAN or HA was 40% within 3 years.
Conclusion:
The prevalence of AN, SAN and HA among chronic SCI subjects is high; repeated SAN and HA often precede death, particularly due to sepsis.
Similar content being viewed by others
Introduction
Anemia (AN) is common during the rehabilitation phase of spinal cord injury (SCI), chiefly due to blood loss and infection.1, 2 The infections implicated have been those of pressure sores or the urinary tract. The accompanying depression of serum iron-binding capacity and erythropoietin has further defined this anemia as the ‘anemia of inflammation’. AN might serve as a marker for infection in the acute SCI subject.
In addition, hypoalbuminemia (HA) has been observed with complications of SCI, which develops during sepsis and accompanys the anemia of inflammation.3, 4 Despite assumptions that this HA is due to malnutrition, intravenous infusion of nutrients has failed to raise the serum albumin in septic conditions.5 Furthermore, infusion of tracer albumin has shown a leak from the vascular system in subjects with SCI.6 This leak is demonstrable in paraplegia, increased by tetraplegia and maximized when SCI is complicated by infection.
Both AN and HA of acute SCI are reported as much less frequent at 1 year after SCI rehabilitation.7 There is a void in the documentation of the prevalence of AN and HA in the later years of SCI. As either AN or HA can serve as a marker for inflammation, often indicating infection, which is a common complication of SCI, a survey of these markers may be applicable to the care of SCI subjects. As infection is a common cause of death in SCI,8 these markers may have prognostic significance. And as both markers are routinely measured at the annual checkup examinations, which are offered at centers for continuing care of SCI, charting the course of these markers is feasible.
Methods
Subjects
Subjects who were followed up by the SCI service of this institution with scheduled annual checkups between 1998 and 2007 were reviewed. The baseline data recorded were cause of paralysis, level and motor completeness of paralysis (using the American Spinal Injury Impairment Scale) and the age and duration of paralysis of the subjects when last examined. For each checkup year, the hematocrit and serum albumin were measured. The lowest values for the year were noted. This notation included values recorded during acute illness that might have required hospitalization. AN was designated for any hematocrit of <40%. Severe anemia (SAN) was designated for a hematocrit of <30%. HA was designated for serum albumin values of <3.0 g%.
Any death during the survey period was recorded and the predominant medical condition leading to death was determined by record review. Deaths occurring 1 year beyond the survey period, that is, 2008, were added to expand the size of the deceased subject group and to better assess the prognostic value of AN, SAN and HA.
The causes of death were determined with the following conventions. Sepsis was assigned the cause of death in the event of terminal fever, whether associated with single-organ disease or with multiple-organ failure. Death was attributed to a single-organ failure with or without fever. Death associated with widespread cancer was attributed to cancer with or without fever. Although sepsis might have occurred without fever in some subjects who died, this was not assumed in any case.
Analysis
The cohort was divided into two groups—those surviving and those deceased through 2008. These groups were compared for age and the duration of paralysis using the t-test and were compared for level and grade of paralysis using the chi-square test.
The number of subjects and the number of survey years that were positive for AN, SAN and HA were compiled and compared between the deceased and survivor groups. The significance of differences between survivor and deceased subjects in the prevalence of each parameter was assessed using the chi-square test.
The year-to-year recurrence of SAN or HA or both appeared to be a poor prognostic sign. Therefore, the number of follow-up years survived by subjects without SAN or HA was compared with the number survived by subjects after a single year with SAN or HA and compared with subjects after a year with a repeated SAN or HA. Survival was expressed in percentage of subjects alive for each follow-up year.
The correlation of SAN and HA with the causes of death was calculated. The cause of death was ranked by the proportion of follow-up years that were positive for either SAN or HA. A contingency table was set up to calculate the significance of differences in these proportions. The chi-square test was applied.
Results
Subjects
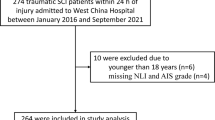
A total of 322 subjects (318 males and 4 females) were followed up at annual checkup during the survey period; 83 (26%) died during the survey period. The characteristics of the survivor and the deceased subjects differed chiefly in the older age and longer duration of paralysis of the deceased. Non-traumatic causes of paralysis were also more common among the deceased subjects (see Table 1).
Anemia (AN) and hypoalbuminemia (HA)
The proportion of surviving subjects who had experienced AN during the survey period was quite high, 72% of this group, but was even higher in the deceased group, 99%. The number of subjects with SAN or HA was also greater in the deceased (see Table 2).
The number of survey years positive for AN, SAN or HA was also high, occurring in consecutive or intermittent years throughout the course of annual checkups. The fraction of survey years positive for AN was 33% for survivors and 83% for deceased subjects. The fractions of survey years positive for SAN or HA were much lower, but once again higher for the deceased subjects (see Table 2). SAN and HA often occurred together in the same survey year, whether for survivors or for deceased subjects. The coincidence rate was 78%. The prevalence of either SAN or HA being lower than that of AN during the survey years suggested better discrimination between the survivor and the deceased subject groups by SAN or HA.
Repeated SAN and HA indicated a poor prognosis; 40% of subjects with a repeated SAN or HA in a follow-up years were dead within 3 years, many dying during the year of the repeated SAN or HA. This is in comparison with a survival of 99% of subjects without SAN or HA during 3 years of follow-up. The survival curves for these subjects are shown in Figure 1.
Severe anemia and HA were also tested as markers for the causes of death in this survey. On the basis of the prevalence of SAN and/or HA in the survey years for each subject, these markers were most often associated with death by sepsis and least often with death by unknown cause among the major causes (see Table 3).
Discussion
Although suggested by the earlier experience with acute SCI,1, 2 it is now documented that AN and HA are commonly found in chronic SCI. In addition, as previously suggested, AN and HA serve as markers, for the most part, of inflammation. The considerably greater prevalence of AN suggests, however, that it is a more sensitive marker of inflammation than HA. The sensitivity of this marker was not compared with other markers of inflammation, such as C reactive protein, fibrinogen or erythrocyte sedimentation rate. Nevertheless, the prevalence of inflammation implied by AN and HA is consistent with the clinical experience of recurrent infection in SCI care and sepsis as a major cause of death associated with SCI.8 A specificity for sepsis cannot be claimed, however, as other indicators of sepsis—hypothermia, change in white blood cell count and positive blood cultures9—were not surveyed, and other conditions, such as cancer and pulmonary or cardiovascular diseases, were also correlated with AN and HA.
Non-inflammatory causes of AN were not ruled out. History of blood loss—as from surgery, bleeding hemorrhoids or bleeding peptic ulcer—and laboratory data distinguishing the iron deficiency of blood loss from the iron sequestration of inflammation were not collected in this survey. Nevertheless, just as iron deficiency was doubted as the cause for 7% prevalence of anemia at 1 year after spinal cord injury,7 clinical experience did not suggest blood loss to explain the long-term prevalence of AN of 72% in the survivors of SCI reported in this study.
Alternative causes of HA are also uncommon. HA is often associated with portal hypertension in the general population. This condition does occur in the SCI population but not to the extent to explain the high prevalence of HA. Only one subject in this survey died of cirrhosis of the liver. Although another condition particularly associated with SCI, renal amyloidosis,10 might lead to glomerular damage and the nephrotic syndrome, a diagnosis of nephrotic syndrome was not found in the review of records of deceased subjects. Renal failure itself, with or without dialysis, causes HA (and AN as well).11 Only three subjects in this series were diagnosed with renal failure. The number of subjects with alternative explanations for HA is small.
The distinction between the survivors and the deceased subjects for inflammation was clearer when SAN and HA were taken as markers—AN being so common in both groups as to be less discriminating. The principal prognostic factor proved to be a repeated SAN or HA during the survey period. Many subjects (40%) with a repeated episode of SAN or HA died within 3 years, whereas very few subjects without SAN or HA died within the same time period.
It could be expected that the cause of death predicted by SAN and HA would be sepsis, and this expectation was supported by this review. However, other causes of death were also associated with these inflammatory markers—notably, cancer, cardiovascular disease and pulmonary failure. This is in keeping with the nonspecific association of other inflammatory markers with a variety of diseases, notably cancer and cardiovascular disease in non-SCI populations.12, 13
It might be asked whether AN and HA are causes or effects of infection and inflammation. The commonly noted rapid fall of the hematocrit and serum albumin with serious infections in clinical practice suggest that AN and HA are the result of the infection. However, resistance to infection might be impaired subsequently by volume depletion and reduced circulation, due to extravasation of albumin and by the reduced oxygen-carrying capacity of the anemia. As a practical matter, the onset of SAN and HA represents severe infection and inflammation, and persistent or recurrent SAN/HA suggests declining defenses against infection.
In the SCI experience, AN and HA, although nonspecific, are readily available markers of inflammation in routine practice. The occurrence of these markers at annual checkup, particularly repeated SAN or HA, should serve as indicators of health-threatening disease. If an infection is not apparent, the clinician might consider an occult abscess or cancer as potentially correctable causes.
Conclusion
Anemia is a common and sensitive marker for inflammation in the subjects with chronic paralysis due to SCI. SAN and HA are markers for more severe inflammation and for poor prognosis. These markers most strongly suggest an eventual death due to sepsis, renal failure, cancer, pulmonary disease or cardiovascular disease. As such, these markers may serve to focus efforts at detection and treatment of inflammatory complications of SCI.
References
Perkash A, Brown M . Anemia in patients with traumatic spinal cord injury. J Am Paraplegia Soc 1986; 9: 10–15.
Hirsh GH, Menard MR, Anton HA . Anemia after traumatic spinal cord injury. Arch Phy Med Rehabil 1991; 72: 195–201.
Scivoletto G, Fuoco U, Morganti B, Cosentino E, Molinari M . Pressure sores and blood and serum dysmetabolism in spinal cord injury patients. Spinal Cord 2004; 42: 473–476.
Wall BM, Mangold T, Huch KM, Corbett C, Cooke CR . Bacteremia in the chronic spinal cord injury population: risk factors for mortality. J Spinal Cord Med 2003; 26: 248–253.
Spiess A, Mikalunas V, Carlson S, Zimmer M, Craig RM . Albumin kinetics in hypoalbuminemic patients receiving total parental nutrition. J Parenter Enteral Nutr 1996; 20: 424–428.
Ring J, Seifert J, Lob G, Stephan W, Probst J, Brendel W . Elimination rate of human serum albumin in paraplegic patients. Paraplegia 1974; 12: 139–144.
Lipetz JS, Kirshblum SC, O’Connor KC, Voorman SJ, Johnston MV . Anemia and serum protein deficiencies in patients with traumatic spinal cord injury. J Spinal Cord Med 1997; 20: 335–340.
Rish BL, Dilustro JF, Salazar AM, Schwab KA, Brown HR . Spinal cord injury: a 25-year morbidity and mortality study. Mil Med 1997; 162: 141–148.
Silver JR, Martindale JH, Moulton A . Septicaemia–the forgotten complication of paraplegia. Paraplegia 1970; 8: 128–142.
Vaziri ND, Mirahmadi MK, Barton CH, Eltorai I, Gordon S, Byrne C et al. Clinicopathological characteristics of dialysis patients with spinal cord injury. J Am Paraplegia Soc 1983; 61: 3–6.
Galic G, Tomic M, Galesic K, Kvesic A, Solijic M, Mozetic V et al. Hypoalbuminemia and complication incidence in hemodialysed uremic patients. Coll Antropol 2009; 33: 559–566.
Cha CH, Park CJ, Cha YJ, Kim HK, Kim DM, Monghoon, Bae JH et al. Erythrocyte sedimentation rate measurements by TEST 1 better reflect inflammation than do those by the Westergren method in patients with malignancy, autoimmune disease, or infection. Am J Clin Pathol 2009; 131: 189–194.
Madjid M, Awan I, Willerson JT, Cassells SW . Leukocyte count and coronary heart disease: implications for risk assessment. J Am Coll Cardiol 2004; 44: 1945–1956.
Acknowledgements
This paper is the result of a study supported with resources and the use of facilities at the VA Boston Healthcare System, Boston, MA, USA. Funding was provided by the New England Chapter of the Paralyzed Veterans of America. Data collection was carried out by Elizabeth Tammaro.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Frisbie, J. Anemia and hypoalbuminemia of chronic spinal cord injury: prevalence and prognostic significance. Spinal Cord 48, 566–569 (2010). https://doi.org/10.1038/sc.2009.163
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2009.163
Keywords
This article is cited by
-
Incidence and risk factors of urinary tract infection in hospitalized patients with spinal cord injury in a hospital of China
Scientific Reports (2024)
-
Acute changes in antioxidants and oxidative stress to vigorous arm exercise: an intervention trial in persons with spinal cord injury and healthy controls
Spinal Cord Series and Cases (2023)
-
Serum albumin as a predictor of neurological recovery after spinal cord injury: a replication study
Spinal Cord (2021)