Abstract
The goal of this study is to compare the construct stability of long segmental dorsal stabilization in unstable midthoracic osteoporotic fractures with complete pedicle screw cement augmentation (ComPSCA) versus restricted pedicle screw cement augmentation (ResPSCA) of the most cranial and caudal pedicle screws under cyclic loading. Twelve fresh frozen human cadaveric specimens (Th4–Th10) from individuals aged 65 years and older were tested in a biomechanical cadaver study. All specimens received a DEXA scan and computer tomography (CT) scan prior to testing. All specimens were matched into pairs. These pairs were randomized into the ComPSCA group and ResPSCA group. An unstable Th7 fracture was simulated. Periodic bending in flexion direction with a torque of 2.5 Nm and 25,000 cycles was applied. Markers were applied to the vertebral bodies to measure segmental movement. After testing, a CT scan of all specimens was performed. The mean age of the specimens was 87.8 years (range 74–101). The mean T-score was − 3.6 (range − 1.2 to − 5.3). Implant failure was visible in three specimens, two of the ComPSCA group and one of the ResPSCA group, affecting only one pedicle screw in each case. Slightly higher segmental movement could be evaluated in these three specimens. No further statistically significant differences were observed between the study groups. The construct stability under cyclic loading in flexion direction of long segmental posterior stabilization of an unstable osteoporotic midthoracic fracture using ResPSCA seems to be comparable to ComPSCA.
Similar content being viewed by others
Introduction
Cement augmentation of pedicle screws is one of the most effective strategies to improve pedicle screw stability in osteoporotic vertebral bodies1,2,3. However, the technique is associated with some serious complications. A 30-day mortality rate of almost 2% has been reported4. Thus, cement augmentation has to be critically questioned for each individual screw with regard to risks and benefits. This applies particularly to long segmental posterior stabilization, which provides a better load distribution compared to short segmental constructs2. Thereby, it can be assumed that the stress level at the screw-bone interface is greatest at the most cranial and most caudal screws. This represents the transition between the rigid instrumented and the freely flexible spine. For this reason, it can be presumed that restricted cementation of long segmental posterior stabilization limited to the most cranial and most caudal vertebrae may achieve comparable stability compared to complete pedicle screw cement augmentation. Restricting cement application can effectively reduce the complication rate. Additionally, it can help to decrease implant cost and surgery time.
Just recently, Spiegl et al.5 have found no differences in the maximum force between restricted pedicle screw augmentation and complete pedicle screw augmentation after long segmental stabilization of an unstable midthoracic fracture. The authors concluded that the construct stability of both strategies was comparable under static axial compression. However, this needed to be evaluated by cyclic biomechanical testing.
Based on this, a biomechanical study was performed to compare the construct stability between restricted pedicle screw augmentation and complete pedicle screw augmentation under cyclic loading. We hypothesized that there would be no significant differences between the two groups with respect to segmental movement and signs of screw loosening.
Materials and methods
Specimen preparation
Twelve fresh human donor spinal columns (Th4–Th10) were already examined in a previous study performing load of failure testing in flexion direction without visible implant failure or implant loosening in the CT performed after testing5. All donors originated from the Institute of Anatomy of the Leipzig University and had given written informed consent to dedicate their bodies to medical education and research purposes. According to the Saxonian Death and Funeral Act of 1994, this study is exempt from the need for approval by a registered ethics committee, however institutional approval for the use of the post-mortem tissues of human body donors was obtained prior to commencing this research. The authors declare that all experiments were performed according to the ethical principles of the Declaration of Helsinki. After computed tomography (CT) and dual-energy X-ray absorption (DEXA) measurements, the intact specimens were grouped into pairs according to gender, mineral bone density, and age. The first group represents the study group with restricted pedicle screw cement augmentation (ResPSCA), while the second group is the control group with complete pedicle screw cement augmentation (ComPSCA) (Table 1).
Soft tissues were dissected while preserving intervertebral discs, facet joints and ligament structures. Based on the CT scans, appropriate pedicle screw diameters and optimum screw lengths were determined. All pedicles of the levels Th5, Th6, Th8 and Th9 were instrumented transpedicularly using cannulated pedicle screws (M.U.S.T., Medacta Corporate, Switzerland) according to the manufacturer's specifications. This included the identification of the correct entry point, which was opened with a sharp awl, predrilling with a 2.5 mm drill bit, subsequent tapping, checking for intactness using a pedicle button, and insertion of the pedicle screws parallel to the cover plate with approximately 10° convergence. Cement augmentation of the pedicle screws was performed according to the previously defined groups. In the study group, cement augmentation was performed at the pedicle screws of the cranial (Th5) and caudal (Th9) level only (ResPSCA). All pedicle screws were cement augmented in the control group (ComPSCA). The bone cement (In. Medtronic, USA) was mixed and 1.0 ml of bone cement was applied slowly over each cemented cannulated screw using a cement application syringes. After curing of the bone cement, the cementing instruments were removed. Afterwards, two titanium rods were contoured to the coronary and sagittal alignment of the respective body donor and the rods were fixed to the pedicle screws according to the manufacturer's instructions. An unstable fracture was modeled by resection of a standardized ventral wedge of Th7 including the posterior cortex. For reproducibility, Kirschner wires were placed over a template to guide the osteotomy5.
The specimens were compressed axially and eccentrically by 20 mm. In a subsequent CT evaluation, no screw loosening and no damage to the spinal column structure was found5. All specimens were wrapped in plastic foil, cooled and shock frozen at − 80 °C to minimize ice crystal growth6.
For the current study, the specimens were then gently thawed. The temperature was gradually increased, for at least 2 days, to − 20 °C, then for one day to − 2 °C, then transitioned to room temperature within 16 h prior to testing. This is intended to reduce the temperature gradient within the specimen during thawing and to protect the tissues.
Experimental procedure
The non-instrumented vertebrae Th4 and Th10 were embedded with a polyurethane casting resin (RenCast; Huntsman Advanced Materials, Basel, Switzerland). Additional screws were inserted into the vertebral bodies to improve the bond between the bone and embedding. The vertebral endplate of Th7 was positioned horizontally to ensure an upright alignment of the spine.
The specimens were clamped in a test stand developed in-house (Fig. 1a). The major component is a swivel arm that is driven by a motor, generating a defined torque. The specimens were fixed with the lower embedding on a slide, while the upper embedding was connected to the swivel arm. The rotation axis of the swivel arm was set to the center of the fracture gap in Th7 (Fig. 1b). In order to generate torque as straight as possible into the spinal column, the specimen was not fully constrained (Fig. 1a). The slide allowed lateral movements while forward and backward movements were suppressed. The upper embedding was connected via a bearing rod to a linear bearing in the swivel arm. This enabled rotation and axial compensatory movements of the spinal column. The linear bearing was, in turn, pivotally mounted in the swivel arm. Thereby, mainly torque in the flexion/extension direction was introduced, whereas pure transverse forces were minimized.
Experimental set-up: (a) test stand: a torque around the axis of the swivel arm (red line) is introduced into the specimen via the motor (M), the blue arrows represent the degrees of freedom of the clamped specimen; (b) Markers with speckle patterns are applied to the instrumented vertebral bodies (Th5, Th6, Th8 and Th9), the swivel arm (sam) and a reference marker (rm). In addition, a positioning aid (pa) for aligning the axis of rotation to the fracture gap is shown.
Markers with speckle patterns were pinned to the instrumented vertebral bodies (Fig. 1). The pins were pinned into the vertebral body. Care was taken to ensure that they were far away from the screw tips and the surrounding cement, which was introduced after carefully evaluating the CT scan after compressive testing. Markers were also attached to the swivel arm, as well at an independent reference point.
The specimens were periodically bent in the direction of flexion. A torque of 2.5 Nm was applied, as recommended in osteoporotic thoracic spines7. A total of 25,000 load cycles were applied, which corresponds to the expected motion within the first 3–4 weeks after surgery in a geriatric patient population8. Tests were carried out at a frequency of 1.2 Hz. During a load cycle, the load was applied in the first half and released in the second half. The specimens were kept moist throughout the testing period, being wrapped in moist gauzes that were regularly moistened7. The rotation of the swivel arm was measured with an angle sensor (Incremental encoder 5821, Fritz Kübler GmbH, Germany). Furthermore, the positions of the markers were recorded with a digital image correlation system with a three-camera setup (Q400, LIMESS Messtechnik und Software GmbH, Krefeld, Germany)9. These measurements were taken at the beginning (10 cycles), every 500 cycles and at the end (24,990 cycles) for continuous monitoring. Two cycles were recorded with a frame rate of 15 Hz for each individual measurement time-point.
Evaluation
After cyclic loading, CT was performed in order to detect any signs of implant failure, screw loosening or subsequent vertebral fractures. These were evaluated independently by two of the authors, one spine surgeon (U.J.S.) and one radiologist (M.R.).
As the markers are anchored into vertebral bodies, it is assumed that they represent the movement of the vertebral bodies during loading9. The marker positions measured with the digital image correlation system were correlated and exported into a coordinate system corresponding to a person standing upright. An evaluation routine was developed to calculate the relative movement between two markers. Since torque was introduced, the evaluation was limited to the relative rotation of the vertebral bodies. In order to calculate these rotational components about a respective axis of the coordinate system, one vector defined by two speckle pattern points on each marker, respectively, was regarded. When selecting these points, it was ensured that the resulting vector was preferably perpendicular to the respective rotation axis prior to loading. For all three axes of the coordinate system, the projection of the respective vector into the plane perpendicular to the respective axis was regarded. The angles between two vector projections of different markers were calculated for each time step. Thus, relative rotation depending on the regarded axis could be calculated for any pair of markers. The calculation was done using MATLAB (MathWorks and Simulink, USA).
The relative rotations between the swivel arm and the reference marker were compared with the data from the angle sensor to check the continuity of the measurements (Supplement). The relative rotations between the adjacent vertebrae Th5/Th6 and Th8/Th9 and between the vertebra pairs Th5/Th9 and Th6/Th8 were evaluated. For each time interval of a series of measurements, the peak-to-peak amplitude and the zero offset to the rest position were determined. In the course of the measurement, the part of the movement characterized by the peak-to-peak amplitude was regarded as reversible. A non-reversible part was indicated by the difference between the zero offset and the rest position of the first time interval. This was subsequently defined as permanent deflection (Supplement). The determined permanent deflections and peak-to-peak amplitudes were considered separately and examined in the course of the 25,000 cycles.
The statistical analysis was performed with SPSS 24.0 (IBM, USA). The Shapiro–Wilk test was used to verify normal distribution. Mean differences were checked with the Student t-test for normally distributed data pairs, otherwise the Mann–Whitney test was used. A value of p < 0.05 was considered significant.
Results
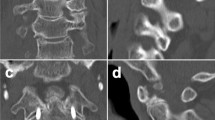
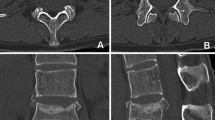
Evaluation of the CT images showed loosening of pedicle screws in three specimens, including screw loosening in one specimen of the study group (Fig. 2a–c). Thereby, a cut-out of the right pedicle screw in Th8 and some signs of loosening of the right augmented pedicle screw in Th9 of specimen ResPSCA 1 were visible (Fig. 2b). In the control group, screw loosening was observed in two specimens. Screw cuts out of the right pedicle screws in Th9 could be seen in ComPSCA 2 and ComPSCA 5 (Fig. 2c).
CT scans after cyclic loading are illustrating one of five cases with ResPSCA, without any signs of screw loosening or implant failure (a), one specimen with cut-out of the right pedicle screw in Th8 (big arrow) and signs of loosening of the right cement-augmented pedicle screw in Th9 (b, small arrows). In (c), one of two specimens is shown with a cut-out of the right cement-augmented pedicle screw of Th9 after ComPSCA (arrow).
In all specimens, mainly relative rotations around the transverse axis were observed, on which the assessment focuses. The marker in Th5 of the specimen ComPSCA 2 protruded slightly into the disc. Based on a potential effect on the measurements, this marker was not taken into account in the assessment. During loading, no pronounced periodic movement between the adjacent vertebral bodies was observed. In the course of the measurements over all specimens, no abrupt changes were detected, which would have indicated premature failure. For this reason, only cycles 10, 5,000, 10,000, 15,000, 20,000 and 24,990 were evaluated.
In Fig. 3, box plots of the peak-to-peak amplitudes between Th6 and Th8, at the beginning and end of the measurements, of both study groups are shown. Statistically, there were no differences in the mean values of the peak-to-peak amplitudes between the beginning and the end of testing in between the groups (p = 0.67 for ResPSCA, p = 0.83 for ComPSCA), as well as between both groups (p = 0.73 for cycle 10 between ResPSCA and ComPSCA, p = 0.53 for cycle 24,990 between ResPSCA and ComPSCA).
Comparison of the peak-to-peak amplitudes between Th6 and Th8 at the beginning (cycle 10) and end (cycle 24,490) of the testing for restricted cement augmentation (ResPSCA) and complete cement augmentation (ComPSCA). Statistically, there are no differences in the mean values of the peak-to-peak amplitudes between the beginning and the end of testing in between a group (p = 0.67 for ResPSCA, p = 0.83 for ComPSCA) and in the direct comparison between both groups (p = 0.73 for cycle 10 between ResPSCA and ComPSCA, p = 0.53 for cycle 24,490 between ResPSCA and ComPSCA).
Figure 4 compares the mean values of the calculated permanent deflections and peak-to-peak amplitudes for both test groups with complete (ComPSCA) and restricted cement augmentation (ResPSCA). For each of the vertebral body pairs the course of the measured values between the two comparison groups appeared to be qualitatively and quantitatively similar. This finding is supported by the fact that, for each data pair between the ResPSCA and ComPSCA groups, the mean values were examined and no statistically significant differences were found (Table 2).
Comparison of the mean values of the test groups with complete (ComPSCA) and restricted cement augmentation (ResPSCA) with regard to permanent deflection (above) and peak-to-peak amplitude (below). No statistically significant differences were found when comparing any pair of data for the ResPSCA and ComPSCA groups. To make the error bars more visible, the dots have been slightly shifted. However, the measured values refer to the cycle indicated on the abscissa.
Figure 5 compares the two test groups. In each case, the permanent deflections and peak-to-peak amplitudes of the comparison pairs Th5/Th6, Th6/Th8 and Th8/Th9 are considered. In most cases, the permanent deflections of Th5/Th6 and Th8/Th9 were small and comparatively smaller than those between Th6/8, with the exception of ResPSCA 1, ComPSCA 2 and ComPSCA 5, respectively. In all of those three specimens, implant failure was visible. The peak-to-peak amplitudes of Th5/Th6 and Th8/Th9 were significantly smaller than those of Th6/Th8, but the differences were less obvious in the specimens ResPSCA 1, ResPSCA 6, ComPSCA 4, and ComPSCA 5.
Discussion
The most important finding of this article is the comparable construct stability between ComPSCA and ResPSCA with two cases of cut-outs in the ComPSCA group and only one in the ResPSCA group under cyclic testing, despite the fact that biomechanical testing under axial loading was done previously in all specimens. The dynamic testing results confirm these three cases of implant failure. Hereby, the orientation of two vertebrae has changed permanently during the course of cyclic loading, which can be interpreted as a sign of screw loosening. However, based on the fact that only a one-sided screw cut-out was seen in all three cases, with signs of implant failure and macroscopically uneventful contralateral screw positioning, no higher grades of instability can be expected. This is in accordance with our results, with consistent but only subtle differences in segmental movement between the three specimens with implant failure in comparison to the others.
Otherwise the peak-to-peak amplitudes of movement were in accordance with the expected results. Minimal to low peak-to-peak amplitudes were recorded in the stabilized healthy segments Th5/Th6 and Th8/Th9. In contrast, moderate to high peak-to-peak amplitudes were seen between Th6/Th8, which represents the stabilized unstable fracture region. Generally, the ranges of peak-to-peak amplitudes between the specimens were large without any significant differences between the study groups. This seems to be not very surprising considering the rather small study group and the big range of ages in patients and the morphological differences between the spines. However, both study groups were matched regarding patient age, bone density and gender in order to minimize the differences between the groups.
Interestingly, two of the specimens with implant failure were highly osteoporotic, with T-scores of less than -4 (two cases). The third specimen had spondylitis ancylosans. Several authors recommend long segmental stabilization with pedicle screw implantation of three levels above and below the fracture in patients with spondylitis ancylosans10,11. This can partially explain the implant failure. However, all implant failure happened to be below the fracture. This is somewhat surprising, as in daily practice screw cut-outs seem to occur more frequently in the instrumented vertebral bodies above the fracture in correspondence to the data reported by Banno et al.12. In contrast, other studies reported observed higher rates of screw loosening at the lowest level of instrumentation13. Generally, the huge majority of implant failure occurs at the lowest or highest level of instrumentation12,13. Additionally, all cut-outs were one-sided. This can be explained by the fact that the cascade of implant failure has just begun. This might end in screw cut-outs of both pedicle screws, leading to higher instabilities in the further course.
Generally, specimens tended to adopt a proceeding kyphotic malposition during the course of testing due to cyclic loading of 25,000 cycles predominantly in the flexion direction. The permanent deflection was expected based on cyclic loading without protective interactions of the muscle and rib cage due to permanent strain on the connective tissues. Generally, 25,000 cycles represent the average load during all day activities over a period of 3–4 weeks for elderly people8. This number of cycles was chosen to simulate this very important period of bony healing. In correspondence to that, increased in vivo stiffness has been observed to begin 3 weeks after osteotomy in an ostoporotic sheep model14. In addition, fatigue tests should be conducted in follow-up studies to evaluate the long-term behavior of the stabilization. Thus, the load acting on the material can be supposed to be higher as compared to clinical practice. The selected bending moment of 2.5 Nm is based on a literature recommendation for range of motion tests on osteoporotic thoracic spines as maximal loads in order not to destroy tissues7. In vivo tests of the more heavily loaded lumbar spine measured 3.5 (± 1.5) Nm when bending the upper body and 4.2 (± 1.7) Nm when lifting a weight from the floor15. On the one hand, significantly lower loads are assumed to be in the area of the middle thoracic spine. On the other hand, upper body flexion and weight lifting are extreme loads that should be avoided postoperatively. By performing cyclic testing over an estimated period of 3 to 4 weeks and applying high cyclic loads, a model was chosen that simulates an extreme situation without any stabilizing effect that would be expected in living patients as a part of the fracture healing process.
When evaluating the relative movement between the individual vertebral bodies, indications of screw loosening were found, but there were no clear patterns. An indirect measuring method was chosen, which allows for continuous observation. In order to measure screw movement in the vertebral body directly, markers would have to be attached to the screw tip or shaft. This would require the removal of bone material, which would have a lasting effect on screw retention. This was not the intention of the study, but should be investigated in subsequent studies.
However, the study has several limitations. First of all, all specimens were previously tested in a load of failure manner by axial compression. Thereby, implant failure particularly screw cut-out or screw loosening could be excluded by CT examination after testing5. A large part of the deformation was elastically stored in the rod system through the fracture gap. Despite the fact that it is not possible to definitely exclude minor lesions, only a minority of specimens showed signs of implant failure. Generally, all specimens had a similar load history and were appropriate for a comparative study. Secondly, another freezing and thawing cycle can influence the mechanical properties of soft tissue negatively16. However, the influence on the mechanical properties of bone tissue seems to be not relevant17,18. Furthermore, only minor effects on the range of motion of functional spine units have been observed19. In a further study, several freezing and thawing cycles were examined. No significant alterations in the range of motion could be seen after the initial freezing during further freeze–thaw cycles20. In addition, the samples were frozen in a tissue-friendly manner6. As the samples have the same storage history, comparative studies are permissible. In addition, the study focuses on the screw anchorage in the bone. The relevant vertebral bodies are rigidly instrumented. The freely movable segments, on which alterations of the intervertebral discs and ligaments would have a greater impact, were not the focus of this study. For the reasons mentioned above, a comparative study with the specimens is permissible, even though they have already undergone initial testing. Since all specimens were always treated in the same way, comparability is ensured. In addition, the usual recommendations were followed for storage, test duration, moisture retention, load rates, etc.7,21,22. Additionally, the cyclic loading was performed in flexion only. In contrast, human spines are subjected to multiple different loadings in different directions, all of which contribute to the development of implant failure. Thereby, the midthoracic spine is particularly susceptible under flexion with lower flexion strength than compressive strength23. Furthermore, it was not possible to generate pure torque only. However, the test set-up applies a uniform torque in the direction of flexion in a reproducible manner, which ensures comparability. Additionally, our sample size was small (six spines in each group) and underpowered. A post-hoc analysis has shown that at least 80 speciment per group are necessary to gain a power of 80%. However, compared with related publications, our study had a similar number of specimens per group24,25,26,27 and complies with the recommendations for in vitro testing with human donor material20. Thereby, the analysis of group differences can be misleading based on the low power. Nevertheless, there were two implant failures visible in the ComPSCA group and only one in the ResPSCA group. Additionally, matching of the groups was performed in accordance to the T-score, age, and gender of the specimen. Next, the anatomic model represents a simplified model not considering the rib cage (leading to a decrease in stiffness), the muscle, and the physiological body weight acting on the midthoracic cage28,29. Last but not least, we did not include a non-cemented group in order to prove that cement-augmented pedicle screw augmentation is superior in our testing scenario. This was done based on the moderate to good biomechanical evidence of the superiority cement-augmented screw hold in osteoporotic bone30,31. Based on this evidence and the clinical experience of the last decade the authors hardly ever perform posterior stabilization without cement-augmented pedicle screws in osteoporotic vertebral body fractures. Generally, only clinical studies are conclusive for the evaluation of screw loosening in everyday life. Therefore, clinical studies are warranted to compare implant failure and reduction loss between restricted and complete pedicle screw augmentation in long segmental posterior stabilization.
Conclusion
No statistically significant differences in both implant failure rate and peak-to-peak amplitudes of movement between the instrumented vertebral bodies could be seen between the ResPSCA and ComPSCA groups under cyclic loading. Thus, the construct stability of long segmental posterior stabilization of an unstable osteoporotic midthoracic fracture using ResPSCA seems to be comparable to ComPSCA.
References
A Saman El A Kelm S Meier AL Sander K Eichler I Marzi H Laurer 2013 Intraoperative PEEP-ventilation during PMMA-injection for augmented pedicle screws: Improvement of leakage rate in spinal surgery Eur. J. Trauma Emerg. Surg. 39 461 468 https://doi.org/10.1007/s00068-013-0319-x
S Hoppe Y Loosli D Baumgartner P Heini L Benneker 2014 Influence of screw augmentation in posterior dynamic and rigid stabilization systems in osteoporotic lumbar vertebrae: A biomechanical cadaveric study Spine (Phila Pa 1976) 39 E384 389 https://doi.org/10.1097/BRS.0000000000000198
SC Yang PH Liu YK Tu 2018 Pullout evaluation of sawbone experiment in different types of pedicle screws combined with bone cement augmentation for severe osteoporotic spine Acta Bioeng. Biomech. 20 55 64
I Janssen YM Ryang J Gempt S Bette J Gerhardt JS Kirschke B Meyer 2017 Risk of cement leakage and pulmonary embolism by bone cement-augmented pedicle screw fixation of the thoracolumbar spine Spine J. 17 837 844 https://doi.org/10.1016/j.spinee.2017.01.009
UJ Spiegl M Weidling S Schleifenbaum M Reinhardt CE Heyde 2020 Comparison of long segmental dorsal stabilization with complete versus restricted pedicle screw cement augmentation in unstable osteoporotic midthoracic vertebral body fractures: A biomechanical study World Neurosurg. 143 e541 e549 https://doi.org/10.1016/j.wneu.2020.08.002
H Steinke 2001 Plastinated body slices for verification of magnetic resonance tomography images Ann. Anat. Anatomischer Anzeiger 183 275 281 https://doi.org/10.1016/S0940-9602(01)80234-X
HJ Wilke K Wenger L Claes 1998 Testing criteria for spinal implants: recommendations for the standardization of in vitro stability testing of spinal implants Eur. Spine J. 7 148 154
HJ Wilke U Mehnert LE Claes MM Bierschneider H Jaksche BM Boszczyk 2006 Biomechanical evaluation of vertebroplasty and kyphoplasty with polymethyl methacrylate or calcium phosphate cement under cyclic loading Spine (Phila Pa 1976) 31 2934 2941 https://doi.org/10.1097/01.brs.0000248423.28511.44
M Weidling C Voigt T Wendler M Heilemann M Werner JS Jarvers CE Heyde 2019 Kinematics of the lumbo-pelvic complex under different loading conditions Curr. Direct. Biomed. Eng. 5 347 350 https://doi.org/10.1515/cdbme-2019-0087
NH Hoh von der J Henkelmann JS Jarvers UJA Spiegl A Voelker C Josten CE Heyde 2020 Magnetic resonance tomography for the early detection of occult fractures of the spinal column in patients with ankylosing spondylitis Eur. Spine J. 29 870 878 https://doi.org/10.1007/s00586-020-06309-7
T Caron R Bransford Q Nguyen J Agel J Chapman C Bellabarba 2010 Spine fractures in patients with ankylosing spinal disorders Spine (Phila Pa 1976) 35 E458 464 https://doi.org/10.1097/BRS.0b013e3181cc764f
T Banno T Hasegawa Y Yamato S Kobayashi D Togawa S Oe Y Mihara K Kurosu N Yamamoto Y Matsuyama 2018 Assessment of the change in alignment of fixed segment after adult spinal deformity surgery Spine 43 262 269 https://doi.org/10.1097/BSD.0000000000000480
L Yuan X Zang Y Zeng Z Chen W Li 2021 Incidence, risk, and outcome of pedicle screw loosening in degnerative lumbar scoliosis patients undergoing long-segment fusion Glob. Spine J. https://doi.org/10.1177/21925682211017477
CA Lill J Hesseln U Schlegel C Eckhardt J Goldhahn E Schneider 2003 Biomechanical evaluation of healing in a non-critical defect in a large animal model of osteoporosis J. Orthop. Res. 21 836 842 https://doi.org/10.1016/S0736-0266(02)00266-8
A Rohlmann D Pohl A Bender F Graichen J Dymke H Schmidt G Bergmann 2014 Activities of everyday life with high spinal loads PLoS ONE 9 e98510 https://doi.org/10.1371/journal.pone.0098510
F Gottsauner-Wolf JJ Grabowski EY Chao KN An 1995 Effects of freeze/thaw conditioning on the tensile properties and failure mode of bone-muscle-bone units: A biomechanical and histological study in dogs J. Orthop. Res. 13 90 95 https://doi.org/10.1002/jor.1100130114
F Linde HC Sorensen 1993 The effect of different storage methods on the mechanical properties of trabecular bone J. Biomech. 26 1249 1252 https://doi.org/10.1016/0021-9290(93)90072-m
ED Sedlin 1965 A rheologic model for cortical bone. A study of the physical properties of human femoral samples Acta Orthop. Scand. Suppl. Suppl. 83 81 77 https://doi.org/10.3109/ort.1965.36.suppl-83.01
MM Panjabi M Krag D Summers T Videman 1985 Biomechanical time-tolerance of fresh cadaveric human spine specimens J. Orthop. Res. 3 292 300 https://doi.org/10.1002/jor.1100030305
M Hongo RE Gay JT Hsu KD Zhao B Ilharreborde LJ Berglund KN An 2008 Effect of multiple freeze-thaw cycles on intervertebral dynamic motion characteristics in the porcine lumbar spine J. Biomech. 41 916 920 https://doi.org/10.1016/j.jbiomech.2007.11.003
HJ Wilke B Jungkunz K Wenger LE Claes 1998 Spinal segment range of motion as a function of in vitro test conditions: Effects of exposure period, accumulated cycles, angular-deformation rate, and moisture condition Anat. Rec. 251 15 19 https://doi.org/10.1002/(SICI)1097-0185(199805)251:1<15::AID-AR4>3.0.CO;2-D
MM Panjabi 1988 Biomechanical evaluation of spinal fixation devices: I. A conceptual framework Spine (Phila Pa 1976) 13 1129 1134
JM Buckley CC Kuo LC Cheng K Loo J Motherway C Slyfield V Deviren C Ames 2009 Relative strength of thoracic vertebrae in axial compression versus flexion Spine J. 9 478 485 https://doi.org/10.1016/j.spinee.2009.02.010
KM Kebaish CT Martin JR O'Brien IE LaMotta GD Voros SM Belkoff 2013 Use of vertebroplasty to prevent proximal junctional fractures in adult deformity surgery: A biomechanical cadaveric study Spine J. 13 1897 1903 https://doi.org/10.1016/j.spinee.2013.06.039
M Kayanja K Evans R Milks IH Lieberman 2006 The mechanics of polymethylmethacrylate augmentation Clin. Orthop. Relat. Res. 443 124 130 https://doi.org/10.1097/01.blo.0000200243.60426.57
MM Kayanja R Schlenk D Togawa L Ferrara I Lieberman 2006 The biomechanics of 1, 2, and 3 levels of vertebral augmentation with polymethylmethacrylate in multilevel spinal segments Spine (Phila Pa 1976) 31 769 774 https://doi.org/10.1097/01.brs.0000207466.40955.31
MJ Kim DP Lindsey M Hannibal TF Alamin 2006 Vertebroplasty versus kyphoplasty: Biomechanical behavior under repetitive loading conditions Spine (Phila Pa 1976) 31 2079 2084 https://doi.org/10.1097/01.brs.0000231714.15876.76
C Liebsch N Graf K Appelt HJ Wilke 2017 The rib cage stabilizes the human thoracic spine: An in vitro study using stepwise reduction of rib cage structures PLoS ONE 12 e0178733 https://doi.org/10.1371/journal.pone.0178733
EM Mannen JT Anderson PM Arnold EA Friis 2015 Mechanical contribution of the rib cage in the human cadaveric thoracic spine Spine (Phila Pa 1976) 40 E760 766 https://doi.org/10.1097/BRS.0000000000000879
D Liu J Sheng H-H Wu X Kang Q-Y Xie Y Luo J-J Zhou W Zheng 2018 Biomechanical study of injectable hollow pedicle screws for PMMA augmentation in severely osteoporotic lumbar vertebrae: Effect of PMMA distribution and volume on screw stability J. Neurosurg. Spine 29 639 646 https://doi.org/10.3171/2018.4.SPINE171225
T Karius C Deborre DC Wirtz C Burger A Prescher A Fölsch K Kabir R Pflugmacher H Goost 2017 Radiofrequency-activated PMMA-augmentation through cannulated pedicle screws: A cadaver study to determine the biomechanical benefits in the osteoporotic spine Technol. Health Care 25 327 342 https://doi.org/10.3233/THC-161273
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
U.S. had the study idea. U.S., M.W., S.S., and C.E.H. developed the study design, M.W. and V.N. performed the main testing, R.H., M.H., and T.W. supported the testing. U.S. and M.R. evaluated the CT separately. U.S. and M.W. wrote the manuscript text and developed the figures and tables, All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
Material supply for biomechanical testing: all authors: Fa. Medacta Heyde: Royalties Fa. Medacta.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Spiegl, U.J., Weidling, M., Nitsch, V. et al. Restricted cement augmentation in unstable geriatric midthoracic fractures treated by long-segmental posterior stabilization leads to a comparable construct stability. Sci Rep 11, 23816 (2021). https://doi.org/10.1038/s41598-021-03336-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-03336-2
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.