Abstract
Study design:
A case report to describe the minimally invasive technique of treating C1-type II odontoid combination fractures.
Objective:
To introduce a new, minimally invasive technique of triple anterior screw fixation for acute combination atlas–axis fractures.
Summary of background data:
Management for C1-type II odontoid combination fractures includes traction, immobilization and posterior fusion with and without instrumentation and anterior odontoid screw fixation. The combination of odontoid and bilateral transarticular C1–C2 anterior screw fixation is a recent addition in treating C1-type II odontoid fractures.
Methods:
A case of combination atlas-type II odontoid fracture occurred in a 39-year-old man. Imaging examinations showed a fracture of the unilateral anterior and posterior arch of C1 associated with type II odontoid fracture and with significant prevertebral soft tissue edema. Treatment consisted of odontoid and bilateral C1–C2 transarticular screw fixation through bilateral anterior small incisions.
Results:
The patient was mobilized early postoperatively with a hard cervical collar and discharged 4 days later. On 2-year follow-up, he presented no cervical complaints and only mild reduction in neck rotation.
Conclusion:
In case of C1-type II odontoid fracture, the triple anterior screw fixation can be taken into consideration as an alternative because of its superiority of minimal invasion, stability and safety.
Similar content being viewed by others
Introduction
Combined fractures of atlas and axis represent about 3% of all acute cervical spine injuries and most occur in the elderly resulting from a fall at home. There have been two reports of 92- and 85-year-old men with ‘triple’ anterior screw fixation technique.1, 2 We report the successful result obtained in a young patient affected by an acute combination atlas-type II odontoid fracture and treated with anterior odontoid and bilateral C1–C2 transarticular screw fixation.
Case report
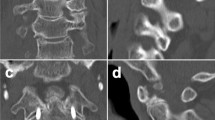
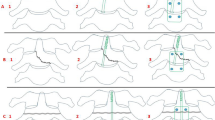
The patient was a 39-year-old man who fell from falsework, complaining of moderate neck pain and stiffness. On examination, he was awake and showed no neurological compromises. The cervical X-rays (Figures 1a and b), computed tomographical scan and sagittal reconstruction (Figures 2a and b), and magnetic resonance imaging (Figure 3) revealed a fracture of the unilateral anterior and posterior arch of C1 associated with type II odontoid fracture and with significant prevertebral soft tissue edema. Magnetic resonance imaging did not show a hyperintense area of the cervical cord in T2-weighted images. The patient was promptly treated with Gardner–Wells skull traction of 3 kg and reduction was obtained. About 72 h later, he was operated on under general anesthesia by nasotracheal intubation. Anterior odontoid screw fixation and bilateral transarticular C1–C2 fixation were performed under lateral and anteroposterior fluoroscopic guidance by G-arm. A radiolucent bite was placed in the patient's mouth to facilitate the open-mouth view.3 The patient was placed in a supine position, with the neck slightly extended. Medial to the right sternocleidomastoid muscle, at the level of C4–C5 space, an incision of 3 cm was made. A standard anterior blunt dissection was performed and the C2–C3 intervertebral disk was exposed. With fluoroscopic guidance, the proper trajectory was confirmed by placing the drill or similar instrument next to the neck, outside the incision. We placed a metal guide tube (5 mm diameter) through the incision and into the open surgical site at C2–C3 as an operating passage. The tip of the tube was docked at the C2 entry site (midpoint of C2 bottom). The K-wire was directed to the posterior superior tip of the odontoid process, monitored by fluoroscopy. After the K-wire was positioned satisfactorily, a 3.5 mm self-tapping cannulated screw with partial threads was placed over the K-wire. Care must be taken to avoid advancing the K-wire further as the insertion is performed. The screw length is usually 1–3 mm shorter than the actual measured length since some degree of compression of the C1-2 joint occurs with screw placement. A screw (3.6 cm length) was inserted in the dens. The drill entry point for the left transarticular screw was identified in the groove between the junction of C2 articular facet and vertebral body, which was 5 mm left of the midpoint of C2 vertebra bottom and adjacent to the odontoid screw. The K-wire was drilled with a lateral angulation of 20° relative to the sagittal plane and a posterior angulation of 15° relative to the coronal plane. It is crucial to ensure the K-wire passes through the center of C1–C2 lateral masses anteroposteriorly and into the center of C1 lateral masses laterally by G-arm monitoring, no matter which method of choosing the entry site and course direction. A left transarticular screw (3.8 cm length) was inserted over the K-wire. With this same technique, a left 3 cm horizontal incision was performed (Figure 4) and then a right transarticular screw (3.8 cm length) was inserted (Figures 5a and b). There were no surgery-related complications. The patient was discharged 4 days later and mobilized early with a hard cervical collar for 2 months. On 2-year follow-up, he presented no cervical complaints and only mild reduction in neck rotation. The right and left cervical rotation was about 50° individually, slightly more than 50% of normal values. Cervical X-rays (Figures 6a and b) showed the correct position of screws.
Discussion
Acute combination fractures of atlas and axis are more common in the elderly, in whom accidental falls are the primary cause. We report a young man whose mechanism of injury may be axial violence causing atlas fracture coupled with a flexion force causing odontoid fracture. There is no definitive class I or Class-α medical evidence regarding the management of this injury. All the published articles describe case series or reports that contained only Class-β evidence.4 The treatment goals are to achieve early maximal stability and minimal reduction in the range of motion. Management techniques for C1-type II odontoid combination fractures include semirigid immobilization (collar), traction followed by mobilization in a brace, rigid immobilization (halo, Minerva, SOMI), posterior fusion with and without instrumentation, and anterior odontoid screw fixation. Odontoid screw fixation combined with hard collar immobilization is used most commonly, provided the atlantal transverse ligament is intact. If a type II odontoid fracture is with an associated Jefferson fracture, or type II odontoid fracture with a ruptured transverse ligament, C1–C2 transarticular screw fixation is required.5
The combination of odontoid and bilateral transarticular C1–C2 anterior screw fixation is a recent addition in treating C1-type II odontoid fractures. When feasible, it ensures early maximal stability, even if it slightly reduces the mobility of C1–C2 complex.1 We apply this technique through two small cervical incisions, which differs from that of Apostolides et al.,2 who described a single approach through which three screws were placed.
Lots of reports have described the technique clinically and anatomically and mentioned the rare, if any, damage to the vertebral artery. Their findings are roughly alike. An anterior transarticular C1–C2 screw of 15–25 mm length can be inserted with a lateral angulation of 5–25° relative to the sagittal plane and a posterior angulation of 10–25° relative to the coronal plane.6 Generally speaking, the less distant the entry site from the midpoint of C2 vertebra bottom, the more inclination the course direction. The main advantage of this technique is that it can attain immediate stability of C1–C2 with a single surgical procedure, thereby avoiding the prone position for posterior fixation and possible injury to the cervical cord due to turning the body over and the resulting cervical instability. Moreover, there is less possibility of injuring the vertebral artery than in the posterior approach and it is as stable as posterior transarticular fixation.7 Its stability can be warranted if the screw is long enough to penetrate the axial vertebra and atlantal lateral mass where the bone density is high and if the transarticular anterior two screws course backward and outward, constituting a stable reverse triangle with the anteroinferior apex and posterosuperior basement. Hence, the constitution is capable of anti-rotation and anti-shearing. However, transarticular C1–C2 anterior screw fixation requires intact C1–C2 lateral masses and is still considered a salvage procedure for C1–C2 instability. Potential risks of this technique are damage to the vertebral artery (if screw trajectory is too lateral) and occipitocervical fusion (if screws are too long).2 We used a 3.8 cm screw and did not find any complications.
References
Agrillo U, Mastronardi L . Acute combination fracture of atlas and axis: ‘triple’ anterior screw fixation in a 92-year-old man: technical note. Surg Neurol 2006; 65: 58–62.
Apostolides PJ, Theodore N, Karahalios DG, Sonntag VK . Triple anterior screw fixation of an acute combination atlas–axis fracture. Case report. J Neurosurg 1997; 87: 96–99.
Chi YL, Wang XY, Xu HZ, Lin Y, Huang QS, Mao FM et al. Management of odontoid fractures with percutaneous anterior odontoid screw fixation. Eur Spine J 2007; 16: 1157–1164.
Section on Disorders of the Spine and Peripheral Nerves of the AANS and CNS. Guidelines for the management of acute cervical spine and spinal cord injuries. Chapter 18: management of combination fractures of the atlas and axis in adults. Neurosurgery 2002; 50 (Suppl): S140–S147.
Guiot B, Fessler RG . Complex atlantoaxial fractures. J Neurosurg 1999; 91 (2 Suppl): 139–143.
Lu J, Ebraheim NA, Yang H, Heck BE, Yeasting RA . Anatomic considerations of anterior transarticular screw fixation for atlantoaxial instability. Spine 1998; 23: 1229–1235.
Sen MK, Steffen T, Beckman L, Tsantrizos A, Reindl R, Aebi M . Atlantoaxial fusion using anterior transarticular screw fixation of C1–C2: technical innovation and biomechanical study. Eur Spine J 2005; 14: 512–518.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dean, Q., Jiefu, S., Jie, W. et al. Minimally invasive technique of triple anterior screw fixation for an acute combination atlas–axis fracture: case report and literature review. Spinal Cord 48, 174–177 (2010). https://doi.org/10.1038/sc.2009.108
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2009.108